Atracurium
{{DrugProjectFormSinglePage |authorTag=Chetan Lokhande, M.B.B.S [1] |genericName=Atracurium |aOrAn=a |drugClass=skeletal muscle relaxant and neuromuscular blocking drugs |indication=induction of neuromuscular blockade, adjunct to general anesthesia, to facilitate endotracheal intubation, and to provide skeletal muscle relaxation during surgery or mechanical ventilation |adverseReactions=dermatologic: flushing (1% to 29.2% ) |blackBoxWarningTitle=TITLE |blackBoxWarningBody=Condition Name: (Content) |fdaLIADAdult=* Dosage must be individualized
- Induction of neuromuscular blockade, adjunct to general anesthesia, to facilitate endotracheal intubation, and to provide skeletal muscle relaxation during surgery or mechanical ventilation:
- Initial
- 0.4 to 0.5 mg/kg IV bolus
- Induction of neuromuscular blockade, adjunct to general anesthesia, to facilitate endotracheal intubation, and to provide skeletal muscle relaxation during surgery or mechanical ventilation
- Maintenance
- 0.08 to 0.1 mg/kg IV bolus 20 to 45 min after initial dose, then every 15 to 25 min as needed
- 5 to 9 mcg/kg/min (range 2 to 15 mcg/kg/min) continuous IV infusion after initial dose, upon early evidence of spontaneous recovery; in ICU, 11 to 13 mcg/kg/min (range 4.5 to 29.5 mcg/kg/min) continuous IV infusion
|offLabelAdultGuideSupport=There is limited information regarding Off-Label Guideline-Supported Use of Atracurium in adult patients. |offLabelAdultNoGuideSupport=There is limited information regarding Off-Label Non–Guideline-Supported Use of Atracurium in adult patients. |fdaLIADPed=* Dosage must be individualized
Infants (age 1 month to 2 yr)
- Induction of neuromuscular blockade, Adjunct to general anesthesia, to facilitate endotracheal intubation, and to provide skeletal muscle relaxation during surgery or mechanical ventilation, under halothane anesthesia,
- Initial, 0.3 to 0.4 mg/kg IV
Age 2 yr and older
- Induction of neuromuscular blockade, Adjunct to general anesthesia, to facilitate endotracheal intubation, and to provide skeletal muscle relaxation during surgery or mechanical ventilation
- Initial, 0.4 to 0.5 mg/kg IV bolus
Age 1 month and older
- Induction of neuromuscular blockade, Adjunct to general anesthesia, to facilitate endotracheal intubation, and to provide skeletal muscle relaxation during surgery or mechanical ventilation
- Maintenance, 0.08 to 0.1 mg/kg IV bolus 20 to 45 min after initial dose, then every 15 to 25 min as needed; children may require maintenance doses more frequently than adults
Age 1 month and older
- Induction of neuromuscular blockade, Adjunct to general anesthesia, to facilitate endotracheal intubation, and to provide skeletal muscle relaxation during surgery or mechanical ventilation
- Maintenance, 5 to 9 mcg/kg/min (range 2 to 15 mcg/kg/min) continuous IV infusion after initial dose, upon early evidence of spontaneous recovery
|offLabelPedGuideSupport=There is limited information regarding Off-Label Guideline-Supported Use of Atracurium in pediatric patients. |offLabelPedNoGuideSupport=There is limited information regarding Off-Label Non–Guideline-Supported Use of Atracurium in pediatric patients. |contraindications=* Atracurium besylate is contraindicated in patients known to have a hypersensitivity to it. Use of atracurium besylate from multiple dose vials containing benzyl alcohol as a preservative is contraindicated in patients with a known hypersensitivity to benzyl alcohol. |warnings=* Atracurium should be used only by those skilled in airway management and respiratory support. equipment and personnel must be immediately available for endotracheal intubation and support of ventilation, including administration of positive pressure oxygen. adequacy of respiration must be assured through assisted or controlled ventilation. anticholinesterase reversal agents should be immediately available.
- Do not give atracurium besylate by intramuscular administration.
- Atracurium has no known effect on consciousness, pain threshold, or cerebration. It should be used only with adequate anesthesia.
