Mivacurium chloride: Difference between revisions
No edit summary |
No edit summary |
||
| Line 26: | Line 26: | ||
|adverseReactions= | |adverseReactions= | ||
[[flushing]] | |||
<!--Black Box Warning--> | <!--Black Box Warning--> | ||
Revision as of 20:57, 18 February 2015
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Vignesh Ponnusamy, M.B.B.S. [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
Mivacurium chloride is a short-acting, nondepolarizing skeletal muscle relaxant that is FDA approved for the {{{indicationType}}} of induction of neuromuscular blockade. Common adverse reactions include flushing.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Induction of Neuromuscular Blockade
- MIVACRON is a short-acting neuromuscular blocking agent indicated for inpatients and outpatients, as an adjunct to general anesthesia, to facilitate tracheal intubation and to provide skeletal muscle relaxation during surgery or mechanical ventilation.
- Initial Doses
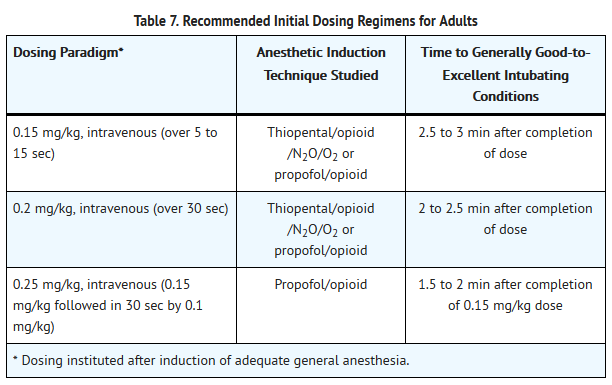
- Doses of 0.15 mg/kg administered over 5 to 15 seconds, 0.2 mg/kg administered over 30 seconds, or 0.25 mg/kg administered in divided doses (0.15 mg/kg followed in 30 seconds by 0.1 mg/kg) are recommended for facilitation of tracheal intubation for most patients (see Table 7).
- The purpose of slowed or divided dosing of MIVACRON at doses above 0.15 mg/kg is to minimize the transient decreases in blood pressure observed in some patients given these doses over 5 to 15 seconds. The quality of intubation conditions does not significantly differ for the times and doses of MIVACRON recommended in Table 7, but the onset of suitable intubation conditions may be reached earlier with higher doses. The choice of a particular dose and regimen should be based on individual circumstances and patient requirements.
- In patients with clinically significant cardiovascular disease and in patients with any history suggesting a greater sensitivity to the release of histamine or other mediators (e.g., asthma), the dose of MIVACRON should be 0.15 mg/kg or less, administered over 60 seconds. No data are available on the use of doses of MIVACRON above 0.15 mg/kg in patients with clinically significant kidney or liver disease.
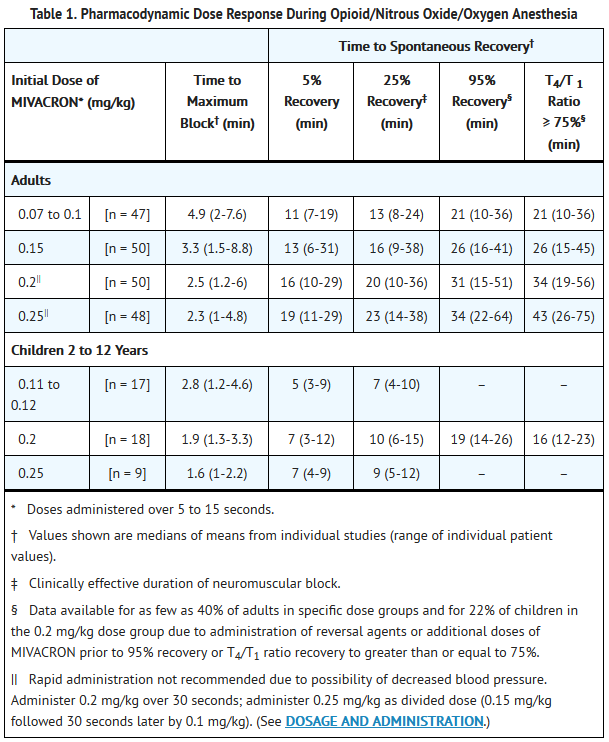
- Clinically effective neuromuscular block may be expected to last for 15 to 20 minutes (range: 9 to 38 minutes) and spontaneous recovery may be expected to be 95% complete in 25 to 30 minutes (range: 16 to 41 minutes) following 0.15 mg/kg MIVACRON administered to patients receiving opioid/nitrous oxide/oxygen anesthesia. The expected duration of clinically effective block and time to 95% spontaneous recovery following 0.2 mg/kg MIVACRON are approximately 20 and 30 minutes, respectively, and following 0.25 mg/kg MIVACRON are approximately 25 and 35 minutes. Initiation of maintenance dosing during opioid/nitrous oxide/oxygen anesthesia is generally required approximately 15, 20 and 25 minutes following initial doses of 0.15 mg/kg, 0.2 mg/kg, and 0.25 mg/kg MIVACRON, respectively (see Table 1). Maintenance doses of 0.1 mg/kg each provide approximately 15 minutes of additional clinically effective block. For shorter or longer durations of action, smaller or larger maintenance doses may be administered.
- The neuromuscular blocking action of MIVACRON is potentiated by isoflurane or enflurane anesthesia. Recommended initial doses of MIVACRON may be used to facilitate tracheal intubation prior to the administration of these agents; however, if MIVACRON is first administered after establishment of stable-state isoflurane or enflurane anesthesia (administered with nitrous oxide/oxygen to achieve 1.25 MAC), the initial dose of MIVACRON may be reduced by as much as 25%. Greater reductions in the dose of MIVACRON may be required with higher concentrations of enflurane or isoflurane. With halothane, which has only a minimal potentiating effect on MIVACRON, a smaller dosage reduction may be considered.
