Wide complex tachycardias: Difference between revisions
| Line 125: | Line 125: | ||
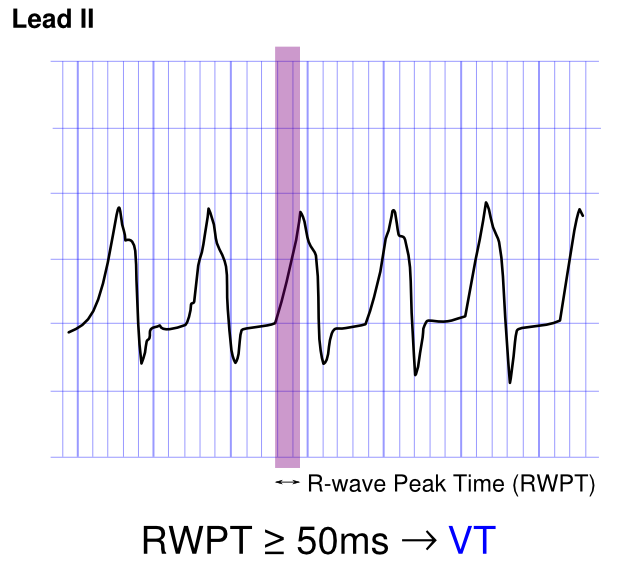
'''Example:''' As shown below, an R-wave to Peak Time (RWPT) of ≥ 50ms in lead II strongly suggests VT: | '''Example:''' As shown below, an R-wave to Peak Time (RWPT) of ≥ 50ms in lead II strongly suggests VT: | ||
[[File:RWPT. | [[File:RWPT.png|center|500px]] | ||
---- | ---- | ||
Revision as of 20:15, 13 October 2012
| Wide complex tachycardias | |
| ICD-10 | I47.2 |
|---|---|
| ICD-9 | 427.1 |
| DiseasesDB | 13819 |
| MeSH | D017180 |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Synonyms and keywords: WCT; fast and wide; wide and fast; wide-complex tachycardia; wide complex rhythm; SVT with aberrancy; SVT with aberrant conduction; supraventricular tachycardia with aberrancy; VT versus SVT
Overview
Wide complex tachycardia is defined as a cardiac rhythm of more than 100 beats per minute with a QRS duration of 120 milliseconds or more. It is critical to differentiate whether the wide complex tachycardia is of ventricular origin and is ventricular tachycardia, or if it is of supraventricular origin with aberrant conduction. Differentiating between these two cause of the wide complex tachycardia is critical because the treatment options are quite different for VT versus SVT with abberancy. Wide complex tachycardia will be due to VT in 80% of cases and will be due to VT in 98% of cases if there's a history of either acute MI or structural heart disease. Only 7% of patients with SVT will have had a prior myocardial infarction (MI).
Causes
A wide complex tachycardia (WCT) can be due to either:
Ventricular Tachycardia
- Ventricular tachycardia (VT) (80% of cases, 98% of cases ff coronary heart disease or structural heart disease are present)
Supraventricular Tachycardia
- Supraventricular tachycardia (SVT) with aberrant ventricular conduction, which is either new or due to a preexisting left or right bundle branch block or a preexisting nonspecific intraventricular conduction delay (IVCD). The underlying supraventricular rhythm that is aberrantly conducted can be any one of the following rhythms:
- Antegrade conduction down an accessory bypass tract
- Atrial flutter with 2:1 conduction and occasional 1:1 conduction
- Automatic junctional tachycardia
- AV nodal reentrant tachycardia
- AV reentrant tachycardia using a bypass tract
- Intraatrial reentrant tachycardia
- Paroxysmal atrial tachycardia
- SA nodal reentrant tachycardia
- Sinus tachycardia
Findings Suggestive of VT
History of Ischemics Heart Disease
A history of ischmeic heart disease or structural heart disease suggests VT. Wide complex tachycardia will be due to VT in 80% of cases and will be due to VT in 98% of cases if there's a history of either acute MI or structural heart disease.
The Presence of AV Dissociation
Although AV dissociation is highly suggestive of VT, it may also be seen in junctional tachycardias with retrograde block.