- Atracurium besylate injection, which has an acid pH, should not be mixed with alkaline solutions (e.g., barbiturate solutions) in the same syringe or administered simultaneously during intravenous infusion through the same needle. Depending on the resultant pH of such mixtures, atracurium may be inactivated and a free acid may be precipitated.
- Atracurium besylate injection 10 mL multiple dose vials contain benzyl alcohol. In neonates, benzyl alcohol has been associated with an increased incidence of neurological and other complications which are sometimes fatal. Atracurium besylate 5 mL single use vials do not contain benzyl alcohol (see Precautions: Pediatric Use).
Anaphylaxis
- Severe anaphylactic reactions to neuromuscular blocking agents, including atracurium besylate, have been reported. These reactions have in some cases been life-threatening and fatal. Due to the potential severity of these reactions, the necessary precautions, such as the immediate availability of appropriate emergency treatment, should be taken. Precautions should also be taken in those individuals who have had previous anaphylactic reactions to other neuromuscular blocking agents since cross-reactivity between neuromuscular blocking agents, both depolarizing and non-depolarizing, has been reported in this class of drugs.
|clinicalTrials=* Observed in Controlled Clinical Studies: Atracurium was well tolerated and produced few adverse reactions during extensive clinical trials. Most adverse reactions were suggestive of histamine release. In studies including 875 patients, atracurium was discontinued in only one patient (who required treatment for bronchial secretions) and six other patients required treatment for adverse reactions attributable to atracurium (wheezing in one, hypotension in five). Of the five patients who required treatment for hypotension, three had a history of significant cardiovascular disease. The overall incidence rate for clinically important adverse reactions, therefore, was 7/875 or 0.8%.
- Table 1 includes all adverse reaction reported attributable to atracurium during clinical trials with 875 patients.
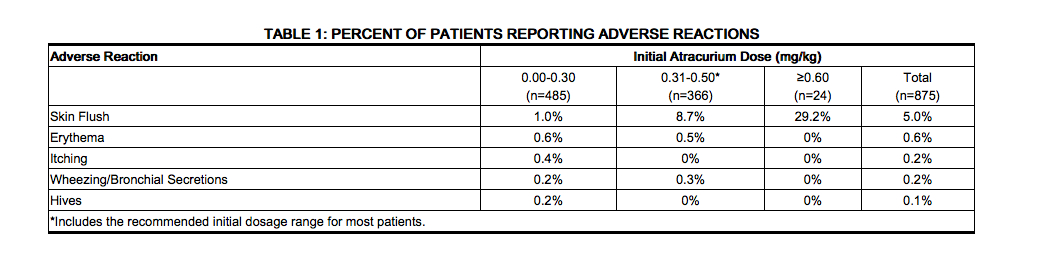
- Most adverse reactions were of little clinical significance unless they were associated with significant hemodynamic changes. Table 2 summarizes the incidences of substantial vital sign changes noted during atracurium clinical trials with 530 patients, without cardiovascular disease, in whom these parameters were assessed.
[File:ATRACURIUMadverse2.jpg|thumb|none|400px|left|This image is provided by the National Library of Medicine.]]
Observed in Clinical Practice
- Based on initial clinical practice experience in approximately 3 million patients who received atracurium in the U.S. and in the United Kingdom, spontaneously reported adverse reactions were uncommon (approximately 0.01% to 0.02%). The following adverse reactions are among the most frequently reported, but there are insufficient data to support an estimate of their incidence:
General
- Allergic reactions (anaphylactic or anaphylactoid responses) which, in rare instances, were severe (e.g., cardiac arrest)
Musculoskeletal
- Inadequate block, prolonged block
Cardiovascular
- Hypotension, vasodilatation (flushing), tachycardia, bradycardia
Respiratory
Integumentary
- There have been rare spontaneous reports of seizures in ICU patients following long-term infusion of atracurium to support mechanical ventilation. There are insufficient data to define the contribution, if any, of atracurium and/or its metabolite laudanosine. (See PRECAUTIONS: Long-Term Use in Intensive Care Unit [ICU]).