- Continuous Infusion
- Continuous infusion of MIVACRON may be used to maintain neuromuscular block. Upon early evidence of spontaneous recovery from an initial dose, an initial infusion rate of 9 to 10 mcg/kg/min is recommended. If continuous infusion is initiated simultaneously with the administration of an initial dose, a lower initial infusion rate should be used (e.g., 4 mcg/kg/min). In either case, the initial infusion rate should be adjusted according to the response to peripheral nerve stimulation and to clinical criteria. On average, an infusion rate of 5 to 7 mcg/kg/min (range: 1 to 15 mcg/kg/min) may be expected to maintain neuromuscular block within the range of 89% to 99% for extended periods in adults receiving opioid/nitrous oxide/oxygen anesthesia. In some patients, particularly those with higher infusion requirements (greater than 8 mcg/kg/min) during the first 30 minutes, the infusion rate required to maintain 89% to 99% T1 suppression may decrease gradually (by greater than or equal to 30%) with time over a 4- to 6-hour period of infusion. Reduction of the infusion rate by up to 35% to 40% should be considered when MIVACRON is administered during stable-state conditions of isoflurane or enflurane anesthesia (administered with nitrous oxide/oxygen to achieve 1.25 MAC). Greater reductions in the infusion rate of MIVACRON may be required with greater concentrations of enflurane or isoflurane. With halothane, smaller reductions in infusion rate may be required.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Mivacurium chloride in adult patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Mivacurium chloride in adult patients.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
Induction of Neuromuscular Blockade
- MIVACRON is a short-acting neuromuscular blocking agent indicated for inpatients and outpatients, as an adjunct to general anesthesia, to facilitate tracheal intubation and to provide skeletal muscle relaxation during surgery or mechanical ventilation.
- Initial Doses
- Dosage requirements for MIVACRON on a mg/kg basis are higher in children than in adults. Onset and recovery of neuromuscular block occur more rapidly in children than in adults.
- The recommended dose of MIVACRON for facilitating tracheal intubation in children 2 to 12 years of age is 0.2 mg/kg administered over 5 to 15 seconds. When administered during stable opioid/nitrous oxide/oxygen anesthesia, 0.2 mg/kg of MIVACRON produces maximum neuromuscular block in an average of 1.9 minutes (range: 1.3 to 3.3 minutes) and clinically effective block for 10 minutes (range: 6 to 15 minutes). Maintenance doses are generally required more frequently in children than in adults. Administration of doses of MIVACRON above the recommended range (greater than 0.2 mg/kg) is associated with transient decreases in MAP in some children. MIVACRON has not been studied in pediatric patients below the age of 2 years.
- Continuous Infusion
- Children require higher infusion rates of MIVACRON than adults. During opioid/nitrous oxide/oxygen anesthesia, the infusion rate required to maintain 89% to 99% neuromuscular block averages 14 mcg/kg/min (range: 5 to 31 mcg/kg/min). The principles for infusion of MIVACRON in adults are also applicable to children (see above).
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Mivacurium chloride in pediatric patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Mivacurium chloride in pediatric patients.
Contraindications
- MIVACRON is contraindicated in patients with known hypersensitivity to the product and its components.
Warnings
- Anaphylaxis
- Severe anaphylactic reactions to neuromuscular blocking agents, including MIVACRON, have been reported. These reactions have in some cases been life-threatening and fatal. Due to the potential severity of these reactions, the necessary precautions, such as the immediate availability of appropriate emergency treatment, should be taken. Precautions should also be taken in those individuals who have had previous anaphylactic reactions to other neuromuscular blocking agents since cross-reactivity between neuromuscular blocking agents, both depolarizing and non-depolarizing, has been reported in this class of drugs.
- Administration
- MIVACRON should be administered in carefully adjusted dosage by or under the supervision of experienced clinicians who are familiar with the drug's actions and the possible complications of its use. The drug should not be administered unless personnel and facilities for resuscitation and life support (tracheal intubation, artificial ventilation, oxygen therapy), and an antagonist of MIVACRON are immediately available. It is recommended that a peripheral nerve stimulator be used to measure neuromuscular function during the administration of MIVACRON in order to monitor drug effect, determine the need for additional drug, and confirm recovery from neuromuscular block.
- MIVACRON has no known effect on consciousness, pain threshold, or cerebration. To avoid distress to the patient, neuromuscular block should not be induced before unconsciousness.
- MIVACRON is metabolized by plasma cholinesterase and should be used with great caution, if at all, in patients known to be or suspected of being homozygous for the atypical plasma cholinesterase gene.
- MIVACRON Injection is acidic (pH 3.5 to 5) and may not be compatible with alkaline solutions having a pH greater than 8.5 (e.g., barbiturate solutions).
Precautions
- General
- Although MIVACRON (a mixture of three stereoisomers) is not a potent histamine releaser, the possibility of substantial histamine release must be considered. Release of histamine is related to the dose and speed of injection.
- Caution should be exercised in administering MIVACRON to patients with clinically significant cardiovascular disease and patients with any history suggesting a greater sensitivity to the release of histamine or related mediators (e.g., asthma). In such patients, the initial dose of MIVACRON should be 0.15 mg/kg or less, administered over 60 seconds; assurance of adequate hydration and careful monitoring of hemodynamic status are important (see CLINICAL PHARMACOLOGY - Hemodynamics and Individualization of Dosages).
- Obese patients may be more likely to experience clinically significant transient decreases in MAP than non-obese patients when the dose of MIVACRON is based on actual rather than ideal body weight. Therefore, in obese patients, the initial dose should be determined using the patient's ideal body weight.
- Recommended doses of MIVACRON have no clinically significant effects on heart rate; therefore, MIVACRON will not counteract the bradycardia produced by many anesthetic agents or by vagal stimulation.
- Neuromuscular blocking agents may have a profound effect in patients with neuromuscular diseases (e.g., myasthenia gravis and the myasthenic syndrome). In these and other conditions in which prolonged neuromuscular block is a possibility (e.g., carcinomatosis), the use of a peripheral nerve stimulator and a dose of not more than 0.015 to 0.02 mg/kg MIVACRON is recommended to assess the level of neuromuscular block and to monitor dosage requirements.
- MIVACRON has not been studied in patients with burns. Resistance to nondepolarizing neuromuscular blocking agents may develop in patients with burns, depending upon the time elapsed since the injury and the size of the burn. Patients with burns may have reduced plasma cholinesterase activity which may offset this resistance.
- Acid-base and/or serum electrolyte abnormalities may potentiate or antagonize the action of neuromuscular blocking agents. The action of neuromuscular blocking agents may be enhanced by magnesium salts administered for the management of toxemia of pregnancy.
- No data are available to support the use of MIVACRON by intramuscular injection.
- Allergic Reactions
- Since allergic cross-reactivity has been reported in this class, request information from your patients about previous anaphylactic reactions to other neuromuscular blocking agents. In addition, inform your patients that severe anaphylactic reactions to neuromuscular blocking agents, including MIVACRON have been reported.
- Renal and Hepatic Disease
- The possibility of prolonged neuromuscular block must be considered when MIVACRON is used in patients with renal or hepatic disease. Most patients with chronic hepatic disease such as hepatitis, liver abscess, and cirrhosis of the liver exhibit a marked reduction in plasma cholinesterase activity. Patients with acute or chronic renal disease may also show a reduction in plasma cholinesterase activity .
