Sandbox:Mehrian: Difference between revisions
No edit summary |
No edit summary |
||
| Line 1: | Line 1: | ||
__NOTOC__ | |||
Classic salt | {{Congenital adrenal hyperplasia}} | ||
{{CMG}}; {{AE}}{{MJ}} | |||
{{SK}} Congenital adrenal hyperplasia, CAH, Adrenal hyperplasia | |||
==Overview== | |||
Congenital adrenal hyperplasia (CAH) refers to any of several autosomal recessive conditions resulting from biochemical paths of the steroidogenesis of cortisol from cholesterol by the adrenal glands. Most of these conditions involve greater or lesser production of sex steroids and can alter development of primary or secondary sex characteristics in affected infants, children, and adults. Only a small minority of people with CAH can be said to have an intersex condition, but this attracted American public attention in the late 1990s and many accounts of varying accuracy have appeared in the popular media. Approximately 95% of cases of CAH are due to 21-hydroxylase deficiency. | |||
Prenatal diagnosis can be made in both of these disorders by chorionic villous sampling, but this can only be done at 8-10 weeks. In order to prevent the deleterious effect of excess androgens on genital (and brain!) development, therapy must be started earlier. This is most often considered if there is an affected sibling. Treatment is dexamethasone, which is not degraded by the placenta, but is associated with significant maternal weight gain, hypertension, and edema. | |||
==Historical Perspective== | |||
* Congenital adrenal hyperplasia first time seen in 1865 by Luigi De Crecchio, an Italian [[pathologist]], in a man at autopsy, who had large [[adrenal glands]] and female [[internal organs]]. | |||
* Important aspects of discovering [[adrenal]] hormones:<ref name="pmid25635623">{{cite journal |vauthors=Delle Piane L, Rinaudo PF, Miller WL |title=150 years of congenital adrenal hyperplasia: translation and commentary of De Crecchio's classic paper from 1865 |journal=Endocrinology |volume=156 |issue=4 |pages=1210–7 |year=2015 |pmid=25635623 |doi=10.1210/en.2014-1879 |url=}}</ref><ref name="ISBN:978-0323297387">{{cite book | last = Melmed | first = Shlomo | title = Williams textbook of endocrinology | publisher = Elsevier | location = Philadelphia, PA | year = 2016 | isbn = 978-0323297387 }}=</ref><ref name="pmid18118071">{{cite journal |vauthors=HENCH PS, KENDALL EC |title=The effect of a hormone of the adrenal cortex (17-hydroxy-11-dehydrocorticosterone; compound E) and of pituitary adrenocorticotropic hormone on rheumatoid arthritis |journal=Proc Staff Meet Mayo Clin |volume=24 |issue=8 |pages=181–97 |year=1949 |pmid=18118071 |doi= |url=}}</ref><ref name="pmid4288776">{{cite journal |vauthors=Biglieri EG, Herron MA, Brust N |title=17-hydroxylation deficiency in man |journal=J. Clin. Invest. |volume=45 |issue=12 |pages=1946–54 |year=1966 |pmid=4288776 |pmc=292880 |doi=10.1172/JCI105499 |url=}}</ref> | |||
** In 1563, Eustachius described the [[Adrenal|adrenals]] and then published by Lancisi in 1714. | |||
** In 1849, [[Thomas Addison]], found on a bronzed appearance associated with the [[adrenal glands]] called [[melasma]] suprarenale while searching for the cause of [[pernicious anemia]]. | |||
** In 1855, [[Thomas Addison]] defined the clinical features and [[autopsy]] findings in 11 cases of diseases of the [[suprarenal]] capsules, and half of them were [[tuberculous]] in origin. | |||
** In 1856, In [[adrenalectomy]] experiments, [[Brown-Sequard syndrome|Brown-Séquard]] found that the [[adrenal glands]] are nessesary for life. | |||
** In 1896, [[William Osler]] prepared an oral glycerin extract derived from pig [[Adrenal|adrenals]] and showed that it had clinical benefit in patients with [[Addison disease]]. | |||
** In 1905, Bulloch and Sequeira described