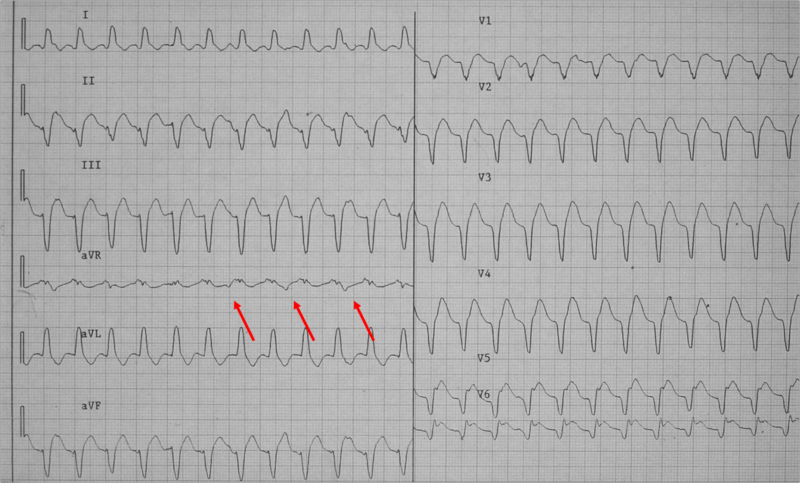
Example: Shown below is a wide complex tachycardia. AV dissociation is present as shown by the varying morphology highlighted by the red arrows. LBBB configuration. Absence of RS in the chest leads. The diagnosis is VT.
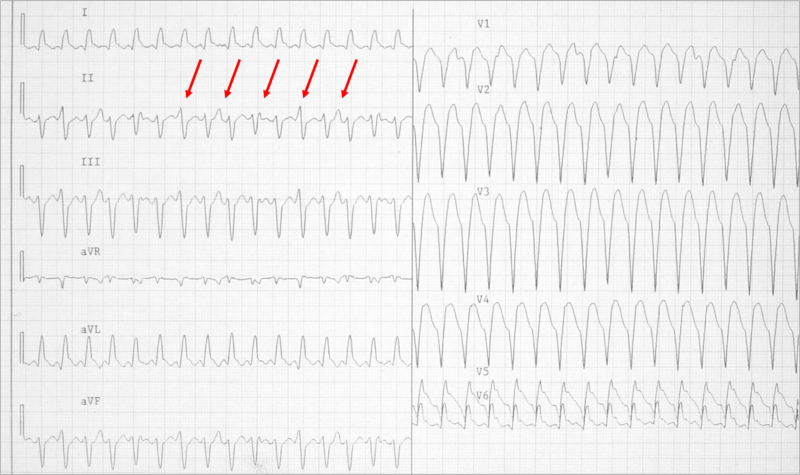
Example: Shown below is a wide complex tachycardia. AV dissociation is present as shown by the varying morphology highlighted by the red arrows. LBBB configuration. Absence of RS in the chest leads. The diagnosis is VT.
Duration of the QRS Complex
- A wide complex tachycardia with a RBBB morphology and a QRS > .14, or a LBBB morphology with a QRS > .16 suggests VT
Morphology of the QRS Complexes
- The finding of a positive or negative QRS complex in all precordial leads is in favor of ventricular tachycardia.
- A monophasic or biphasic RBBB QRS complex in V1. But none of their patients with SVT had a preexisting RBBB. Therefore, this finding is of limited importance. (A Wellens criterion)
- 80 to 85% of aberrant beats have a RBBB pattern, but ectopic beats that arise from the LV have a similar morphology.
- LBBB with a rightward axis
- LBBB with the following QRS morphology
- R wave in V1 or V2 > 0.03 second
- any Q wave in V6
- Onset of the QRS to nadir of the S wave in V1 > 0.06 seconds
- Notching of the S wave in V1 or V2
Morphology of Premature Beats During Sinus Rhythm
- If premature ventricular contractions (PVCs) are present on a prior tracing, and if the morphology of the wide complex tachycardia is the same, then it is likely to be ventricular tachycardia.
- Previous EKG may show a preexisting intraventricular conduction delay (IVCD) which would favor SVT with abberancy.
- If there are premature atrial contractions (PAC)s with aberrant conduction, then the origin of the wide complex tachycardia may be supraventricular.