- Reduced Plasma Cholinesterase Activity
- The possibility of prolonged neuromuscular block following administration of MIVACRON must be considered in patients with reduced plasma cholinesterase (pseudocholinesterase) activity.
- Plasma cholinesterase activity may be diminished in the presence of genetic abnormalities of plasma cholinesterase (e.g., patients heterozygous or homozygous for the atypical plasma cholinesterase gene), pregnancy, liver or kidney disease, malignant tumors, infections, burns, anemia, decompensated heart disease, peptic ulcer, or myxedema. Plasma cholinesterase activity may also be diminished by chronic administration of oral contraceptives, glucocorticoids, or certain monoamine oxidase inhibitors and by irreversible inhibitors of plasma cholinesterase (e.g., organophosphate insecticides, echothiophate, and certain antineoplastic drugs).
- MIVACRON has been used safely in patients heterozygous for the atypical plasma cholinesterase gene. At doses of 0.1 to 0.2 mg/kg MIVACRON, the clinically effective duration of action was 8 minutes to 11 minutes longer in patients heterozygous for the atypical gene than in genotypically normal patients.
- As with succinylcholine, patients homozygous for the atypical plasma cholinesterase gene (one in 2500 patients) are extremely sensitive to the neuromuscular blocking effect of MIVACRON. In three such adult patients, a small dose of 0.03 mg/kg (approximately the ED10-20 in genotypically normal patients) produced complete neuromuscular block for 26 to 128 minutes. Once spontaneous recovery had begun, neuromuscular block in these patients was antagonized with conventional doses of neostigmine. One adult patient, who was homozygous for the atypical plasma cholinesterase gene, received a dose of 0.18 mg/kg MIVACRON and exhibited complete neuromuscular block for about 4 hours. Response to post-tetanic stimulation was present after 4 hours, all four responses to train-of-four stimulation were present after 6 hours, and the patient was extubated after 8 hours. Reversal was not attempted in this patient.
- Malignant Hyperthermia (MH)
- In a study of MH-susceptible pigs, MIVACRON did not trigger MH. MIVACRON has not been studied in MH-susceptible patients. Because MH can develop in the absence of established triggering agents, the clinician should be prepared to recognize and treat MH in any patient undergoing general anesthesia.
- Long-Term Use in the Intensive Care Unit (ICU)
- No data are available on the long-term use of MIVACRON in patients undergoing mechanical ventilation in the ICU.
Adverse Reactions
Clinical Trials Experience
- MIVACRON (a mixture of three stereoisomers) was well tolerated during extensive clinical trials in inpatients and outpatients. Prolonged neuromuscular block, which is an important adverse experience associated with neuromuscular blocking agents as a class, was reported as an adverse experience in three of 2074 patients administered MIVACRON. The most commonly reported adverse experience following the administration of MIVACRON was transient, dose-dependent cutaneous flushing about the face, neck, and/or chest. Flushing was most frequently noted after the initial dose of MIVACRON and was reported in about 25% of adult patients who received 0.15 mg/kg MIVACRON over 5 to 15 seconds. When present, flushing typically began within 1 to 2 minutes after the dose of MIVACRON and lasted for 3 to 5 minutes. Of 105 patients who experienced flushing after 0.15 mg/kg MIVACRON, two patients also experienced mild hypotension that was not treated, and one patient experienced moderate wheezing that was successfully treated.
- Overall, hypotension was infrequently reported as an adverse experience in the clinical trials of MIVACRON. One of 332 (0.3%) healthy adults who received 0.15 mg/kg MIVACRON over 5 to 15 seconds and none of 37 cardiac surgery patients who received 0.15 mg/kg MIVACRON over 60 seconds were treated for a decrease in blood pressure in association with the administration of MIVACRON. One to two percent of healthy adults given greater than or equal to 0.2 mg/kg MIVACRON over 5 to 15 seconds, 2% to 3% of healthy adults given 0.2 mg/kg over 30 seconds, none of 100 healthy adults given 0.25 mg/kg as a divided dose (0.15 mg/kg followed in 30 seconds by 0.1 mg/kg), and 2% to 4% of cardiac surgery patients given greater than or equal to 0.2 mg/kg over 60 seconds were treated for a decrease in blood pressure. None of the 63 children who received the recommended dose of 0.2 mg/kg MIVACRON was treated for a decrease in blood pressure in association with the administration of MIVACRON.
- The following adverse experiences were reported in patients administered MIVACRON (all events judged by investigators during the clinical trials to have a possible causal relationship):
- Incidence Greater Than 1%
Cardiovascular
Flushing (16%)
- Incidence Less Than 1%
Cardiovascular
Hypotension, tachycardia, bradycardia, cardiac arrhythmia, phlebitis
Respiratory
Bronchospasm, wheezing, hypoxemia
Dermatological
Rash, urticaria, erythema, injection site reaction
Nonspecific
Prolonged drug effect
Neurologic
Musculoskeletal
Postmarketing Experience
- Based on initial clinical practice experience in patients who received MIVACRON, spontaneously reported adverse events are uncommon. Some of these events occurred at recommended doses and required treatment.
- Anaphylaxis/Anaphylactoid Reactions: From post-marketing surveillance, MIVACRON has been associated with reports of anaphylactic/anaphylactoid reactions which in some cases have been life-threatening and fatal. Because these reactions were reported voluntarily from a population of uncertain size, it is not possible to reliably estimate their frequency. In some of these reports, sensitivity to MIVACRON was confirmed using skin test procedures.
- Other adverse reaction data from clinical practice are insufficient to establish a causal relationship or to support an estimate of their incidence. These adverse events include:
Musculoskeletal
Diminished drug effect, prolonged drug effect
Cardiovascular
Hypotension (rarely severe), flushing
Respiratory
Integumentary
Drug Interactions
- Although MIVACRON (a mixture of three stereoisomers) has been administered safely following succinylcholine-facilitated tracheal intubation, the interaction between MIVACRON and succinylcholine has not been systematically studied. Prior administration of succinylcholine can potentiate the neuromuscular blocking effects of nondepolarizing agents. Evidence of spontaneous recovery from succinylcholine should be observed before the administration of MIVACRON.
- The use of MIVACRON before succinylcholine to attenuate some of the side effects of succinylcholine has not been studied.
- There are no clinical data on the use of MIVACRON with other nondepolarizing neuromuscular blocking agents.