patients with [[congenital adrenal hyperplasia]]. | |||
** In 1936, Selye described the concept of stress and its effect on [[pituitary]]-[[adrenal]] function. | |||
** In 1937-1952, Kendall and Reichstein, defined the isolation and structural characterization of [[Adrenocortical hormone|adrenocortical hormones]]. | |||
** In 1943, Li and colleagues isolated [[adrenocorticotropic hormone]] from sheep [[pituitary]]. | |||
** In 1950, Hench, Kendall, and Reichstein shared the [[Nobel Prize in Medicine]] for describing the [[anti-inflammatory]] effects of [[cortisone]] in patients with [[rheumatoid arthritis]] | |||
** In 1956, Conn described [[primary aldosteronism]]. | |||
** In 1981, Vale defined characterization and synthesis of [[corticotropin-releasing hormone]]. | |||
** From 1980-present called the molecular era; highlights in this section are: | |||
*** Cloning and functional characterization of [[Steroid hormone receptor|steroid hormone receptors]] discovered. | |||
*** [[Steroidogenic]] [[enzymes]] described. | |||
*** [[Adrenal]] [[transcription factors]] were reported. | |||
*** [[Molecular]] basis for human adrenal diseases described. | |||
==Pathophisiology== | |||
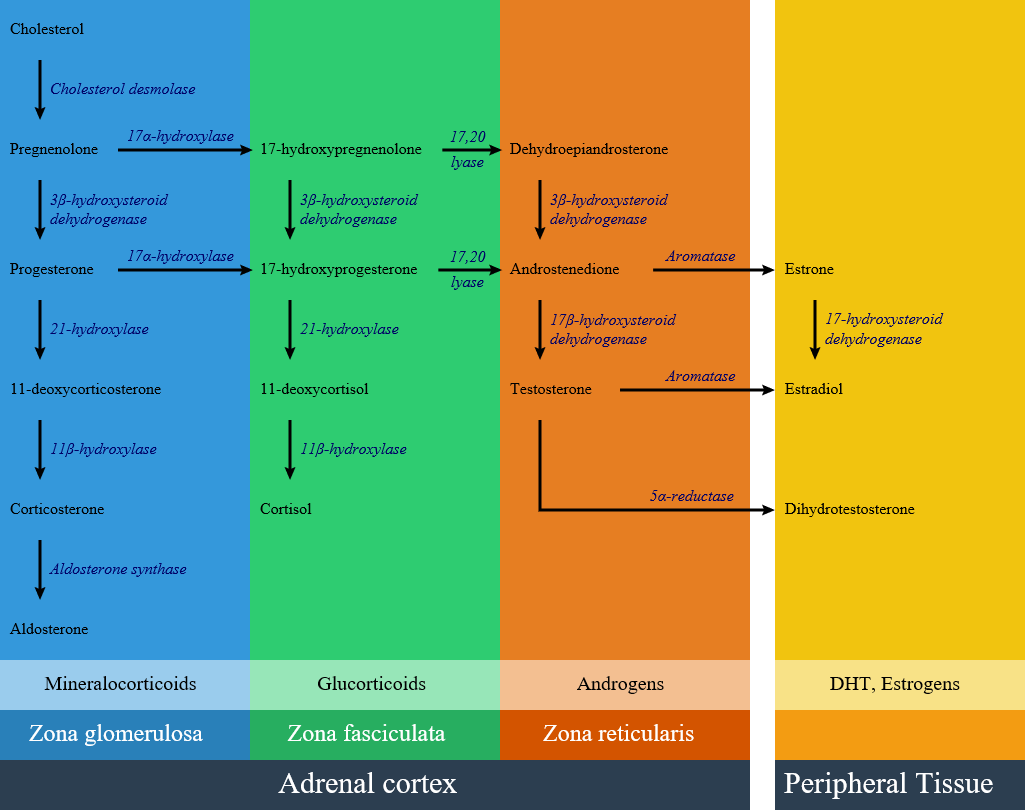
[[image:Adrenal Steroids.png|600px]] | |||
==Gross Pathology== | |||
Gross pathology findings in patients with congenital adrenal hyperplasia are:<ref name="radio">Congenital adrenal hyperplasia. Dr Henry Knipe and Dr M Venkatesh . Radiopaedia.org 2015.http://radiopaedia.org/articles/congenital-adrenal-hyperplasia</ref><ref name="pmid25372578">{{cite journal |vauthors=Teixeira SR, Elias PC, Andrade MT, Melo AF, Elias Junior J |title=The role of imaging in congenital adrenal hyperplasia |journal=Arq Bras Endocrinol Metabol |volume=58 |issue=7 |pages=701–8 |year=2014 |pmid=25372578 |doi= |url=}}</ref> | |||
*Enlarged adrenal glands | |||
*Wrinkled surface adrenal glands | |||
*Cerebriform pattern adrenal glands (pathognomonic sign) | |||
*Normal ultrasound appearances may also be seen | |||
*Testicular masses may be identified representing adrenal rest tissue | |||
==Microscopic Pathology== | |||
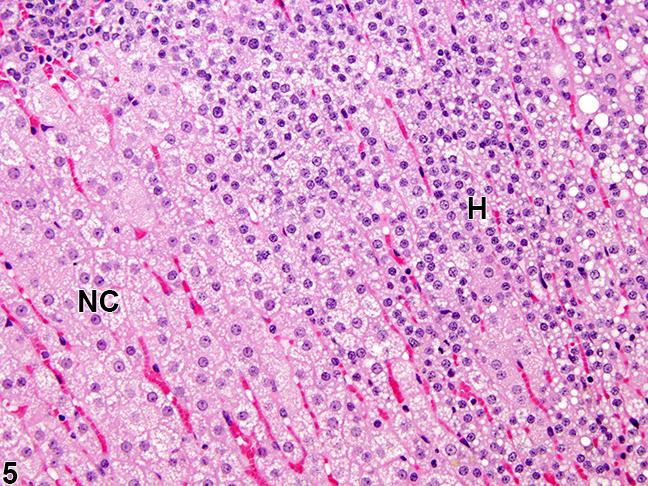
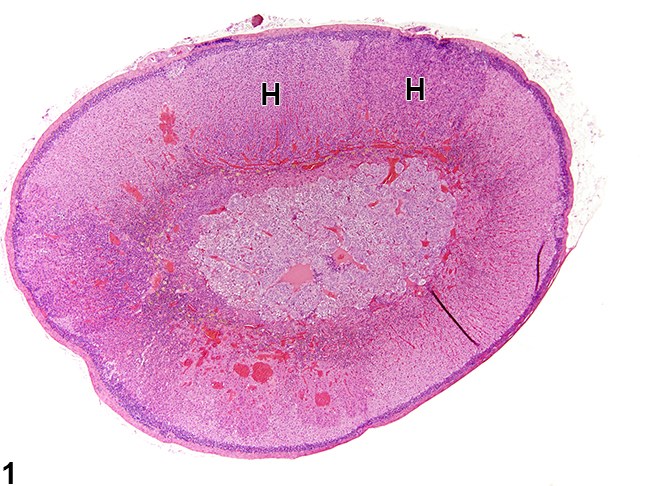
In congenital adrenal hyperplasia, hyperplastic cells are usually but not always smaller, with cytoplasm that can be vacuolated also often more basophilic. Rare mitotic figures may be present, but the hyperplastic cells typically lack features of cellular atypia.<ref name="urlAdrenal Gland - Hyperplasia - Nonneoplastic Lesion Atlas">{{cite web |url=https://ntp.niehs.nih.gov/nnl/endocrine/adrenal/hyperpl/index.htm |title=Adrenal Gland - Hyperplasia - Nonneoplastic Lesion Atlas |format= |work= |accessdate=}}</ref> | |||
> | {| | ||
| | |||
> | [[Image:Cah mic.jpg|thumb|200px|frame|Adrenal gland, Cortex - Hyperplasia in a female rat from a chronic study. There is a hyperplastic lesion (H) in which cortical cells are increased in number but are smaller in size than adjacent normal cortical cells (NC)]]<ref name="urlAdrenal Gland - Hyperplasia - Nonneoplastic Lesion Atlas">{{cite web |url=https://ntp.niehs.nih.gov/nnl/endocrine/adrenal/hyperpl/index.htm |title=Adrenal Gland - Hyperplasia - Nonneoplastic Lesion Atlas |format= |work= |accessdate=}}</ref> | ||
| | |||
[[Image:Cah.jpg|thumb|250px|frame|Adrenal gland, Cortex - Hyperplasia in a male rat from a chronic study. There are two adjacent foci of hyperplasia (H) in the zona fasciculata.]]<ref name="urlAdrenal Gland - Hyperplasia - Nonneoplastic Lesion Atlas">{{cite web |url=https://ntp.niehs.nih.gov/nnl/endocrine/adrenal/hyperpl/index.htm |title=Adrenal Gland - Hyperplasia - Nonneoplastic Lesion Atlas |format= |work= |accessdate=}}</ref> | |||
|} | |||
==Classification== | |||
