Cirrhosis physical examination: Difference between revisions
Jump to navigation
Jump to search
No edit summary |
No edit summary |
||
| Line 6: | Line 6: | ||
Many signs and symptoms may occur in the presence of cirrhosis or as a result of the complications or causes of cirrhosis. Many are nonspecific and may occur in other diseases and do not necessarily point to cirrhosis. Likewise, the absence of any sign or symptom does not rule out the possibility of cirrhosis. | Many signs and symptoms may occur in the presence of cirrhosis or as a result of the complications or causes of cirrhosis. Many are nonspecific and may occur in other diseases and do not necessarily point to cirrhosis. Likewise, the absence of any sign or symptom does not rule out the possibility of cirrhosis. | ||
==Physical Examination== | |||
*Physical examination of [[Patient|patients]] with [[cirrhosis]] is usually remarkable for: [[jaundice]], [[Spider angioma|spider angiomata]], [[ascites]], [[asterixis]], [[Splenomegaly|spleenomegaly]] and [[palmar erythema]]. | |||
===Appearance of the Patient=== | |||
*[[Patient|Patients]] with [[cirrhosis]] usually appear weak due to constitutional [[Symptom|symptoms]] such as [[weight loss]], [[anorexia]] and [[muscle atrophy]]. Yellowish discoloration of [[skin]] and [[abdominal distension]] may also be present due to [[ascites]]. | |||
*Normal/low [[blood pressure]] with normal [[pulse pressure]]. | |||
===Skin=== | |||
*[[Jaundice]] : yellow discoloration of the skin, eyes, and mucus membranes due to increased [[bilirubin]] (at least 2-3 mg/dL or 30 mmol/L). Urine may also appear dark. | |||
*[[Pallor]] | |||
*[[Bruise|Bruises]] | |||
*[[Palmar erythema]] on the [[Thenar eminence|thenar]] and [[Hypothenar eminence|hypothenar eminences]], due to altered sex hormone metabolism. | |||
*[[Spider angioma|Spider angiomata]]: Increased estradiol levels lead to the formation of vascular lesions consisting of central arterioles surrounded by smaller vessels <ref name="pmid10423070">{{cite journal |author=Li CP, Lee FY, Hwang SJ, ''et al'' |title=Spider angiomas in patients with liver cirrhosis: role of alcoholism and impaired liver function|journal=Scand. J. Gastroenterol. |volume=34 |issue=5 |pages=520-3 |year=1999 |pmid=10423070 |doi=}}</ref> | |||
*'''[[Telangiectasia|Telangiectasias]]''' or '''spider veins:''' small dilated [[blood vessel]]s near the surface of the [[skin]]. | |||
===HEENT=== | |||
* Abnormalities of the head/hair may include thinning of hair on the scalp due to [[hyperestrogenism]] | |||
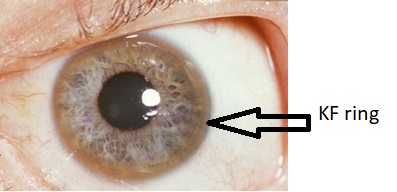
* '''[[Kayser-Fleischer ring]]s''' : dark rings that appear to encircle the [[iris (anatomy)|iris]] of the [[eye]] in [[Patient|patients]] with [[Wilson's disease]]. | |||
* [[Parotid gland]] enlargement | |||
* [[Fetor hepaticus]]: severe portal-systemic shunting leads to increased levels of [[dimethyl sulfide]] leads to a sweet pungent smell in the breath | |||
===Abdomen=== | |||
* Inspection: | |||
** [[Abdominal distension]] | |||
** [[Caput medusae]] | |||
* Palpation: | |||
** Fluid wave | |||
** [[Hepatomegaly]] may be present in initial stages. The liver may also be normal or shrunken. | |||
** [[Splenomegaly|Spleenomegaly]] may be present in patients with [[cirrhosis]] from nonalcoholic etiologies, due to portal hypertension | |||
* Percussion: | |||
** Flank dullness may be present due to [[ascites]] (needs approximately 1500ml for detection) | |||
* Auscultation: | |||
** [[Cruveilhier-Baumgarten murmur]]: venous hum that may be present in patients with [[portal hypertension]]. | |||
*** Mechanism: due to collateral connections between remnant of the [[umbilical vein]] and the [[Portal venous system|portal system]] | |||
*** Location: [[Epigastrium]] | |||
*** Exacerbating factors: [[Valsalva maneuver]] | |||
*** Diminished by: application of [[pressure]] on the [[skin]] above the [[Navel|umbilicus]] | |||
===Genitourinary=== | |||
*[[Testicular atrophy]] | |||
*Inversion of the normal male [[pubic hair]] pattern | |||
===Neuromuscular=== | |||
* [[Hepatic encephalopathy]] may have signs of: | |||
** Alteration of [[Mental status examination|mental status]] | |||
** [[Confusion]] | |||
** [[Coma]] | |||
* [[Asterixis]] (bilateral but asynchronous flapping motions of outstretched, dorsiflexed hands) is seen in patients with [[hepatic encephalopathy]]. | |||
===Extremities=== | |||
*[[edema]] of the lower extremities | |||
*[[Muscle atrophy]] | |||
*Nail changes: | |||
**Muehrcke nails: paired horizontal white bands separated by normal color due to [[hypoalbuminemia]] | |||
**Terry nails: the proximal two-thirds of the nail plate appears white, whereas the distal one-third is red due to [[hypoalbuminemia]] | |||
** [[Clubbing]]: the angle between the nail plate and proximal nail fold is greater than 180 degrees | |||
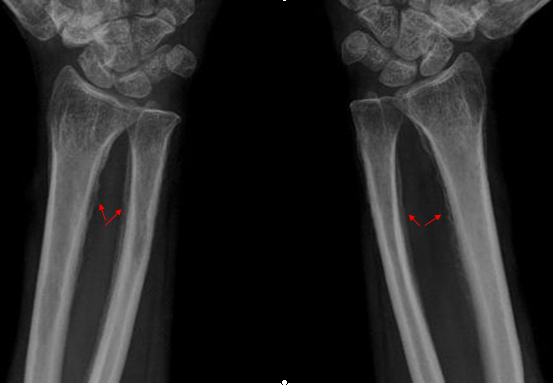