- Isoflurane and enflurane (administered with nitrous oxide/oxygen to achieve 1.25 MAC) decrease the ED50 of MIVACRON by as much as 25%. These agents may also prolong the clinically effective duration of action and decrease the average infusion requirement of MIVACRON by as much as 35% to 40%. A greater potentiation of the neuromuscular blocking effects of MIVACRON may be expected with higher concentrations of enflurane or isoflurane. Halothane has little or no effect on the ED50, but may prolong the duration of action and decrease the average infusion requirement by as much as 20%.
- Other drugs which may enhance the neuromuscular blocking action of nondepolarizing agents such as MIVACRON include certain antibiotics (e.g., aminoglycosides, tetracyclines, bacitracin, polymyxins, lincomycin, clindamycin, colistin, and sodium colistimethate), magnesium salts, lithium, local anesthetics, procainamide, and quinidine. The neuromuscular blocking effect of MIVACRON may be enhanced by drugs that reduce plasma cholinesterase activity (e.g., chronically administered oral contraceptives, glucocorticoids, or certain monoamine oxidase inhibitors) or by drugs that irreversibly inhibit plasma cholinesterase.
- Resistance to the neuromuscular blocking action of nondepolarizing neuromuscular blocking agents has been demonstrated in patients chronically administered phenytoin or carbamazepine. While the effects of chronic phenytoin or carbamazepine therapy on the action of MIVACRON are unknown, slightly shorter durations of neuromuscular block may be anticipated and infusion rate requirements may be higher.
Use in Specific Populations
Pregnancy
- Pregnancy Category C
- Teratology testing in nonventilated pregnant rats and mice treated subcutaneously with maximum subparalyzing doses of MIVACRON revealed no maternal or fetal toxicity or teratogenic effects. There are no adequate and well-controlled studies of MIVACRON in pregnant women. Because animal studies are not always predictive of human response, and the doses used were subparalyzing, MIVACRON should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
- Australian Drug Evaluation Committee (ADEC) Pregnancy Category
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Mivacurium chloride in women who are pregnant.
Labor and Delivery
- The use of MIVACRON during labor, vaginal delivery, or cesarean section has not been studied in humans and it is not known whether MIVACRON administered to the mother has effects on the fetus. Doses of 0.08 and 0.2 mg/kg MIVACRON given to female beagles undergoing cesarean section resulted in negligible levels of the stereoisomers in MIVACRON in umbilical vessel blood of neonates and no deleterious effects on the puppies.
Nursing Mothers
- It is not known whether any of the stereoisomers of mivacurium are excreted in human milk. Because many drugs are excreted in human milk, caution should be exercised following administration of MIVACRON to a nursing woman.
Pediatric Use
- MIVACRON has not been studied in pediatric patients below the age of 2 years.
Geriatic Use
- MIVACRON was safely administered during clinical trials to 64 geriatric (greater than or equal to 65 years) patients, including 31 patients with significant cardiovascular disease. In general, the clearances of MIVACRON are most likely lower, the duration may be longer, the rate of recovery may be slower, therefore, MIVACRON requirements may be lower in geriatric patients.
Gender
There is no FDA guidance on the use of Mivacurium chloride with respect to specific gender populations.
Race
There is no FDA guidance on the use of Mivacurium chloride with respect to specific racial populations.
Renal Impairment
There is no FDA guidance on the use of Mivacurium chloride in patients with renal impairment.
Hepatic Impairment
There is no FDA guidance on the use of Mivacurium chloride in patients with hepatic impairment.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Mivacurium chloride in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Mivacurium chloride in patients who are immunocompromised.
Administration and Monitoring
Administration
- Intravenous
Monitoring
There is limited information regarding Monitoring of Mivacurium chloride in the drug label.
IV Compatibility
- Y-site Administration
- MIVACRON Injection may not be compatible with alkaline solutions having a pH greater than 8.5 (e.g., barbiturate solutions).
- Studies have shown that MIVACRON Injection is compatible with:
- 5% Dextrose Injection, USP
- 0.9% Sodium Chloride Injection, USP
- 5% Dextrose and 0.9% Sodium Chloride Injection, USP
- Lactated Ringer's Injection, USP
- 5% Dextrose in Lactated Ringer's Injection
- Sufenta® (sufentanil citrate) Injection, diluted as directed
- Alfenta® (alfentanil hydrochloride) Injection, diluted as directed
- Sublimaze® (fentanyl citrate) Injection, diluted as directed
- Versed® (midazolam hydrochloride) Injection, diluted as directed
- Inapsine® (droperidol) Injection, diluted as directed
- Compatibility studies with other parenteral products have not been conducted.
- Dilution Stability
- MIVACRON Injection diluted to 0.5 mg mivacurium per mL in 5% Dextrose Injection, USP, 5% Dextrose and 0.9% Sodium Chloride Injection, USP, 0.9% Sodium Chloride Injection, USP, Lactated Ringer's Injection, USP, or 5% Dextrose in Lactated Ringer's Injection is physically and chemically stable when stored in PVC (polyvinylchloride) bags at 5° to 25°C (41° to 77°F) for up to 24 hours. Aseptic techniques should be used to prepare the diluted product. Admixtures of MIVACRON should be prepared for single patient use only and used within 24 hours of preparation. The unused portion of diluted MIVACRON should be discarded after each case.
- NOTE: Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration whenever solution and container permit. Solutions which are not clear and colorless should not be used.
Overdosage
Acute Overdose
- Overdosage with neuromuscular blocking agents may result in neuromuscular block beyond the time needed for surgery and anesthesia. The primary treatment is maintenance of a patent airway and controlled ventilation until recovery of normal neuromuscular function is assured. Once evidence of recovery from neuromuscular block is observed, further recovery may be facilitated by administration of an anticholinesterase agent (e.g., neostigmine, edrophonium) in conjunction with an appropriate anticholinergic agent. Overdosage may increase the risk of hemodynamic side effects, especially decreases in blood pressure. If needed, cardiovascular support may be provided by proper positioning of the patient, fluid administration, and/or vasopressor agent administration.
- Administration of 0.03 to 0.064 mg/kg neostigmine or 0.5 mg/kg edrophonium at approximately 10% recovery from neuromuscular block (range: 1 to 15) produced 95% recovery of the muscle twitch response and a T4/T1 ratio greater than or equal to 75% in about 10 minutes. The times from 25% recovery of the muscle twitch response to T4/T1 ratio greater than or equal to 75% following these doses of antagonists averaged about 7 to 9 minutes. In comparison, average times for spontaneous recovery from 25% to T4/T1 greater than or equal to 75% were 12 to 13 minutes.