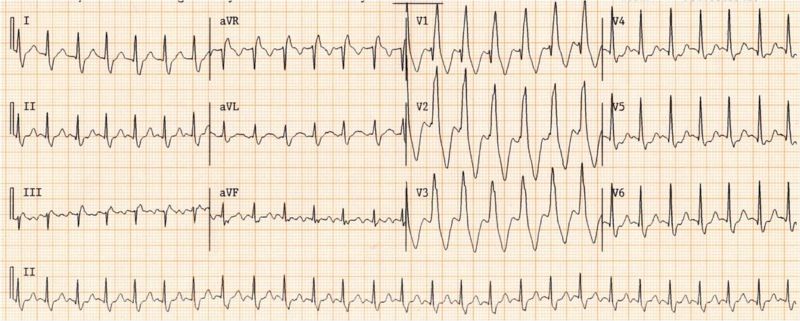
Example: Shown below is a wide complex tachycardia. There is no AV dissociation. A RBBB morphology is present. The wide complex tachycardia resembles sinus rhythm from the same patient. The diagnosis in this patient is SVT with RBBB:
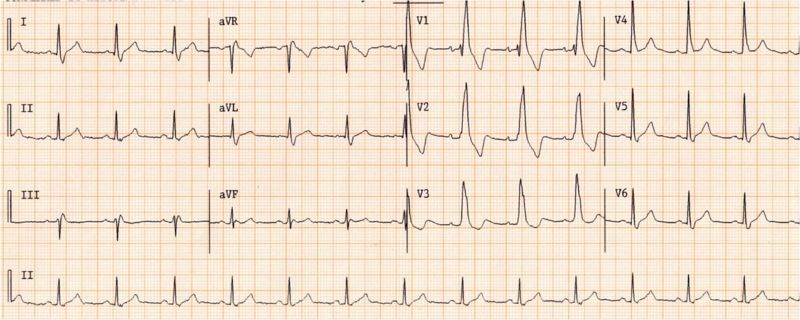
Shown below is the ECG from the same patient as above in sinus rhythm. The QRS complex is very similiar to that during the wide complex tachycardia:
The QRS Axis
- A "Northwest axis" with a QRS axis in the RUQ between -90 and +180 degrees favors ventricular tachycardia
Capture Beats
- Rare, but one of the strongest pieces of evidence in favor of VT.
- SVT with aberrancy rarely follows a beat with a short cycle length.
Fusion Beats
- Rare but also strongly suggests VT.
Vagal Manuevers
- VT is generally not affected by vagal stimulation.
- May terminate reentrant arrhythmias
Atrial pacing
- A pacing wire is placed in the RA and the atrium is stimulated at a rate faster than the tachycardia.
- If ventricular capture occurs and the QRS is normal in duration, then one can exclude the possibility of aberrant conduction.
Onset of the Tachycardia
- Diagnosis of SVT made if the episode is initiated by a premature P wave.
- If the paroxysm begins with a QRS then the tachycardia may be either ventricular or junctional in origin.
- If the first QRS of the tachycardia is preceded by a sinus p wave with a PR interval shorter than that of the conducted sinus beats, the tachycardia is ventricular.
His Bundle Recording
- In SVT, each QRS is preceded by a His bundle potential.
- In VT there is no preceding His deflection.
- The retrograde His deflection is usually obscured by the much larger QRS complex.
Regularity of the Rhythm
Regular
- VT (slight irregularity of RR)
- SVT with aberrancy: Sinus, atrial tachycardia (AT), or Flutter.
- Antidromic atrioventricular reentrant tachycardia (AVRT)
Irregular
- The first 50 beats of VT can be irregular
- SVT with aberrancy: Atrial fibrillation, multifocal atrial tachycardia (MAT)
- Atrial fibrillation with bypass tract
- The mechanism of SVT with aberrancy is usually concealed retrograde conduction. The ventricular beat penetrates the right branch (RB) or left branch (LB). When the next supraventricular activation front occurs that bundle is refractory and if conduction can occur, it will proceed down the other bundle. Since the RB has a longer refractory period than the LB, a right bundle branch block (RBBB) morphology is more common.
- Other mechanisms of “rate related aberrancy” are preexisting bundle branch block (BBB), physiologic (phase 3) aberration and use dependent aberration secondary to medication. In physiologic aberration, the stimulus comes to the His-Purkinje system before it has fully recovered from the previous stimulus. The ensuing activation is either blocked or conducts slowly. Again, the RB is the one more at risk. Most commonly seen at the onset of paroxysmal supraventricular tachycardia (PSVT), but can become sustained.