**Severe [[clubbing]]: | |||
***"Drum stick" appearance of distal fingers | |||
***[[Hypertrophic pulmonary osteoarthropathy|Hypertrophic osteoarthropathy]]: chronic proliferative [[periostitis]] of the [[long bones]] | |||
**[[Dupuytrens contracture|Dupuytren's contracture]] may cause flexion deformities of the fingers: This occurs due to shortening and thickening of the palmar fascia, due to collagen deposition and fibroblastic proliferation. | |||
**[[Asterixis]] in cases with [[hepatic encephalopathy]] | |||
=== Chest findings === | |||
* [[Gynecomastia]]: due to increased estradiol levels | |||
* Loss of chest or [[Underarm hair|axillary hair]] | |||
===Other findings=== | |||
* [[Hemorrhoids]] | |||
* [[Hematemesis]] | |||
* [[Melena]] | |||
==Physical Examination== | ==Physical Examination== | ||
Revision as of 17:45, 7 December 2017
|
Cirrhosis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case studies |
|
Cirrhosis physical examination On the Web |
|
American Roentgen Ray Society Images of Cirrhosis physical examination |
|
Risk calculators and risk factors for Cirrhosis physical examination |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Aditya Govindavarjhulla, M.B.B.S. [2]
Overview
Many signs and symptoms may occur in the presence of cirrhosis or as a result of the complications or causes of cirrhosis. Many are nonspecific and may occur in other diseases and do not necessarily point to cirrhosis. Likewise, the absence of any sign or symptom does not rule out the possibility of cirrhosis.
Physical Examination
- Physical examination of patients with cirrhosis is usually remarkable for: jaundice, spider angiomata, ascites, asterixis, spleenomegaly and palmar erythema.
Appearance of the Patient
- Patients with cirrhosis usually appear weak due to constitutional symptoms such as weight loss, anorexia and muscle atrophy. Yellowish discoloration of skin and abdominal distension may also be present due to ascites.
- Normal/low blood pressure with normal pulse pressure.
Skin
- Jaundice : yellow discoloration of the skin, eyes, and mucus membranes due to increased bilirubin (at least 2-3 mg/dL or 30 mmol/L). Urine may also appear dark.
- Pallor
- Bruises
- Palmar erythema on the thenar and hypothenar eminences, due to altered sex hormone metabolism.
- Spider angiomata: Increased estradiol levels lead to the formation of vascular lesions consisting of central arterioles surrounded by smaller vessels [1]
- Telangiectasias or spider veins: small dilated blood vessels near the surface of the skin.
HEENT
- Abnormalities of the head/hair may include thinning of hair on the scalp due to hyperestrogenism
- Kayser-Fleischer rings : dark rings that appear to encircle the iris of the eye in patients with Wilson's disease.
- Parotid gland enlargement
- Fetor hepaticus: severe portal-systemic shunting leads to increased levels of dimethyl sulfide leads to a sweet pungent smell in the breath
Abdomen
- Inspection:
- Palpation:
- Fluid wave
- Hepatomegaly may be present in initial stages. The liver may also be normal or shrunken.
- Spleenomegaly may be present in patients with cirrhosis from nonalcoholic etiologies, due to portal hypertension
- Percussion:
- Flank dullness may be present due to ascites (needs approximately 1500ml for detection)
- Auscultation:
- Cruveilhier-Baumgarten murmur: venous hum that may be present in patients with portal hypertension.
- Mechanism: due to collateral connections between remnant of the umbilical vein and the portal system
- Location: Epigastrium
- Exacerbating factors: Valsalva maneuver
- Diminished by: application of pressure on the skin above the umbilicus
- Cruveilhier-Baumgarten murmur: venous hum that may be present in patients with portal hypertension.
Genitourinary
- Testicular atrophy
- Inversion of the normal male pubic hair pattern
Neuromuscular
- Hepatic encephalopathy may have signs of:
- Alteration of mental status
- Confusion
- Coma
- Asterixis (bilateral but asynchronous flapping motions of outstretched, dorsiflexed hands) is seen in patients with hepatic encephalopathy.
Extremities
- edema of the lower extremities
- Muscle atrophy
- Nail changes:
- Muehrcke nails: paired horizontal white bands separated by normal color due to hypoalbuminemia
- Terry nails: the proximal two-thirds of the nail plate appears white, whereas the distal one-third is red due to hypoalbuminemia
- Clubbing: the angle between the nail plate and proximal nail fold is greater than 180 degrees
- Severe clubbing:
- "Drum stick" appearance of distal fingers
- Hypertrophic osteoarthropathy: chronic proliferative periostitis of the long bones
- Dupuytren's contracture may cause flexion deformities of the fingers: This occurs due to shortening and thickening of the palmar fascia, due to collagen deposition and fibroblastic proliferation.
- Asterixis in cases with hepatic encephalopathy
Chest findings
- Gynecomastia: due to increased estradiol levels
- Loss of chest or axillary hair
Other findings
Physical Examination
Skin
| RT-8OzD9j00}} | -fTGzcsygBI}} |


 |
 |
Eyes
Abdomen
{{#ev:youtube|CHUBTgrU3Oc}}



{{#ev:youtube|Or65nOrcz1A}}