- Patients administered antagonists should be evaluated for adequate clinical evidence of antagonism, e.g., 5-second head lift and grip strength. Ventilation must be supported until no longer required.
- Antagonism may be delayed in the presence of debilitation, carcinomatosis, and the concomitant use of certain broad spectrum antibiotics, or anesthetic agents and other drugs which enhance neuromuscular block or separately cause respiratory depression. Under such circumstances the management is the same as that of prolonged neuromuscular block.
Chronic Overdose
There is limited information regarding Chronic Overdose of Mivacurium chloride in the drug label.
Pharmacology
Mechanism of Action
- MIVACRON (a mixture of three stereoisomers) binds competitively to cholinergic receptors on the motor end-plate to antagonize the action of acetylcholine, resulting in a block of neuromuscular transmission. This action is antagonized by acetylcholinesterase inhibitors, such as neostigmine.
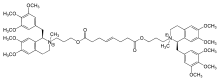
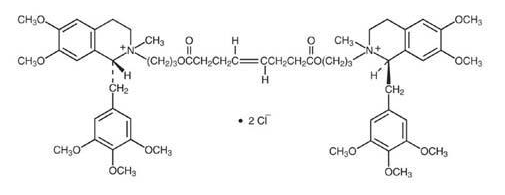
Structure
- MIVACRON (mivacurium chloride) is a short-acting, nondepolarizing skeletal muscle relaxant for intravenous (IV) administration. Mivacurium chloride is [R-[R*,R*-(E)]]-2,2'-[(1,8-dioxo-4-octene-1,8-diyl)bis(oxy-3,1-propanediyl)]bis[1,2,3,4-tetrahydro-6,7-dimethoxy-2-methyl-1-[(3,4,5-trimethoxyphenyl)methyl]isoquinolinium] dichloride. The molecular formula is C58H80Cl2N2O14 and the molecular weight is 1100.18. The structural formula is:
- The partition coefficient of the compound is 0.015 in a 1-octanol/distilled water system at 25°C.
- Mivacurium chloride is a mixture of three stereoisomers: (1R,1'R , 2S, 2'S ), the trans-trans diester; (1R,1'R , 2R, 2'S ), the cis-trans diester; and (1R,1'R , 2R, 2'R ), the cis-cis diester. The trans-trans and cis-trans stereoisomers comprise 92% to 96% of mivacurium chloride and their neuromuscular blocking potencies are not significantly different from each other or from mivacurium chloride. The cis-cis diester has been estimated from studies in cats to have one-tenth the neuromuscular blocking potency of the other two stereoisomers.
- MIVACRON Injection is a sterile, non-pyrogenic solution (pH 3.5 to 5) containing mivacurium chloride equivalent to 2 mg/mL mivacurium in Water for Injection. Hydrochloric acid may have been added to adjust pH.
Pharmacodynamics
- The time to maximum neuromuscular block is similar for recommended doses of MIVACRON and intermediate-acting agents (e.g., atracurium), but longer than for the ultra-short-acting agent, succinylcholine. The clinically effective duration of action of MIVACRON (a mixture of three stereoisomers) is one-third to one-half that of intermediate-acting agents and 2 to 2.5 times that of succinylcholine.
- The average ED95 (dose required to produce 95% suppression of the adductor pollicis muscle twitch response to ulnar nerve stimulation) of MIVACRON is 0.07 mg/kg (range: 0.05 mg/kg to 0.09 mg/kg) in adults receiving opioid/nitrous oxide/oxygen anesthesia. The pharmacodynamics of doses of MIVACRON greater than or equal to ED95 administered over 5 to 15 seconds during opioid/nitrous oxide/oxygen anesthesia are summarized in Table 1. The mean time for spontaneous recovery of the twitch response from 25% to 75% of control amplitude is about 6 minutes (range: 3 to 9 minutes, n = 32) following an initial dose of 0.15 mg/kg MIVACRON and 7 to 8 minutes (range: 4 to 24 minutes, n = 85) following initial doses of 0.2 or 0.25 mg/kg MIVACRON.
- Volatile anesthetics may decrease the dosing requirement for MIVACRON and prolong the duration of action; the magnitude of these effects may be increased as the concentration of the volatile agent is increased. Isoflurane and enflurane (administered with nitrous oxide/oxygen to achieve 1.25 MAC [Minimum Alveolar Concentration]) may decrease the effective dose of MIVACRON by as much as 25%, and may prolong the clinically effective duration of action and decrease the average infusion requirement by as much as 35% to 40%. At equivalent MAC values, halothane has little or no effect on the ED50 of MIVACRON, but may prolong the duration of action and decrease the average infusion requirement by as much as 20%.
- Administration of MIVACRON over 30 to 60 seconds does not alter the time to maximum neuromuscular block or the duration of action. The duration of action of MIVACRON may be prolonged in patients with reduced plasma cholinesterase (pseudocholinesterase) activity.
- Interpatient variability in duration of action occurs with MIVACRON as with other neuromuscular blocking agents. However, analysis of data from 224 patients in clinical studies receiving various doses of MIVACRON during opioid/nitrous oxide/oxygen anesthesia with a variety of premedicants and varying lengths of surgery indicated that approximately 90% of the patients had clinically effective durations of block within 8 minutes of the median duration predicted from the dose-response data shown in Table 1. Variations in plasma cholinesterase activity, including values within the normal range and values as low as 20% below the lower limit of the normal range, were not associated with clinically significant effects on duration. The variability in duration, however, was greater in patients with plasma cholinesterase activity at or slightly below the lower limit of the normal range.
- When administered during the induction of adequate anesthesia using thiopental or propofol, nitrous oxide/oxygen, and co-induction agents such as fentanyl and/or midazolam, doses of 0.15 mg/kg (2 x ED95) MIVACRON administered over 5 to 15 seconds or 0.2 mg/kg MIVACRON administered over 30 seconds produced generally good-to-excellent tracheal intubation conditions in 2.5 to 3 and 2 to 2.5 minutes, respectively. A dose of 0.25 mg/kg MIVACRON administered as a divided dose (0.15 mg/kg followed 30 seconds later by 0.1 mg/kg) produced generally good-to-excellent intubation conditions in 1.5 to 2 minutes after initiating the dosing regimen.
- Repeated administration of maintenance doses or continuous infusion of MIVACRON for up to 2.5 hours is not associated with development of tachyphylaxis or cumulative neuromuscular blocking effects in ASA Physical Status I-II patients. Based on pharmacokinetic studies in 82 adults receiving infusions of MIVACRON for longer than 2.5 hours, spontaneous recovery of neuromuscular function after infusion is independent of the duration of infusion and comparable to recovery reported for single doses (Table 1).