Congenital adrenal hyperplasia is classified into seven types based on the genetic causes that lead to hyperplasia and hormonal imbalance. | |||
{| align="center" class="wikitable" style="border: 0px; font-size: 90%; margin: 3px;" | |||
! align="center" style="background:#DCDCDC;" rowspan="2" colspan="2" |Disease | |||
! align="center" style="background:#DCDCDC;" colspan="2" |History and symptoms | |||
! align="center" style="background:#DCDCDC;" colspan="3" |Laboratory findings | |||
! align="center" style="background:#DCDCDC;" |Defective gene | |||
|- | |||
!Blood pressure | |||
!Genitalia | |||
!Increased | |||
!Decreased | |||
!K levels | |||
! | |||
|- | |||
| align="center" style="padding: 5px 5px; background: #DCDCDC;" rowspan="2" |[[21-hydroxylase deficiency]] | |||
- | |Classic type | ||
| | |||
* Low in salt-wasting | |||
* Normal in non-salt-wasting | |||
| | |||
* Female: ambiguous | |||
* Male: normal or scrotal pigmentation and large phallus | |||
| | |||
* [[Deoxycorticosterone]] | |||
* 11-Deoxy-[[cortisol]] | |||
* [[17-Hydroxyprogesterone|17-hydroxyprogesterone]], mild elevation | |||
| | |||
* [[Cortisol]] | |||
* [[Corticosterone]] | |||
* [[Aldosterone]] | |||
| | |||
* High in salt wasting type | |||
* Normal in non salt wasting | |||
| | |||
* CYP21A1 and CYP21A2 gene | |||
|- | |||
|Non-classic type | |||
| | |||
* Normal | |||
| | |||
* Female: virilization after puberty | |||
* Male: normal appearance | |||
| | |||
* [[17-Hydroxyprogesterone|17-hydroxyprogesterone]] | |||
* Exaggerated [[Androstenedione]], [[DHEA]], and [[17-Hydroxyprogesterone|17-hydroxyprogesterone]] | |||
response to [[ACTH]] | |||
| | |||
| | |||
* Normal | |||
| | |||
* CYP21A1 and CYP21A2 gene | |||
|- | |||
| align="center" style="padding: 5px 5px; background: #DCDCDC;" colspan="2" |[[17 alpha-hydroxylase deficiency|17-α hydroxylase deficiency]] | |||
| align="center" style="padding: 5px 5px; background: #F5F5F5;" | | |||
* Hypertension | |||
| | |||
* Female: normal | |||
* Male: ambiguous | |||
| align="center" style="padding: 5px 5px; background: #F5F5F5;" | | |||
* [[Deoxycorticosterone]] | |||
* [[Corticosterone]] | |||
* [[Progesterone]] | |||
| | |||
* [[Cortisol]] | |||
* [[Aldosterone]] | |||
| | |||
* Low | |||
| align="center" style="padding: 5px 5px; background: #F5F5F5;" | | |||
* CYP17A1 | |||
|- | |||
| align="center" style="padding: 5px 5px; background: #DCDCDC;" colspan="2" |[[11β-hydroxylase deficiency|11-β hydroxylase deficiency]] | |||
| align="center" style="padding: 5px 5px; background: #F5F5F5;" | | |||
* Hypertension | |||
| | |||
* Female: ambiguous | |||
* Male: normal or scrotal pigmentation and large phallus | |||
| align="center" style="padding: 5px 5px; background: #F5F5F5;" | | |||
* [[Deoxycorticosterone]] | |||
* 11-Deoxy-[[cortisol]] | |||
* [[17-Hydroxyprogesterone|17-hydroxyprogesterone]], mild elevation | |||
| | |||
* [[Cortisol]] | |||
* [[Corticosterone]] | |||
* [[Aldosterone]] | |||
| | |||
* Low | |||
| align="center" style="padding: 5px 5px; background: #F5F5F5;" | | |||
* CYP11B1 | |||
|- | |||
| align="center" style="padding: 5px 5px; background: #DCDCDC;" colspan="2" |3β-Hydroxysteroid Dehydrogenase | |||
| align="center" style="padding: 5px 5px; background: #F5F5F5;" | | |||
| | |||
| align="center" style="padding: 5px 5px; background: #F5F5F5;" | | |||
* [[Dehydroepiandrosterone]] | |||
* [[17-hydroxypregnenolone]] | |||
* [[Pregnenolone]] | |||
| | |||
* [[Cortisol]] | |||
* [[Aldosterone]] | |||
| | |||
* High | |||
| align="center" style="padding: 5px 5px; background: #F5F5F5;" | | |||
|- | |||
| align="center" style="padding: 5px 5px; background: #DCDCDC;" colspan="2" |Cytochrome P450-oxidoreductase (POR) deficiency (ORD) | |||
| align="center" style="padding: 5px 5px; background: #F5F5F5;" | | |||