- There have been post-marketing reports of severe allergic reactions (anaphylactic and anaphylactoid reactions) associated with use of neuromuscular blocking agents, including atracurium besylate. These reactions, in some cases, have been life-threatening and fatal. Because these reactions were reported voluntarily from a population of uncertain size, it is not possible to reliably estimate their frequency (see Warnings and Precautions).
|drugInteractions=* Drugs which may enhance the neuromuscular blocking action of atracurium include: enflurane; isoflurane; halothane; certain antibiotics, especially the aminoglycosides and polymyxins; lithium; magnesium salts; procainamide; and quinidine.
- If other muscle relaxants are used during the same procedure, the possibility of a synergistic or antagonist effect should be considered.
- The prior administration of succinylcholine does not enhance the duration, but quickens the onset and may increase the depth, of neuromuscular block induced by atracurium besylate. Atracurium should not be administered until a patient has recovered from succinylcholine-induced neuromuscular block.
|FDAPregCat=C |useInPregnancyFDA=* Atracurium besylate has been shown to be potentially teratogenic in rabbits when given in doses up to approximately one-half the human dose. There are no adequate and well-controlled studies in pregnant women. Atracurium should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
- Atracurium besylate was administered subcutaneously on days 6 through 18 of gestation to nonventilated Dutch rabbits. Treatment groups were given either 0.15 mg/kg once daily or 0.10 mg/kg twice daily. Lethal respiratory distress occurred in two 0.15 mg/kg animals and in one 0.10 mg/kg animal, with transient respiratory distress or other evidence of neuromuscular block occurring in 10 of 19 and in 4 of 20 of the 0.15 mg/kg and 0.10 mg/kg animals, respectively. There was an increased incidence of certain spontaneously occurring visceral and skeletal anomalies or variations in one or both treated groups when compared to non-treated controls. The percentage of male fetuses was lower (41% vs. 51%) and the post-implantation losses were increased (15% vs. 8%) in the group given 0.15 mg/kg once daily when compared to the controls; the mean numbers of implants (6.5 vs. 4.4) and normal live fetuses (5.4 vs. 3.8) were greater in this group when compared to the control group.
|useInLaborDelivery=* It is not known whether muscle relaxants administered during vaginal delivery have immediate or delayed adverse effects on the fetus or increase the likelihood that resuscitation of the newborn will be necessary. The possibility that forceps delivery will be necessary may increase.
- Atracurium besylate (0.3 mg/kg) has been administered to 26 pregnant women during delivery by cesarean section. No harmful effects were attributable to atracurium in any of the neonates, although small amounts of atracurium were shown to cross the placental barrier. The possibility of respiratory depression in the neonate should always be considered following cesarean section during which a neuromuscular blocking agent has been administered. In patients receiving magnesium sulfate, the reversal of neuromuscular block may be unsatisfactory and the dose of atracurium besylate should be lowered as indicated.
|useInNursing=* It is not known whether this drug is excreted in human milk. Because many drugs are excreted in human milk, caution should be exercised when atracurium besylate is administered to a nursing woman. |useInPed=* Safety and effectiveness in pediatric patients below the age of 1 month have not been established. |useInGeri=* Since marketing in 1983, uncontrolled clinical experience and limited data from controlled trials have not identified differences in effectiveness, safety, or dosage requirements between healthy elderly and younger patients (see Clinical pharmacology); however, as with other neuromuscular blocking agents, the use of a peripheral nerve stimulater to monitor neuromuscular function is suggested (see Dosage and administration). |administration=* To avoid distress to the patient, atracurium should not be administered before unconsciousness has been induced. Atracurium should not be mixed in the same syringe, or administered simultaneously through the same needle, with alkaline solutions (e.g., barbiturate solutions).
- Atracurium besylate should be administered intravenously. Do not give atracurium besylate by intramuscular administration. Intramuscular administration of atracurium besylate may result in tissue irritation and there are no clinical data to support this route of administration.
- As with other neuromuscular blocking agents, the use of a peripheral nerve stimulator will permit the most advantageous use of atracurium besylate, minimizing the possibility of overdosage or underdosage, and assist in the evaluation of recovery.