- MIVACRON was administered as an infusion for as long as 4 to 6 hours in 20 adult patients and 19 geriatric patients. In most patients, after a brief period of adjustment, the rate of MIVACRON required to maintain 89% to 99% T1 suppression remained relatively constant over time. There was a subset of patients in each group whose infusion rates did not stabilize quickly and decreased (by greater than or equal to 30%) over the period of infusion. The rate of spontaneous recovery in these patients was comparable with that of patients having stable infusion rates and not dependent on the duration of infusion. These patients, however, tended to have higher infusion requirements (i.e., greater than 8 mcg/kg/min) during the first 30 minutes of infusion than patients with stable infusion rates, although their final infusion rates were similar to those with stable infusion rates. There were no clinically important differences in infusion rate requirements between geriatric and young patients.
- The neuromuscular block produced by MIVACRON is readily antagonized by anticholinesterase agents. As seen with other nondepolarizing neuromuscular blocking agents, the more profound the neuromuscular block at the time of reversal, the longer the time and the greater the dose of anticholinesterase agent required for recovery of neuromuscular function.
- In children (2 to 12 years), MIVACRON has a higher ED95 (0.1 mg/kg), faster onset, and shorter duration of action than in adults. The mean time for spontaneous recovery of the twitch response from 25% to 75% of control amplitude is about 5 minutes (n = 4) following an initial dose of 0.2 mg/kg MIVACRON. Recovery following reversal is faster in children than in adults (Table 1).
- Hemodynamics
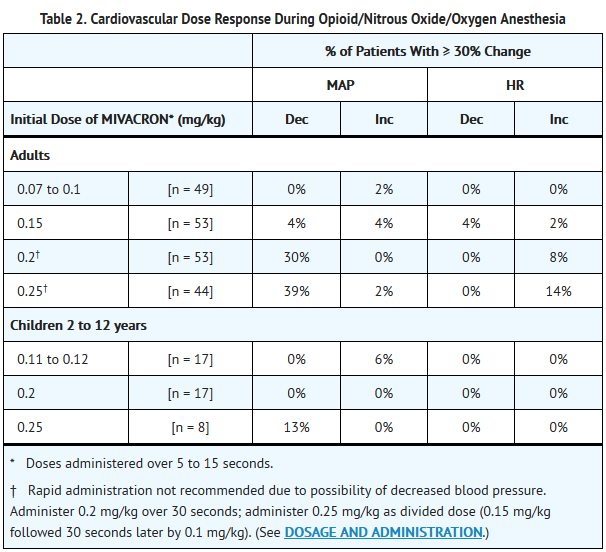
- Administration of MIVACRON in doses up to and including 0.15 mg/kg (2 x ED95) over 5 to 15 seconds to ASA Physical Status I-II patients during opioid/nitrous oxide/oxygen anesthesia is associated with minimal changes in mean arterial blood pressure (MAP) or heart rate (HR) (Table 2).
- Higher doses of greater than or equal to 0.2 mg/kg (greater than or equal to 3 x ED95) may be associated with transient decreases in MAP and increases in HR in some patients. These decreases in MAP are usually maximal within 1 to 3 minutes following the dose, typically resolve without treatment in an additional 1 to 3 minutes, and are usually associated with increases in plasma histamine concentration. Decreases in MAP can be minimized by administering MIVACRON over 30 to 60 seconds.
- Analysis of 426 patients in clinical studies receiving initial doses of MIVACRON up to and including 0.3 mg/kg during opioid/nitrous oxide/oxygen anesthesia showed that high initial doses and a rapid rate of injection contributed to a greater probability of experiencing a decrease of greater than or equal to 30% in MAP after administration of MIVACRON. Obese patients also had a greater probability of experiencing a decrease of greater than or equal to 30% in MAP when dosed on the basis of actual body weight, thereby receiving a larger dose than if dosed on the basis of ideal body weight.
- Children experience minimal changes in MAP or HR after administration of doses of MIVACRON up to and including 0.2 mg/kg over 5 to 15 seconds, but higher doses (greater than or equal to 0.25 mg/kg) may be associated with transient decreases in MAP (Table 2).
- Following a dose of 0.15 mg/kg MIVACRON administered over 60 seconds, adult patients with significant cardiovascular disease undergoing coronary artery bypass grafting or valve replacement procedures showed no clinically important changes in MAP or HR. Transient decreases in MAP were observed in some patients after doses of 0.2 to 0.25 mg/kg MIVACRON administered over 60 seconds. The number of patients in whom these decreases in MAP required treatment was small.
Pharmacokinetics
- MIVACRON is a mixture of isomers which do not interconvert in vivo. The cis-trans and trans-trans isomers (92% to 96% of the mixture) are equipotent. The steady-state concentrations of the cis-trans and trans-trans isomers doubled after the infusion rate was increased from 5 to 10 mcg/kg/min, indicating that their pharmacokinetics is dose-proportional.
- The cis-cis isomer (6% of the mixture) has approximately one-tenth the neuromuscular blocking potency of the trans-trans and cis-trans isomers in cats. Neuromuscular blocking effects due to the cis-cis isomer cannot be ruled out in humans; however, modeling of clinical pharmacokinetic-pharmacodynamic data suggests that the cis-cis isomer produces minimal (less than 5%) neuromuscular block during a 2-hour infusion. In studies of ASA Physical Status I-II patients receiving infusions of MIVACRON lasting as long as 4 to 6 hours, the 5% to 25% and the 25% to 75% recovery indices were independent of the duration of infusion, suggesting that the cis-cis isomer does not affect the rate of post-infusion recovery.
- Distribution
- The volume of distribution of cis-trans and trans-trans isomers in healthy surgical patients is relatively small, reflecting limited tissue distribution (Table 3). The volume of distribution of cis-cis isomers is also small and averaged 335 mL/kg (range 192 to 523) in the 18 healthy surgical patients whose data are displayed in Table 3. The protein binding of mivacurium has not been determined due to its rapid hydrolysis by plasma cholinesterase.
- Metabolism
- Enzymatic hydrolysis by plasma cholinesterase is the primary mechanism for inactivation of mivacurium and yields a quaternary alcohol and a quaternary monoester metabolite. Tests in which these two metabolites were administered to cats and dogs suggest that each metabolite is unlikely to produce clinically significant neuromuscular, autonomic, or cardiovascular effects following administration of MIVACRON.
