Sandbox:Amd: Difference between revisions
Jump to navigation
Jump to search
| Line 66: | Line 66: | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |N | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |N | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |Abnormal [[LFT]] | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* Abnormal [[LFT]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |Ultrasound shows [[biliary]] dilatation/stents/tumor | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |Ultrasound shows [[biliary]] dilatation/stents/tumor | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |Biliary drainage ([[Endoscopic retrograde cholangiopancreatography|ERCP]]) + IV antibiotics | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |Biliary drainage ([[Endoscopic retrograde cholangiopancreatography|ERCP]]) + IV antibiotics | ||
| Line 96: | Line 97: | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |N | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |N | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |Increased [[amylase]] / [[lipase]] | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* Increased [[amylase]] / [[lipase]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |Ultrasound shows evidence of [[inflammation]] | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |Ultrasound shows evidence of [[inflammation]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |Pain radiation to back | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |Pain radiation to back | ||
| Line 110: | Line 112: | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |− | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |− | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |N | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |N | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |Increased AMA level, abnormal [[LFTs]] | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* Increased AMA level, abnormal [[LFTs]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
| Line 145: | Line 148: | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |N to hyperactive for dislodged stone | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |N to hyperactive for dislodged stone | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |[[Leukocytosis]] | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* [[Leukocytosis]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |Ultrasound shows [[gallstone]] | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |Ultrasound shows [[gallstone]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |[[Murphy's sign|Murphy’s sign]] | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |[[Murphy's sign|Murphy’s sign]] | ||
| Line 222: | Line 226: | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |WBC> 10,000 | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* WBC> 10,000 | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |Air under [[diaphragm]] in upright [[CXR]] | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |Air under [[diaphragm]] in upright [[CXR]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
| Line 237: | Line 242: | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |Hypoactive | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |Hypoactive | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |[[Leukocytosis]] | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* [[Leukocytosis]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |Ultrasound shows evidence of [[inflammation]] | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |Ultrasound shows evidence of [[inflammation]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |[[Nausea and vomiting|Nausea & vomiting]], [[decreased appetite]] | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |[[Nausea and vomiting|Nausea & vomiting]], [[decreased appetite]] | ||
| Line 251: | Line 257: | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |Hypoactive | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |Hypoactive | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |[[Leukocytosis]] | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* [[Leukocytosis]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |CT scan and ultrasound shows evidence of inflammation | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |CT scan and ultrasound shows evidence of inflammation | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
| Line 394: | Line 401: | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |'''−''' | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |'''−''' | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |[[RUQ]] | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |[[RUQ]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |± | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + in liver failure leading to varices | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | + in liver failure leading to varices | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |'''−''' | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |'''−''' | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |'''−''' | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |'''−''' | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |N | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
*Elevated [[Aspartate aminotransferase|serum aspartate aminotransferase]] and [[alanine aminotransferase]] levels may be more than five times the upper limit of the normal range. | |||
*Elevated serum [[alkaline phosphatase]] and [[Bilirubin|bilirubin levels]], decreased [[Albumin|serum albumin level]]. | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
| Line 414: | Line 423: | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |− | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |− | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |− | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |− | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |>60% TS | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | | ||
* >60% TS | |||
* >240 μg/L SF | |||