| | |||
| align="center" style="padding: 5px 5px; background: #F5F5F5;" | | |||
| | |||
| | |||
| align="center" style="padding: 5px 5px; background: #F5F5F5;" | | |||
|- | |||
| align="center" style="padding: 5px 5px; background: #DCDCDC;" colspan="2" |Congenital lipoid adrenal hyperplasia | |||
| align="center" style="padding: 5px 5px; background: #F5F5F5;" | | |||
| | |||
| align="center" style="padding: 5px 5px; background: #F5F5F5;" | | |||
| | |||
| | |||
| align="center" style="padding: 5px 5px; background: #F5F5F5;" | | |||
|- | |||
| align="center" style="padding: 5px 5px; background: #DCDCDC;" colspan="2" |Cholesterol side-chain cleavage enzyme deficiency | |||
| align="center" style="padding: 5px 5px; background: #F5F5F5;" | | |||
| | |||
| align="center" style="padding: 5px 5px; background: #F5F5F5;" | | |||
| | |||
| | |||
| align="center" style="padding: 5px 5px; background: #F5F5F5;" | | |||
|} | |||
==Screening== | |||
According to Endocrine Society Clinical Practice Guideline, screening for 21-hydroxylase deficiency by measuring 17a-hydroxyprogesterone is recommended for all newborns. | |||
*Blood sample on filter paper should be obtained from heel puncture preferably between two and four days after birth. | |||
*Screening programs should be done using a two-tier protocol (initial immunoassay with further evaluation of positive tests by liquid chromatography/tandem mass spectrometry. | |||
*Most affected neonates have concentrations greater than 3500 ng/dL (105 nmol/L).<ref name="pmid2208708">{{cite journal |vauthors=Gonzalez RR, Mäentausta O, Solyom J, Vihko R |title=Direct solid-phase time-resolved fluoroimmunoassay of 17 alpha-hydroxyprogesterone in serum and dried blood spots on filter paper |journal=Clin. Chem. |volume=36 |issue=9 |pages=1667–72 |year=1990 |pmid=2208708 |doi= |url=}}</ref><ref name="pmid20823466">{{cite journal |vauthors=Speiser PW, Azziz R, Baskin LS, Ghizzoni L, Hensle TW, Merke DP, Meyer-Bahlburg HF, Miller WL, Montori VM, Oberfield SE, Ritzen M, White PC |title=Congenital adrenal hyperplasia due to steroid 21-hydroxylase deficiency: an Endocrine Society clinical practice guideline |journal=J. Clin. Endocrinol. Metab. |volume=95 |issue=9 |pages=4133–60 |year=2010 |pmid=20823466 |pmc=2936060 |doi=10.1210/jc.2009-2631 |url=}}</ref> | |||
===Genetic counseling=== | |||
The Endocrine Society's Clinical Practice Guideline recommends that genetic counseling be provided for individuals who are planning to conceive, and there is a family history of 21-hydroxylase deficiency.<ref name="pmid20823466">{{cite journal |vauthors=Speiser PW, Azziz R, Baskin LS, Ghizzoni L, Hensle TW, Merke DP, Meyer-Bahlburg HF, Miller WL, Montori VM, Oberfield SE, Ritzen M, White PC |title=Congenital adrenal hyperplasia due to steroid 21-hydroxylase deficiency: an Endocrine Society clinical practice guideline |journal=J. Clin. Endocrinol. Metab. |volume=95 |issue=9 |pages=4133–60 |year=2010 |pmid=20823466 |pmc=2936060 |doi=10.1210/jc.2009-2631 |url=}}</ref> | |||
==Differentiating congenital adrenal hyperplasia from other diseases== | |||
[[Congenital adrenal hyperplasia]] must be differentiated from diseases that cause [[ambiguous genitalia]]:<ref name="pmid17875484">{{cite journal |vauthors=Hughes IA, Nihoul-Fékété C, Thomas B, Cohen-Kettenis PT |title=Consequences of the ESPE/LWPES guidelines for diagnosis and treatment of disorders of sex development |journal=Best Pract. Res. Clin. Endocrinol. Metab. |volume=21 |issue=3 |pages=351–65 |year=2007 |pmid=17875484 |doi=10.1016/j.beem.2007.06.003 |url=}}</ref><ref name="pmid10857554">{{cite journal |vauthors=White PC, Speiser PW |title=Congenital adrenal hyperplasia due to 21-hydroxylase deficiency |journal=Endocr. Rev. |volume=21 |issue=3 |pages=245–91 |year=2000 |pmid=10857554 |doi=10.1210/edrv.21.3.0398 |url=}}</ref> | |||