- The mean ± S.D. in vitro t½ values of the trans-trans and the cis-trans isomers were 1.3 ± 0.3 and 0.8 ± 0.2 minutes, respectively, in human plasma from healthy male (n = 5) and female (n = 5) volunteers. The mean in vivo t½ values for the more potent trans-trans and cis-trans isomers in healthy surgical patients (Table 3) were similar to those found in vitro , suggesting that hydrolysis by plasma cholinesterase is the predominant elimination pathway for these isomers. The mean ± S.D. in vitro t½ of the less potent cis-cis isomer was 276 ± 130 minutes, while the mean ± S.D. in vivo t½ for the cis-cis isomer in healthy surgical patients was 53 ± 20 minutes. These data suggest that in vivo , pathways other than hydrolysis by plasma cholinesterase contribute to the elimination of the cis-cis isomer.
- Elimination
- The clearance (CL) values of the two more potent isomers, cis-trans and trans-trans, are very high and are dependent on plasma cholinesterase activity (Table 3). The combination of high CL and low distribution volume results in t½ values of approximately 2 minutes for the two more potent isomers. The short t½ and high CL of the more potent isomers are consistent with the short duration of action of MIVACRON.
- The CL of the less potent cis-cis isomer is not dependent on plasma cholinesterase. The mean ± S.D. CL was 4.6 ± 1.1 mL/min/kg and t½ was 53 ± 20 minutes in the 18 healthy surgical patients whose data are displayed in Table 3.
- Renal and biliary excretion of unchanged mivacurium are minor elimination pathways; urine and bile are important elimination pathways for the two metabolites.
- Special Populations
- Geriatric Patients (greater than or equal to 60 years)
- Two pharmacokinetic/pharmacodynamic studies of MIVACRON have been conducted in geriatric patients. The first study compared the pharmacokinetics and pharmacodynamics of mivacurium in 19 geriatric patients with those in 20 adult patients receiving infusions for as long as 4 to 6 hours. The average infusion rate required to produce 89% to 99% T1 suppression was slightly (~ 14%) lower in geriatric patients. This difference is not regarded as clinically important, but is most likely secondary to differences in pharmacokinetics (i.e., a lower CL of the cis-trans and trans-trans isomers in geriatric patients) (Table 4). The rate of post-infusion spontaneous recovery was not dependent on duration of infusion and appeared to be comparable in these geriatric patients and adult patients. Two pharmacodynamic studies in which patients received infusions for a shorter duration (2 to 3 hours) have shown that the infusion rate requirements were lower (by 38%) in geriatric patients (64 to 86 years of age) than in younger patients (18 to 41 years of age).
- The second pharmacokinetic/pharmacodynamic study showed no clinically important differences in the pharmacokinetics of the individual isomers nor the ED95 determined for 36 young adult patients (18 to 40 years) and 35 geriatric patients (greater than or equal to 65 years) during opioid/nitrous oxide/oxygen anesthesia. Following infusions for up to 3.5 hours in these patients, the rate of spontaneous recovery was slightly (~ 2 to 4 minutes, on average) slower in the geriatric patients than in young adult patients.
- In a third study of the pharmacodynamics of 0.1 mg/kg MIVACRON administered to eight geriatric patients (68 to 77 years) and nine adult patients (18 to 49 years) during N2O/O2/isoflurane anesthesia, the time to onset was approximately 1.5 minutes slower in geriatric patients than in adult patients. In addition, the clinical duration was slightly (~ 3 minutes, on average) longer in geriatric patients than in adult patients; these differences are not considered clinically important.
- Although these studies showed conflicting findings, in general, the clearances of the more potent isomers are most likely lower in geriatric patients. This difference does not lead to clinically important differences in the ED95 of MIVACRON or the infusion rate of MIVACRON required to produce 95% T1 suppression in geriatric patients. However, the time to onset may be slower, the duration may be slightly longer, the rate of recovery may be slightly slower, therefore MIVACRON requirements may be lower in geriatric patients.
- Patients with Renal Disease
- An early clinical trial showed that the clinically effective duration of action of 0.15 mg/kg MIVACRON was about 1.5 times longer in kidney transplant patients than in healthy patients, presumably due to reduced clearance of one or more isomers. A second study was conducted in seven patients with mild to moderate renal impairment, eight patients with severe renal dysfunction (not undergoing transplantation), and 11 patients with normal renal function. This study showed that the pharmacokinetics of the more potent (cis-trans and trans-trans) isomers were not statistically significantly affected by renal impairment or failure (Table 5). However, the CL of the cis-cis isomer was lower and the t½ values of the cis-cis isomer and metabolites were longer in patients with renal impairment or failure than in patients with normal renal function. The second study also showed that there were no differences in the average infusion rate required to produce 89% to 99% T1 suppression, nor were there any differences in the post-infusion recovery profile among these populations (Table 5). A third study in a similar population showed that patients with renal dysfunction had a longer duration and a slower rate of recovery than patients with normal renal function. This study did, however, confirm that there were no differences in the average infusion rate required to produce 89% to 99% T1 suppression in these patient populations. Therefore, although there were minor differences in the pharmacokinetics of the cis-cis isomer and metabolites, there were no clinically significant differences in the infusion rate requirements of MIVACRON in patients with mild, moderate, or severe renal dysfunction receiving infusions of MIVACRON for an average of 1 to 2 hours; however, the duration may be longer and the rate of recovery may be slower following administration of MIVACRON in some patients with renal dysfunction.
- Patients with Hepatic Disease
- The clinically effective duration of action of 0.15 mg/kg MIVACRON was three times longer in eight patients with end-stage liver disease (undergoing liver transplantation) than in eight healthy patients and is likely related to the markedly decreased plasma cholinesterase activity (30% of healthy patient values) which could decrease the clearance of the trans-trans and cis-trans isomers.
- A separate study compared the pharmacokinetics and pharmacodynamics of mivacurium in patients with mild or moderate cirrhosis to healthy adults with normal hepatic function (Table 6). Although the number of patients in each group is small, the CL values of the more potent isomers, trans-trans and cis-trans, are lower in patients with mild to moderate cirrhosis as expected based on the marked decreases in plasma cholinesterase activity in this population.
- Individualization of Dosages
- Doses of MIVACRON should be individualized and a peripheral nerve stimulator should be used to measure neuromuscular function during administration of MIVACRON in order to monitor drug effect, determine the need for additional doses, and confirm recovery from neuromuscular block.