* Raised LFT <br>Hyperglycemia | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |Ultrasound shows evidence of cirrhosis | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |Ultrasound shows evidence of cirrhosis | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |Extra intestinal findings: | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |Extra intestinal findings: | ||
| Line 671: | Line 683: | ||
{| | {| | ||
|- | |- | ||
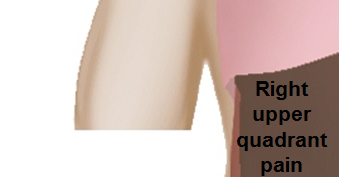
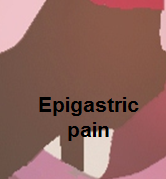
| <figure-inline class="mw-default-size"><figure-inline><figure-inline><figure-inline>[[Image:Right_upper_quadrant.PNG|link=Right upper quadrant abdominal pain resident survival guide|339x339px]]</figure-inline></figure-inline></figure-inline></figure-inline>||<figure-inline class="mw-default-size"><figure-inline><figure-inline><figure-inline>[[Image:Epigastric_quadrant_pain.PNG|link=Epigastric pain resident survival guide|179x179px]]</figure-inline></figure-inline></figure-inline></figure-inline>||<figure-inline class="mw-default-size"><figure-inline><figure-inline><figure-inline>[[Image:Left_upper_quadrant.PNG|link=Left upper quadrant abdominal pain resident survival guide|329x329px]]</figure-inline></figure-inline></figure-inline></figure-inline> | | <figure-inline class="mw-default-size"><figure-inline><figure-inline><figure-inline><figure-inline>[[Image:Right_upper_quadrant.PNG|link=Right upper quadrant abdominal pain resident survival guide|339x339px]]</figure-inline></figure-inline></figure-inline></figure-inline></figure-inline>||<figure-inline class="mw-default-size"><figure-inline><figure-inline><figure-inline><figure-inline>[[Image:Epigastric_quadrant_pain.PNG|link=Epigastric pain resident survival guide|179x179px]]</figure-inline></figure-inline></figure-inline></figure-inline></figure-inline>||<figure-inline class="mw-default-size"><figure-inline><figure-inline><figure-inline><figure-inline>[[Image:Left_upper_quadrant.PNG|link=Left upper quadrant abdominal pain resident survival guide|329x329px]]</figure-inline></figure-inline></figure-inline></figure-inline></figure-inline> | ||
|- | |- | ||
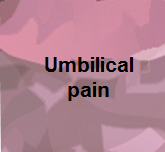
| <figure-inline class="mw-default-size"><figure-inline><figure-inline><figure-inline>[[Image:Right_flank_quadrant.PNG|link=Right flank pain resident survival guide|338x338px]]</figure-inline></figure-inline></figure-inline></figure-inline>||<figure-inline class="mw-default-size"><figure-inline><figure-inline><figure-inline>[[Image:Umbilical_pain.PNG|link=Umbilical region pain resident survival guide|165x165px]]</figure-inline></figure-inline></figure-inline></figure-inline>||<figure-inline class="mw-default-size"><figure-inline><figure-inline><figure-inline>[[Image:Left_flank_quadrant.PNG|link=Left flank quadrant abdominal pain resident survival guide|335x335px]]</figure-inline></figure-inline></figure-inline></figure-inline> | | <figure-inline class="mw-default-size"><figure-inline><figure-inline><figure-inline><figure-inline>[[Image:Right_flank_quadrant.PNG|link=Right flank pain resident survival guide|338x338px]]</figure-inline></figure-inline></figure-inline></figure-inline></figure-inline>||<figure-inline class="mw-default-size"><figure-inline><figure-inline><figure-inline><figure-inline>[[Image:Umbilical_pain.PNG|link=Umbilical region pain resident survival guide|165x165px]]</figure-inline></figure-inline></figure-inline></figure-inline></figure-inline>||<figure-inline class="mw-default-size"><figure-inline><figure-inline><figure-inline><figure-inline>[[Image:Left_flank_quadrant.PNG|link=Left flank quadrant abdominal pain resident survival guide|335x335px]]</figure-inline></figure-inline></figure-inline></figure-inline></figure-inline> | ||
|- | |- | ||
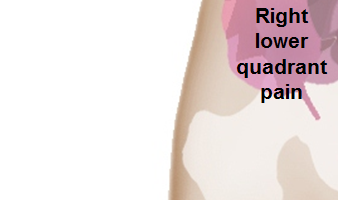
| <figure-inline class="mw-default-size"><figure-inline><figure-inline><figure-inline>[[Image:Right_lower_quadrant.PNG|link=Right lower quadrant abdominal pain resident survival guide|338x338px]]</figure-inline></figure-inline></figure-inline></figure-inline>||<figure-inline class="mw-default-size"><figure-inline><figure-inline><figure-inline>[[Image:Hypogastric.PNG|link=Hypogastric pain resident survival guide|199x199px]]</figure-inline></figure-inline></figure-inline></figure-inline>||<figure-inline class="mw-default-size"><figure-inline><figure-inline><figure-inline>[[Image:Left_lower_quadrant.PNG|link=Left lower quadrant abdominal pain resident survival guide|335x335px]]</figure-inline></figure-inline></figure-inline></figure-inline> | | <figure-inline class="mw-default-size"><figure-inline><figure-inline><figure-inline><figure-inline>[[Image:Right_lower_quadrant.PNG|link=Right lower quadrant abdominal pain resident survival guide|338x338px]]</figure-inline></figure-inline></figure-inline></figure-inline></figure-inline>||<figure-inline class="mw-default-size"><figure-inline><figure-inline><figure-inline><figure-inline>[[Image:Hypogastric.PNG|link=Hypogastric pain resident survival guide|199x199px]]</figure-inline></figure-inline></figure-inline></figure-inline></figure-inline>||<figure-inline class="mw-default-size"><figure-inline><figure-inline><figure-inline><figure-inline>[[Image:Left_lower_quadrant.PNG|link=Left lower quadrant abdominal pain resident survival guide|335x335px]]</figure-inline></figure-inline></figure-inline></figure-inline></figure-inline> | ||
|} | |} | ||
Revision as of 16:36, 21 November 2017
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Amandeep Singh M.D.[2]
Differential diagnosis of abdominal pain
Differential diagnosis
Abbreviations:
RUQ= Right upper quadrant of the abdomen, LUQ= Left upper quadrant, LLQ= Left lower quadrant, RLQ= Right lower quadrant, LFT= Liver function test, SIRS= Systemic inflammatory response syndrome, ERCP= Endoscopic retrograde cholangiopancreatography, IV= Intravenous, N= Normal, AMA= Anti mitochondrial antibodies, LDH= Lactate dehydrogenase, GI= Gastrointestinal, CXR= Chest X ray, IgA= Immunoglobulin A, IgG= Immunoglobulin G, IgM= Immunoglobulin M, CT= Computed tomography, PMN= Polymorphonuclear cells, ESR= Erythrocyte sedimentation rate, CRP= C-reactive protein
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||