{| class="wikitable" | |||
!Disease name | |||
! colspan="2" |Laboratory tests | |||
!Important clinical findings | |||
|- | |||
! | |||
!Increased | |||
!Decreased | |||
! | |||
|- | |||
|[[21-hydroxylase deficiency|Classic type of 21-hydroxylase deficiency]] | |||
| | |||
* [[17-Hydroxyprogesterone|17-hydroxyprogesterone]] | |||
* [[Progesterone]] | |||
* [[Androstenedione]] | |||
* [[DHEA]] | |||
| | |||
* [[Aldosterone]] | |||
* [[Corticosterone]] (salt-wasting) | |||
* [[Cortisol]] (simple [[virilizing]]) | |||
| | |||
* [[Ambiguous genitalia]] in female | |||
* [[Virilization]] in female | |||
* Salt-wasting | |||
* [[Hypotension]] and [[hyperkalemia]] | |||
|- | |||
|[[11β-hydroxylase deficiency|11-β hydroxylase deficiency]] | |||
| | |||
* [[Deoxycorticosterone]] | |||
* 11-Deoxy-[[cortisol]] | |||
* [[17-Hydroxyprogesterone|17-hydroxyprogesterone]], mild elevation | |||
| | |||
* [[Cortisol]] | |||
* [[Corticosterone]] | |||
* [[Aldosterone]] | |||
| | |||
* [[Ambiguous genitalia]] in female | |||
* [[Hypertension]] and [[hypokalemia]] | |||
* [[Virilization]] | |||
|- | |||
|[[17 alpha-hydroxylase deficiency|17-α hydroxylase deficiency]] | |||
| | |||
* [[Deoxycorticosterone]] | |||
* [[Corticosterone]] | |||
* [[Progesterone]] | |||
| | |||
* [[Cortisol]] | |||
* [[Aldosterone]] | |||
| | |||
* [[Ambiguous genitalia]] in male | |||
* [[Hypertension]] | |||
* [[Primary amenorrhea]] | |||
* Absence of [[secondary sexual characteristics]] | |||
* Minimal [[body hair]] | |||
|- | |||
|3β-Hydroxysteroid Dehydrogenase | |||
| | |||
* [[Dehydroepiandrosterone]] | |||
* [[17-hydroxypregnenolone]] | |||
* [[Pregnenolone]] | |||
| | |||
* [[Cortisol]] | |||
* [[Aldosterone]] | |||
| | |||
* [[Vomiting]], [[volume depletion]], [[hyponatremia]], and [[hyperkalemia]] | |||
* 46-XY infants often show [[undervirilization]], due to a block in [[testosterone]] synthesis | |||
|- | |||
|Gestational [[hyperandrogenism]] | |||
| colspan="2" | | |||
* Maternal serum [[androgen]] concentrations (usually [[testosterone]] and [[androstenedione]]) are high | |||
* If [[virilization]] is caused by exogenous hormone administration, the values may be low because the offending hormone is usually a synthetic [[steroid]] not measured in assays for [[testosterone]] or other [[androgens]] | |||
| | |||
* [[Androgen]] excess sign and symptoms in mother | |||
* History of [[androgen]] containing [[medication]] consumption during [[pregnancy]] in mother | |||
* [[Virilization]] in a 46,XX individual with normal female internal anatomy | |||
* Causes include maternal [[luteoma]] or theca-[[lutein]] [[cysts]], and [[placental]] [[aromatase]] enzyme deficiency | |||
|} | |||
congenital adrenal hyperplasia must be differentiated from diseases that cause [[virilization]] and [[hirsutism]] in female:<ref name="pmid24830586">{{cite journal |vauthors=Hohl A, Ronsoni MF, Oliveira Md |title=Hirsutism: diagnosis and treatment |journal=Arq Bras Endocrinol Metabol |volume=58 |issue=2 |pages=97–107 |year=2014 |pmid=24830586 |doi= |url=}}</ref><ref name="pmid10857554">{{cite journal |vauthors=White PC, Speiser PW |title=Congenital adrenal hyperplasia due to 21-hydroxylase deficiency |journal=Endocr. Rev. |volume=21 |issue=3 |pages=245–91 |year=2000 |pmid=10857554 |doi=10.1210/edrv.21.3.0398 |url=}}</ref><ref name="ISBN:978-0323297387">{{cite book | last = Melmed | first = Shlomo | title = Williams textbook of endocrinology | publisher = Elsevier | location = Philadelphia, PA | year = 2016 | isbn = 978-0323297387 }}=</ref> | |||
{| class="wikitable" | |||
!Disease name | |||
!Steroid status | |||
!Other laboratory | |||
!Important clinical findings | |||
|- | |||
|Non-classic type of 21-hydroxylase deficiency | |||
