Sandbox:Affan: Difference between revisions
Jump to navigation
Jump to search
No edit summary |
No edit summary |
||
| Line 622: | Line 622: | ||
{| class="wikitable" | {| class="wikitable" | ||
|+ | |+ | ||
! colspan=" | ! colspan="6" style="background:#4479BA; color: #FFFFFF;" align="center" + |Soft tissue oral lesions | ||
|- | |- | ||
! rowspan="1" style="background:#4479BA; color: #FFFFFF;" align="center" + |Reactive lesions | ! rowspan="1" style="background:#4479BA; color: #FFFFFF;" align="center" + |Reactive lesions | ||
! rowspan="1" style="background:#4479BA; color: #FFFFFF;" align="center" + |Symptoms | ! rowspan="1" style="background:#4479BA; color: #FFFFFF;" align="center" + |Symptoms | ||
! rowspan="1" style="background:#4479BA; color: #FFFFFF;" align="center" + |Characterstic features | ! rowspan="1" style="background:#4479BA; color: #FFFFFF;" align="center" + |Characterstic features | ||
! rowspan="1" style="background:#4479BA; color: #FFFFFF;" align="center" + |Associated conditions | ! rowspan="1" style="background:#4479BA; color: #FFFFFF;" align="center" + |Associated conditions | ||
| Line 634: | Line 633: | ||
| rowspan="1" style="background: #DCDCDC; padding: 5px; text-align: center;" | | | rowspan="1" style="background: #DCDCDC; padding: 5px; text-align: center;" | | ||
* Leukoedema | * Leukoedema | ||
| | | | ||
| | | | ||
| Line 642: | Line 640: | ||
| style="background: #DCDCDC; padding: 5px; text-align: center;" | | | style="background: #DCDCDC; padding: 5px; text-align: center;" | | ||
* Fordyce granules | * Fordyce granules | ||
| | | | ||
| | | | ||
| Line 650: | Line 647: | ||
| style="background: #DCDCDC; padding: 5px; text-align: center;" | | | style="background: #DCDCDC; padding: 5px; text-align: center;" | | ||
* Hairy tongue | * Hairy tongue | ||
| | | | ||
| | | | ||
| Line 658: | Line 654: | ||
| style="background: #DCDCDC; padding: 5px; text-align: center;" | | | style="background: #DCDCDC; padding: 5px; text-align: center;" | | ||
* Hairy leukoplakia | * Hairy leukoplakia | ||
| | | | ||
| | | | ||
| Line 666: | Line 661: | ||
| style="background: #DCDCDC; padding: 5px; text-align: center;" | | | style="background: #DCDCDC; padding: 5px; text-align: center;" | | ||
* White sponge nevus | * White sponge nevus | ||
| | | | ||
| | | | ||
| Line 674: | Line 668: | ||
| style="background: #DCDCDC; padding: 5px; text-align: center;" | | | style="background: #DCDCDC; padding: 5px; text-align: center;" | | ||
* Lichen planus | * Lichen planus | ||
| | | | ||
| | | | ||
| Line 683: | Line 676: | ||
* Focal keratosis | * Focal keratosis | ||
| | | | ||
| | | | ||
| | | | ||
| | | | ||
|- | |- | ||
! colspan=" | ! colspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" + |Tumors | ||
! rowspan="1" style="background:#4479BA; color: #FFFFFF;" align="center" + |etiology | ! rowspan="1" style="background:#4479BA; color: #FFFFFF;" align="center" + |etiology | ||
! rowspan="1" style="background:#4479BA; color: #FFFFFF;" align="center" + |location | ! rowspan="1" style="background:#4479BA; color: #FFFFFF;" align="center" + |location | ||
| Line 695: | Line 687: | ||