- In use-dependent aberration, a patient on and anti-arrhythmic (especially class Ic agents) will have a progressive decrement in ventricular conduction rate the more it is stimulated. During faster heart rates, less time is available for the drug to dissociate from the receptor and an increased number of receptors are blocked.
Brugada Criteria
In 2010 Joseph Brugada et al. published a new criterion to differentiate VT from SVT in wide complex tachycardias: the R wave peak time (RWPT) in Lead II. They suggest measuring the duration of onset of the QRS to the first change in polarity (either nadir Q or peak R) in lead II. If the RWPT is ≥ 50ms the likelihood of a VT very high (positive likelihood ratio 34.8). This criterion was successful in their own population of 163 selected patients and is awaiting prospective testing in a larger trial.
Example: As shown below, an R-wave to Peak Time (RWPT) of ≥ 50ms in lead II strongly suggests VT:
Pearls from Mark E. Josephson
- In a wide complex tachycardia with right bundle branch block (RBBB) morphology with normal or inferior axis, VT is associated with an R/S ratio may be >1, and SVT with an R/S ratio <1
- If the QRS during the wide complex tachycardia is narrower than in normal sinus rhythm (NSR), this suggests VT
Differentiation of VT from Antidromic AVRT
- Angina pectoris (AP) activate ventricles from base to apex by virtue of their location in the atrioventricular (AV) ring. This results in predominately positive QRS complexes in V4-V6. If negative, favors VT. For same reason, qR complexes in V2-V4 cannot be found in AVRT unless there is preexisting heart disease.[1] [2] [3]
- Because the atria are part of the circuit in AVRT, any relationship other than 1:1 of P and QRS means VT (100%).
ACC Algorithm for Distinguishing SVT from VT
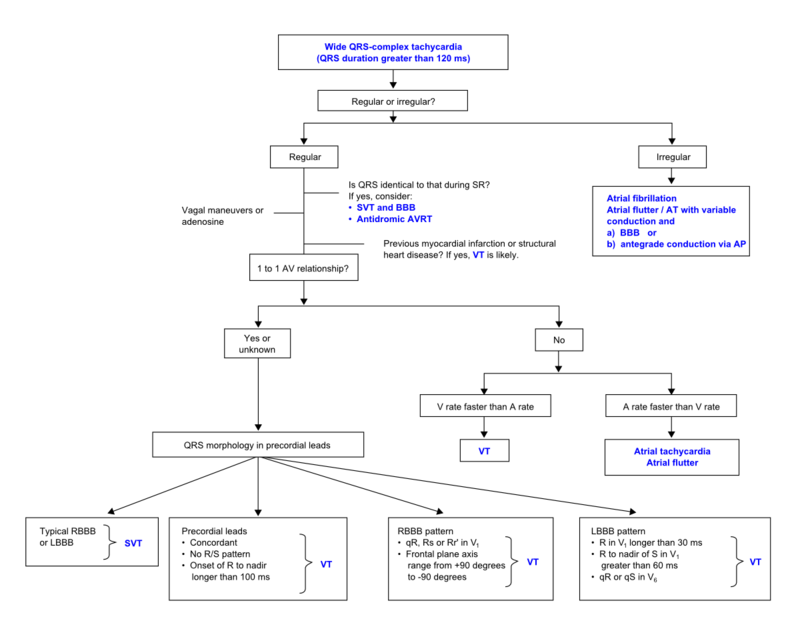
The above figure is adpated from the American College of Cardiology algorithm.
Diagnosis
History
The patient should be asked about drugs that are associated with ventricular tachycardia and if there is a history of ischemic heart disease which would dramatically increase the odds that the rhythm is VT. Wide complex tachycardia will be due to VT in 80% of cases and will be due to VT in 98% of cases if there's a history of either acute MI or structural heart disease. Only 7% of patients with SVT will have had a prior myocardial infarction (MI). VT or an accelerated idioventricular rhythm can be seen following reperfusion in STEMI. Digoxin, antiarrhythmics, phenothiazines, TCAs, and pheochromocytoma may also cause VT. Recent procedures such as cardiac catheterization, DC countershock, repair of congenital lesions are all associated iwth VT. A family history of sudden cardiac death, a history of a channelopathy associated with arrhythmias, and the hereditary Long QT syndrome, and Brugada syndrome are all associated with VT.