|Increased: | |||
* [[17-Hydroxyprogesterone|17-hydroxyprogesterone]] | |||
* Exaggerated [[Androstenedione]], [[DHEA]], and [[17-Hydroxyprogesterone|17-hydroxyprogesterone]] | |||
response to [[ACTH]] | |||
| | |||
* Low [[testosterone]] levels | |||
| | |||
* No symptoms in infancy and male | |||
* [[Virilization]] in females | |||
|- | |||
|[[11β-hydroxylase deficiency|11-β hydroxylase deficiency]] | |||
|Increased: | |||
* DOC | |||
* 11-Deoxy-[[Cortisol]] | |||
Decreased: | |||
* [[Cortisol]] | |||
* [[Corticosterone]] | |||
* [[Aldosterone]] | |||
| | |||
* Low [[testosterone]] levels | |||
| | |||
* [[Hypertension]] and [[hypokalemia]] | |||
* [[Virilization]] | |||
|- | |||
|3β-Hydroxysteroid Dehydrogenase | |||
|Increased: | |||
* [[DHEA]] | |||
* [[17-hydroxypregnenolone]] | |||
* [[Pregnenolone]] | |||
Decreased: | |||
* [[Cortisol]] | |||
* [[Aldosterone]] | |||
| | |||
* Low [[testosterone]] levels | |||
| | |||
* Salt-wasting [[adrenal crisis]] in infancy | |||
* Mild [[virilization]] of genetically female infants | |||
* [[Undervirilization]] of genetically male infants, making it the only form of [[CAH]] which can cause [[ambiguous genitalia]] in both genetic sexes. | |||
|- | |||
|[[Polycystic ovary syndrome ]] | |||
| | |||
* High [[DHEAS]] and [[androstenedione]] levels | |||
| | |||
* Low [[testosterone]] levels | |||
| | |||
* [[Polycystic ovaries]] in sonography | |||
* [[Obesity]] | |||
* [[PCOS]] is the most common cause of [[hirsutism]] in women | |||
* No evidence another diagnosis | |||
|- | |||
|[[Adrenal tumors]] | |||
| | |||
* Variable levels depends on [[tumor]] type | |||
| | |||
* Low [[testosterone]] level | |||
| | |||
* Older age | |||
* Rapidly progressive symptoms | |||
|- | |||
|Ovarian [[virilizing]] tumor | |||
| | |||
* Variable levels depends on [[tumor]] type | |||
| | |||
* [[Testosterone]] is high | |||
| | |||
* Older age | |||
* Rapidly progressive symptoms | |||
|- | |||
|[[Cushing's syndrome]] | |||
| | |||
* Increase [[cortisol]] & metabolites | |||
* Variable other [[steroids]] | |||
| | |||
* Variable [[mineralocorticoid]] excess | |||
| | |||
* [[Cushingoid appearance]] | |||
|- | |||
|[[Hyperprolactinemia]] | |||
| | |||
* Normal levels of most of [[steroids]] | |||
| | |||
* Increased [[prolactin]] | |||
| | |||
* [[Infertility]], [[galactorrhea]] | |||
|} | |||
==References== | |||
{{reflist|2}} | |||
Revision as of 19:21, 1 August 2017
|
Congenital adrenal hyperplasia main page |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Mehrian Jafarizade, M.D [2]
Synonyms and keywords: Congenital adrenal hyperplasia, CAH, Adrenal hyperplasia
Overview
Congenital adrenal hyperplasia (CAH) refers to any of several autosomal recessive conditions resulting from biochemical paths of the steroidogenesis of cortisol from cholesterol by the adrenal glands. Most of these conditions involve greater or lesser production of sex steroids and can alter development of primary or secondary sex characteristics in affected infants, children, and adults. Only a small minority of people with CAH can be said to have an intersex condition, but this attracted American public attention in the late 1990s and many accounts of varying accuracy have appeared in the popular media. Approximately 95% of cases of CAH are due to 21-hydroxylase deficiency. Prenatal diagnosis can be made in both of these disorders by chorionic villous sampling, but this can only be done at 8-10 weeks. In order to prevent the deleterious effect of excess androgens on genital (and brain!) development, therapy must be started earlier. This is most often considered if there is an affected sibling. Treatment is dexamethasone, which is not degraded by the placenta, but is associated with significant maternal weight gain, hypertension, and edema.