! rowspan="1" style="background:#4479BA; color: #FFFFFF;" align="center" + |Image | ! rowspan="1" style="background:#4479BA; color: #FFFFFF;" align="center" + |Image | ||
|- | |- | ||
| rowspan=" | | rowspan="3" |Epithelial tumors | ||
| rowspan=" | | | ||
* | * Squamous cell carcinoma | ||
| | |||
| | |||
| | |||
| | |||
| | |||
|- | |||
| | |||
* Oral epithelial dysplasia | |||
| | |||
| | |||
| | |||
| | |||
| | |||
|- | |||
| | |||
* Proliferative verrucous leukoplakia | |||
| | |||
| | |||
| | |||
| | |||
| | |||
|- | |||
| rowspan="3" |Papillomas | |||
| | |||
* Condyloma acuminatum | |||
| | |||
| | |||
| | |||
| | |||
| | |||
|- | |||
| | |||
* Verrucous vulgaris | |||
| | |||
| | |||
| | |||
| | |||
| | |||
|- | |||
| | |||
* Multifocal epithelial hyperplasia | |||
| | |||
| | |||
| | |||
| | |||
| | |||
|- | |||
| rowspan="2" |Salivary type tumors | |||
| | |||
* Mucoepidermoid carcinoma | |||
| | |||
| | |||
| | |||
| | |||
| | |||
|- | |||
| | |||
* Pleomorphic adenoma | |||
| | |||
| | |||
| | |||
| | |||
| | |||
|- | |||
| rowspan="8" |Soft tissue and Neural tumors | |||
| | |||
* Granular cell tumor | |||
| | |||
| | |||
| | |||
| | |||
| | |||
|- | |||
| | |||
* Rhabdomyoma | |||
| | |||
| | |||
| | |||
| | |||
| | |||
|- | |||
| | |||
* Lymphangioma | |||
| | | | ||
| | | | ||
| | | | ||
| Line 706: | Line 780: | ||
|- | |- | ||
| | | | ||
* | * Hemangioma | ||
| | |||
| | | | ||
| | | | ||
| Line 713: | Line 788: | ||
|- | |- | ||
| | | | ||
* | * Schwannoma | ||
| | |||
| | | | ||
| | | | ||
| Line 719: | Line 795: | ||
| | | | ||
|- | |- | ||
| | | | ||
* | * Neurofibroma | ||
| | |||
| | |||
| | |||
| | |||
| | |||
|- | |||
| | |||
* Kaposi sarcoma | |||
| | |||
| | |||
| | |||
| | |||
| | |||
|- | |||
| | |||
* Myofibroblastic sarcoma | |||
| | |||
| | |||
| | |||
| | |||
| | |||
|- | |||
| rowspan="4" |Hematolymphoid tumors | |||
| | |||
* CD-30 positive lymphoproliferative disorder | |||
| | | | ||
| | | | ||
| Line 727: | Line 828: | ||
| | | | ||
|- | |- | ||
| | |||
* | * Plasmablastic lymphoma | ||
| | | | ||
| | | | ||
| Line 735: | Line 836: | ||
| | | | ||
|- | |- | ||
| | |||
* Langerhan cell histiocytosis | |||
* | |||
| | | | ||
| | | | ||
| Line 744: | Line 844: | ||
| | | | ||
|- | |- | ||
| | |||
* | * Extramedullary myeloid sarcoma | ||
| | | | ||
| | | | ||
| Line 752: | Line 852: | ||
| | | | ||
|- | |- | ||
| | | rowspan="2" |Tumors of uncertain histiogenesis | ||
* | | | ||
* Congenital granular cell epulis | |||
| | | | ||
| | | | ||
| Line 760: | Line 861: | ||
| | | | ||
|- | |- | ||
| | |||
* | * Ectomesenchymal chondromyxoid tumor | ||
| | | | ||
| | | | ||
| Line 771: | Line 872: | ||
| style="background: #DCDCDC; padding: 5px; text-align: center;" | | | style="background: #DCDCDC; padding: 5px; text-align: center;" | | ||
* Gingival cyst | * Gingival cyst | ||
| | | | ||
| | | | ||
| Line 779: | Line 879: | ||
| style="background: #DCDCDC; padding: 5px; text-align: center;" | | | style="background: #DCDCDC; padding: 5px; text-align: center;" | | ||
* Lymphoepithelial cyst | * Lymphoepithelial cyst | ||
| | | | ||
| | | | ||
| Line 787: | Line 886: | ||