Symptoms
- Shortness of breath
- Syncope
- Sudden cardiac death would suggest a diagnosis of ventricular tachycardia
Physical Examination
- Vitals should be obtained to assess hemodynamic stability and guide therapy
- Cannon-a waves are a manifestation of AV dissociation and suggest VT
- Carotid sinus massage (CSM)/Valsalva: ST can gradually slow. MAT, AT, Flutter, and AF may transiently slow. An AV nodal dependent WCT may terminate. AV dissociation may become more apparent with CSM in VT. VT can terminate with CSM
Electrocardiogram
- Extreme axis deviation favors VT. Especially -90 to -180 or “northwest” or “superior” axis. (23% of SVT will have SAD)
- QRS duration >140 msec favors VT (21% of VT will have QRS <140 msec)
- AV dissociation is demonstrated in only 21% of VT
- Morphologic Criteria
- 4% of SVT and 6% of VT did not fulfill criteria in any lead
- 40% will have discordance between V1/V2 and V5/V6. One lead may suggest VT while another suggests SVT.
- An algorithmic approach was proposed by Brugada in 1991. It has a reported sensitivity of 99% and specificity of 97%.
| example | regularity | atrial frequency | ventricular frequency | origin (SVT/VT) | p-wave | effect of adenosine | |
|---|---|---|---|---|---|---|---|
| Wide complex (QRS>0.12) | |||||||
| Ventricular Tachycardia | regular (mostly) | 60-100 bpm | 110-250 bpm | ventricle (VT) | AV-dissociation | no rate reduction (sometimes accelerates) | |
| Ventricular Fibrillation | irregular | 60-100 bpm | 400-600 bpm | ventricle (VT) | AV-dissociation | none | |
| Ventricular Flutter | regular | 60-100 bpm | 150-300 bpm | ventricle (VT) | AV-dissociation | none | |
| Accelerated Idioventricular Rhythm | regular (mostly) | 60-100 bpm | 50-110 bpm | ventricle (VT) | AV-dissociation | no rate reduction (sometimes accelerates) | |
| Torsade de Pointes | regular | 150-300 bpm | ventricle (VT) | AV-dissociation | no rate reduction (sometimes accelerates) | ||
| Bundle-branch re-entrant tachycardia* | regular | 60-100 bpm | 150-300 bpm | ventricles (VT) | AV-dissociation | no rate reduction | |
| *) Bundle-branch re-entrant tachycardia is extremely rare | |||||||
Electrocardiographic Examples
Treatment
Defibrillation
Indications for defibrillation include the following:
- Chest pain
- Congestive heart failure (CHF)
- Hypotension with symptoms
- Loss of consciousness
- Seizure
Acute Pharmacotherapies
- If stable: (More patients than you think)
- DO NOT USE Ca2+ Channel blocker, Digoxin or Adenosine if you don't not know the etiology of the Wide Complex Tachycardia. Ca2+ Channel blockers and Digoxin can lead to accelerated conduction down a bypass tract and VF.
- Though ACLS guidelines recommend a diagnostic trial of Adenosine, it can precipitate VF in some patients with SVT. Patients who have underlying coronary disease may become ischemic from coronary steal. Rhythm can degenerate and lead to VF that cannot be resuscitated. Furthermore, some VT (esp those with structurally normal hearts) are adenosine responsive and can terminate.
- Etiology Uncertain
- Pronestyl 15mg/kg load over 30 minutes then 2-6mg/min gtt
- Ventricular Tachycardia with active ischemia
- Lidocaine 1 mg/kg q5-10 min up to 3 times then 2-6mg.min gtt
- If unsuccessful, Pronestyl as above
- If unsuccessful, IV Amiodarone 150-300 load over 15-20min. 30-60mg/hr gtt for total of 1gram
- Ventricular Tachycardia in Setting of Cardiomyopathy
- Positively SVT with aberrancy
- Antidromic AVRT
- Etiology Uncertain
References
- ↑ Brugada P, Brugada J, Mont L et al. A new approach to the differential diagnosis of a regular tachycardia with wide QRS complex. Circulation. 1991;83: 1649-1659. PMID 2022022
- ↑ Kindwall KE, Brown, J, Josephson ME. Electrocardiographic criteria for ventricular tachycardia in wide complex left bundle branch block morphology tachycardias. Am J Cardiology. 1988; 61:1279-1283. PMID 3376886
- ↑ Podrid P, Brugada P. Approach to wide QRS complex tachycardias. Up To Date. 1998.