Historical Perspective
- Congenital adrenal hyperplasia first time seen in 1865 by Luigi De Crecchio, an Italian pathologist, in a man at autopsy, who had large adrenal glands and female internal organs.
- Important aspects of discovering adrenal hormones:[1][2][3][4]
- In 1563, Eustachius described the adrenals and then published by Lancisi in 1714.
- In 1849, Thomas Addison, found on a bronzed appearance associated with the adrenal glands called melasma suprarenale while searching for the cause of pernicious anemia.
- In 1855, Thomas Addison defined the clinical features and autopsy findings in 11 cases of diseases of the suprarenal capsules, and half of them were tuberculous in origin.
- In 1856, In adrenalectomy experiments, Brown-Séquard found that the adrenal glands are nessesary for life.
- In 1896, William Osler prepared an oral glycerin extract derived from pig adrenals and showed that it had clinical benefit in patients with Addison disease.
- In 1905, Bulloch and Sequeira described patients with congenital adrenal hyperplasia.
- In 1936, Selye described the concept of stress and its effect on pituitary-adrenal function.
- In 1937-1952, Kendall and Reichstein, defined the isolation and structural characterization of adrenocortical hormones.
- In 1943, Li and colleagues isolated adrenocorticotropic hormone from sheep pituitary.
- In 1950, Hench, Kendall, and Reichstein shared the Nobel Prize in Medicine for describing the anti-inflammatory effects of cortisone in patients with rheumatoid arthritis
- In 1956, Conn described primary aldosteronism.
- In 1981, Vale defined characterization and synthesis of corticotropin-releasing hormone.
- From 1980-present called the molecular era; highlights in this section are:
- Cloning and functional characterization of steroid hormone receptors discovered.
- Steroidogenic enzymes described.
- Adrenal transcription factors were reported.
- Molecular basis for human adrenal diseases described.
Pathophisiology
Gross Pathology
Gross pathology findings in patients with congenital adrenal hyperplasia are:[5][6]
- Enlarged adrenal glands
- Wrinkled surface adrenal glands
- Cerebriform pattern adrenal glands (pathognomonic sign)
- Normal ultrasound appearances may also be seen
- Testicular masses may be identified representing adrenal rest tissue
Microscopic Pathology
In congenital adrenal hyperplasia, hyperplastic cells are usually but not always smaller, with cytoplasm that can be vacuolated also often more basophilic. Rare mitotic figures may be present, but the hyperplastic cells typically lack features of cellular atypia.[7]
 |
 |
Classification
Congenital adrenal hyperplasia is classified into seven types based on the genetic causes that lead to hyperplasia and hormonal imbalance.
| Disease | History and symptoms | Laboratory findings | Defective gene | ||||
|---|---|---|---|---|---|---|---|
| Blood pressure | Genitalia | Increased | Decreased | K levels | |||
| 21-hydroxylase deficiency | Classic type |
|
|
|
|
| |
| Non-classic type |
|
|
response to ACTH |
|
| ||
| 17-α hydroxylase deficiency |
|
|
|
| |||
| 11-β hydroxylase deficiency |
|
|
|
|
| ||
| 3β-Hydroxysteroid Dehydrogenase |
|
||||||
| Cytochrome P450-oxidoreductase (POR) deficiency (ORD) | |||||||
| Congenital lipoid adrenal hyperplasia | |||||||
| Cholesterol side-chain cleavage enzyme deficiency | |||||||
Screening
According to Endocrine Society Clinical Practice Guideline, screening for 21-hydroxylase deficiency by measuring 17a-hydroxyprogesterone is recommended for all newborns.
- Blood sample on filter paper should be obtained from heel puncture preferably between two and four days after birth.