- Based on the known actions of MIVACRON (a mixture of three stereoisomers) and other neuromuscular blocking agents, the following factors should be considered when administering MIVACRON:
- Renal or Hepatic Impairment
- A dose of 0.15 mg/kg MIVACRON is recommended for facilitation of tracheal intubation in patients with renal or hepatic impairment. However, the clinically effective duration of block produced by this dose may be about 1.5 times longer in patients with end-stage kidney disease and about 3 times longer in patients with end-stage liver disease than in patients with normal renal and hepatic function. Infusion rates should be decreased by as much as 50% in patients with hepatic disease depending on the degree of hepatic impairment. No infusion rate adjustments are necessary in patients with renal impairment.
- Reduced Plasma Cholinesterase Activity
- The possibility of prolonged neuromuscular block following administration of MIVACRON must be considered in patients with reduced plasma cholinesterase (pseudocholinesterase) activity. MIVACRON should be used with great caution, if at all, in patients known or suspected of being homozygous for the atypical plasma cholinesterase gene. Doses of 0.03 mg/kg produced complete neuromuscular block for 26 to 128 minutes in three such patients; thus initial doses greater than 0.03 mg/kg are not recommended in homozygous patients. Infusions of MIVACRON are not recommended in homozygous patients.
- MIVACRON has been used safely in patients heterozygous for the atypical plasma cholinesterase gene and in genotypically normal patients with reduced plasma cholinesterase activity. After an initial dose of 0.15 mg/kg MIVACRON, the clinically effective duration of block in heterozygous patients may be approximately 10 minutes longer than in patients with normal genotype and normal plasma cholinesterase activity. Lower infusion rates of MIVACRON are recommended in these patients.
- Drugs or Conditions Causing Potentiation of or Resistance to Neuromuscular Block
- As with other neuromuscular blocking agents, MIVACRON may have profound neuromuscular blocking effects in cachectic or debilitated patients, patients with neuromuscular diseases, and patients with carcinomatosis. In these or other patients in whom potentiation of neuromuscular block or difficulty with reversal may be anticipated, the initial dose should be decreased. A test dose of not more than 0.015 to 0.02 mg/kg, which represents the lower end of the dose-response curve for MIVACRON, is recommended in such patients.
- The neuromuscular blocking action of MIVACRON is potentiated by isoflurane or enflurane anesthesia. Recommended initial doses of MIVACRON may be used for intubation prior to the administration of these agents. If MIVACRON is first administered after establishment of stable-state isoflurane or enflurane anesthesia (administered with nitrous oxide/oxygen to achieve 1.25 MAC), the initial dose of MIVACRON should be reduced by as much as 25%, and the infusion rate reduced by as much as 35% to 40%. A greater potentiation of the neuromuscular blocking action of MIVACRON may be expected with higher concentrations of enflurane or isoflurane. The use of halothane requires no adjustment of the initial dose of MIVACRON, but may prolong the duration of action and decrease the average infusion rate by as much as 20%.
- When MIVACRON is administered to patients receiving certain antibiotics, magnesium salts, lithium, local anesthetics, procainamide and quinidine, longer durations of neuromuscular block may be expected and infusion requirements may be lower.
- When MIVACRON is administered to patients chronically receiving phenytoin or carbamazepine, slightly shorter durations of neuromuscular block may be anticipated and infusion rate requirements may be higher.
- Severe acid-base and/or electrolyte abnormalities may potentiate or cause resistance to the neuromuscular blocking action of MIVACRON. No data are available in such patients and no dosing recommendations can be made.
- Burns
- While patients with burns are known to develop resistance to nondepolarizing neuromuscular blocking agents, they may also have reduced plasma cholinesterase activity. Consequently, in these patients, a test dose of not more than 0.015 to 0.02 mg/kg MIVACRON is recommended, followed by additional appropriate dosing guided by the use of a neuromuscular block monitor.
- Cardiovascular Disease
- In patients with clinically significant cardiovascular disease, the initial dose of MIVACRON should be 0.15 mg/kg or less, administered over 60 seconds.
- Obesity
- Obese patients (patients weighing greater than or equal to 30% more than their ideal body weight) dosed on the basis of actual body weight, thereby receiving a larger dose than if dosed on the basis of ideal body weight, had a greater probability of experiencing a decrease of greater than or equal to 30% in MAP. Therefore, in obese patients, the initial dose should be determined using the patient's ideal body weight (IBW), according to the following formulae:
- Men: IBW in kg = (106 + [6 x inches in height above 5 feet])/2.2
- Women: IBW in kg = (100 + [5 x inches in height above 5 feet])/2.2
- Allergy and Sensitivity
Nonclinical Toxicology
- Carcinogenesis and fertility studies have not been performed. MIVACRON was evaluated in a battery of four short-term mutagenicity tests. It was non-mutagenic in the Ames Salmonella assay, the mouse lymphoma assay, the human lymphocyte assay, and the in vivo rat bone marrow cytogenetic assay.
Clinical Studies
There is limited information regarding Clinical Studies of Mivacurium chloride in the drug label.
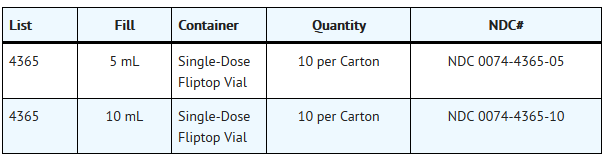
How Supplied
- MIVACRON Injection, 2 mg mivacurium in each mL.
- STORAGE
- Store MIVACRON Injection at 25°C (77°F). Excursions permitted between 15° - 30°C (59° - 86°F). DO NOT FREEZE.
Storage
There is limited information regarding Mivacurium chloride Storage in the drug label.
Images
Drug Images
{{#ask: Page Name::Mivacurium chloride |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
{{#ask: Label Page::Mivacurium chloride |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
There is limited information regarding Patient Counseling Information of Mivacurium chloride in the drug label.
Precautions with Alcohol
- Alcohol-Mivacurium chloride interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
- MIVACRON®[1]
Look-Alike Drug Names
There is limited information regarding Mivacurium chloride Look-Alike Drug Names in the drug label.
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
{{#subobject:
|Page Name=Mivacurium chloride |Pill Name=No image.jpg |Drug Name= |Pill Ingred=|+sep=; |Pill Imprint= |Pill Dosage= |Pill Color=|+sep=; |Pill Shape= |Pill Size (mm)= |Pill Scoring= |Pill Image= |Drug Author= |NDC=
}}
{{#subobject:
|Label Page=Mivacurium chloride |Label Name=Mivacurium chloride10.png
}}
{{#subobject:
|Label Page=Mivacurium chloride |Label Name=Mivacurium chloride11.png
}}