| style="background: #DCDCDC; padding: 5px; text-align: center;" | | | style="background: #DCDCDC; padding: 5px; text-align: center;" | | ||
* Epidermoid cyst | * Epidermoid cyst | ||
| | | | ||
| | | | ||
| Line 795: | Line 893: | ||
| style="background: #DCDCDC; padding: 5px; text-align: center;" | | | style="background: #DCDCDC; padding: 5px; text-align: center;" | | ||
* Thyroglossal tract cyst | * Thyroglossal tract cyst | ||
| | | | ||
| | | | ||
| Line 803: | Line 900: | ||
| style="background: #DCDCDC; padding: 5px; text-align: center;" | | | style="background: #DCDCDC; padding: 5px; text-align: center;" | | ||
* Nasolabial cyst | * Nasolabial cyst | ||
| | | | ||
| | | | ||
Revision as of 21:52, 11 February 2019
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Muhammad Affan M.D.[2]
| Surface oral lesions | |||||||
|---|---|---|---|---|---|---|---|
| Oral lesions | Appearance | Associated conditions | Location | Microscopic | Image | ||
| White Lesions | Leukoedema |
|
|
|
|

| |
| Fordyce granules |
|
|
|
|
 | ||
| Benign migratoy glossitis |
|
|
|
|
 | ||
| Hairy tongue |
|
|
|
|
 | ||
| Hairy leukoplakia |
White patches
|
|
|
|

| ||
| White sponge nevus |
|
|
|
||||
| Lichen Planus |
|
|
|
|
 | ||
| Frictional hyperkeratosis |
|
|
|
|
 | ||
| Leukoplakia |
|
|
|
|
 | ||
| Erythroplakia |
|
|
|
|
 | ||
| Oral lesions | Characterestic features | Associated conditions | Location | Microscopic | Image | ||
| Pigmented lesions |
|
|
|
|
|
 | |
|
|
|
|
||||
|
|
|
 | ||||
|
|
|
|
|
 | ||
|
|
|
|
|
 | ||
|
|
|
|
 | |||
|
|
|
|
 | |||
|
|
Intraorally |
|
 | |||
|
|
|
|
||||
|
|
|
|||||
|
|
|
|
 | |||
| Oral lesions | Characteristic features | Associated conditions | Location | Microscopic | Image | ||
| Vesicular/
Ulcerative |
Infections | Herpes simplex virusinfections |
|
|
|
 | |
| Herpes zoster |
|
|
|
 | |||
| Hand foot mouth disease |
|
|
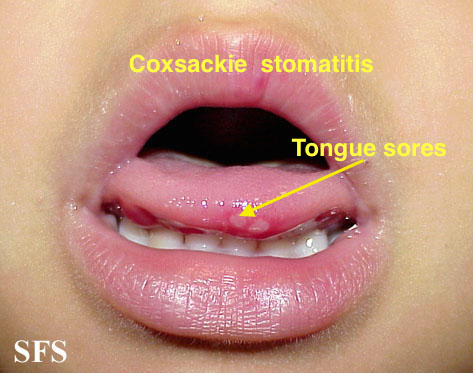 | ||||
| Infectious mononucliosis |
|
||||||
| Erosive lichen planus |
|
||||||
| Pseudomembranous candidiasis |
|
||||||
| Histoplasmosis |
|
|
|||||
| Blastomycosis |
|
|
|||||
| Coccidiodomycosis |
|
||||||
| Autoimmune conditions | Pemphigus vulgaris |
|
|
||||
| Mucous membrane pemphigoid (Cicatricial pemphigoid) |
|
||||||
| Aphthous ulcer |
|
||||||
| Erythema multiforme |
|
||||||
| Sjogren's Syndrome |
Affects salivary and lacrimal glands
|
||||||
| Bullous pemphigoid |
|
||||||
| Idiopathic conditions | Allergic contact stomatitis |
|
|
||||
| Irritant contact stomatitis | |||||||
| Soft tissue oral lesions | ||||||
|---|---|---|---|---|---|---|
| Reactive lesions | Symptoms | Characterstic features | Associated conditions | Location | Image | |
|
||||||
|
||||||
|
||||||
|
||||||
|
||||||
|
||||||
|
||||||
| Tumors | etiology | location | Clinical appearance | Gold standard/Diagnosis | Image | |
| Epithelial tumors |
|
|||||
|
||||||
|
||||||
| Papillomas |
|
|||||
|
||||||
|
||||||
| Salivary type tumors |
|
|||||
|
||||||
| Soft tissue and Neural tumors |
|
|||||
|
||||||
|
||||||
|
||||||
|
||||||
|
||||||
|
||||||
|
||||||
| Hematolymphoid tumors |
|
|||||
|
||||||
|
||||||
|
||||||
| Tumors of uncertain histiogenesis |
|
|||||
|
||||||
| Cysts |
|
|||||
|
||||||
|
||||||
|
||||||
|
||||||