- Screening programs should be done using a two-tier protocol (initial immunoassay with further evaluation of positive tests by liquid chromatography/tandem mass spectrometry.
- Most affected neonates have concentrations greater than 3500 ng/dL (105 nmol/L).[8][9]
Genetic counseling
The Endocrine Society's Clinical Practice Guideline recommends that genetic counseling be provided for individuals who are planning to conceive, and there is a family history of 21-hydroxylase deficiency.[9]
Differentiating congenital adrenal hyperplasia from other diseases
Congenital adrenal hyperplasia must be differentiated from diseases that cause ambiguous genitalia:[10][11]
| Disease name | Laboratory tests | Important clinical findings | |
|---|---|---|---|
| Increased | Decreased | ||
| Classic type of 21-hydroxylase deficiency |
|
| |
| 11-β hydroxylase deficiency |
|
| |
| 17-α hydroxylase deficiency |
| ||
| 3β-Hydroxysteroid Dehydrogenase |
| ||
| Gestational hyperandrogenism |
|
| |
congenital adrenal hyperplasia must be differentiated from diseases that cause virilization and hirsutism in female:[12][11][2]
| Disease name | Steroid status | Other laboratory | Important clinical findings |
|---|---|---|---|
| Non-classic type of 21-hydroxylase deficiency | Increased:
response to ACTH |
|
|
| 11-β hydroxylase deficiency | Increased:
Decreased: |
|
|
| 3β-Hydroxysteroid Dehydrogenase | Increased:
Decreased: |
|
|
| Polycystic ovary syndrome |
|
|
|
| Adrenal tumors |
|
|
|
| Ovarian virilizing tumor |
|
|
|
| Cushing's syndrome |
|
||
| Hyperprolactinemia |
|
|
References
- ↑ Delle Piane L, Rinaudo PF, Miller WL (2015). "150 years of congenital adrenal hyperplasia: translation and commentary of De Crecchio's classic paper from 1865". Endocrinology. 156 (4): 1210–7. doi:10.1210/en.2014-1879. PMID 25635623.
- ↑ 2.0 2.1 Melmed, Shlomo (2016). Williams textbook of endocrinology. Philadelphia, PA: Elsevier. ISBN 978-0323297387.=
- ↑ HENCH PS, KENDALL EC (1949). "The effect of a hormone of the adrenal cortex (17-hydroxy-11-dehydrocorticosterone; compound E) and of pituitary adrenocorticotropic hormone on rheumatoid arthritis". Proc Staff Meet Mayo Clin. 24 (8): 181–97. PMID 18118071.
- ↑ Biglieri EG, Herron MA, Brust N (1966). "17-hydroxylation deficiency in man". J. Clin. Invest. 45 (12): 1946–54. doi:10.1172/JCI105499. PMC 292880. PMID 4288776.
- ↑ Congenital adrenal hyperplasia. Dr Henry Knipe and Dr M Venkatesh . Radiopaedia.org 2015.http://radiopaedia.org/articles/congenital-adrenal-hyperplasia
- ↑ Teixeira SR, Elias PC, Andrade MT, Melo AF, Elias Junior J (2014). "The role of imaging in congenital adrenal hyperplasia". Arq Bras Endocrinol Metabol. 58 (7): 701–8. PMID 25372578.
- ↑ 7.0 7.1 7.2 "Adrenal Gland - Hyperplasia - Nonneoplastic Lesion Atlas".
- ↑ Gonzalez RR, Mäentausta O, Solyom J, Vihko R (1990). "Direct solid-phase time-resolved fluoroimmunoassay of 17 alpha-hydroxyprogesterone in serum and dried blood spots on filter paper". Clin. Chem. 36 (9): 1667–72. PMID 2208708.
- ↑ 9.0 9.1 Speiser PW, Azziz R, Baskin LS, Ghizzoni L, Hensle TW, Merke DP, Meyer-Bahlburg HF, Miller WL, Montori VM, Oberfield SE, Ritzen M, White PC (2010). "Congenital adrenal hyperplasia due to steroid 21-hydroxylase deficiency: an Endocrine Society clinical practice guideline". J. Clin. Endocrinol. Metab. 95 (9): 4133–60. doi:10.1210/jc.2009-2631. PMC 2936060. PMID 20823466.
- ↑ Hughes IA, Nihoul-Fékété C, Thomas B, Cohen-Kettenis PT (2007). "Consequences of the ESPE/LWPES guidelines for diagnosis and treatment of disorders of sex development". Best Pract. Res. Clin. Endocrinol. Metab. 21 (3): 351–65. doi:10.1016/j.beem.2007.06.003. PMID 17875484.
- ↑ 11.0 11.1 White PC, Speiser PW (2000). "Congenital adrenal hyperplasia due to 21-hydroxylase deficiency". Endocr. Rev. 21 (3): 245–91. doi:10.1210/edrv.21.3.0398. PMID 10857554.
- ↑ Hohl A, Ronsoni MF, Oliveira M (2014). "Hirsutism: diagnosis and treatment". Arq Bras Endocrinol Metabol. 58 (2): 97–107. PMID 24830586. Vancouver style error: initials (help)