Bolus Doses for Intubation and Maintenance of Neuromuscular Block
Adults
- An atracurium besylate dose of 0.4 to 0.5 mg/kg (1.7 to 2.2 times the ED95), given as an intravenous bolus injection, is the recommended initial dose for most patients. With this dose, good or excellent conditions for nonemergency intubation can be expected in 2 to 2.5 minutes in most patients, with maximum neuromuscular block achieved approximately 3 to 5 minutes after injection. Clinically required neuromuscular block generally lasts 20 to 35 minutes under balanced anesthesia. Under balanced anesthesia, recovery to 25% of control is achieved approximately 35 to 45 minutes after injection, and recovery is usually 95% complete approximately 60 minutes after injection.
- Atracurium is potentiated by isoflurane or enflurane anesthesia. The same initial atracurium besylate dose of 0.4 to 0.5 mg/kg may be used for intubation prior to administration of these inhalation agents; however, if atracurium is first administered under steady-state of isoflurane or enflurane, the initial atracurium besylate dose should be reduced by approximately one-third, i.e., to 0.25 to 0.35 mg/kg, to adjust for the potentiating effects of these anesthetic agents. With halothane, which has only a marginal (approximately 20%) potentiating effect on atracurium, smaller dosage reductions may be considered.
- Atracurium besylate doses of 0.08 to 0.10 mg/kg are recommended for maintenance of neuromuscular block during prolonged surgical procedures. * The first maintenance dose will generally be required 20 to 45 minutes after the initial atracurium besylate injection, but the need for maintenance doses should be determined by clinical criteria. Because atracurium lacks cumulative effects, maintenance doses may be administered at relatively regular intervals for each patient, ranging approximately from 15 to 25 minutes under balanced anesthesia, slightly longer under isoflurane or enflurane. Higher atracurium doses (up to 0.2 mg/kg) permit maintenance dosing at longer intervals.
Pediatric Patients
- No atracurium dosage adjustments are required for pediatric patients two years of age or older. An atracurium besylate dose of 0.3 to 0.4 mg/kg is recommended as the initial dose for infants (1 month to 2 years of age) under halothane anesthesia. Maintenance doses may be required with slightly greater frequency in infants and children than in adults.
Special Considerations
- An initial atracurium besylate dose of 0.3 to 0.4 mg/kg, given slowly or in divided doses over one minute, is recommended for adults, children, or infants with significant cardiovascular disease and for adults, children, or infants with any history (e.g., severe anaphylactoid reactions or asthma) suggesting a greater risk of histamine release.
- Dosage reductions must be considered also in patients with neuromuscular disease, severe electrolyte disorders, or carcinomatosis in which potentiation of neuromuscular block or difficulties with reversal have been demonstrated. There has been no clinical experience with atracurium in these patients, and no specific dosage adjustments can be recommended. No atracurium dosage adjustments are required for patients with renal disease.
- An initial atracurium besylate dose of 0.3 to 0.4 mg/kg is recommended for adults following the use of succinylcholine for intubation under balanced anesthesia. Further reductions may be desirable with the use of potent inhalation anesthetics. The patient should be permitted to recover from the effects of succinylcholine prior to atracurium administration. Insufficient data are available for recommendation of a specific initial atracurium dose for administration following the use of succinylcholine in children and infants.
Use by Continuous Infusion
Infusion in the Operating Room (OR)
- After administration of a recommended initial bolus dose of atracurium besylate injection (0.3 to 0.5 mg/kg), a diluted solution of atracurium besylate can be administered by continuous infusion to adults and pediatric patients aged 2 or more years for maintenance of neuromuscular block during extended surgical procedures.
- Infusion of atracurium should be individualized for each patient. The rate of administration should be adjusted according to the patient’s response as determined by peripheral nerve stimulation. Accurate dosing is best achieved using a precision infusion device.
- Infusion of atracurium should be initiated only after early evidence of spontaneous recovery from the bolus dose. An initial infusion rate of 9 to 10 mcg/kg/min may be required to rapidly counteract the spontaneous recovery of neuromuscular function. Thereafter, a rate of 5 to 9 mcg/kg/min should be adequate to maintain continuous neuromuscular block in the range of 89% to 99% in most pediatric and adult patients under balanced anesthesia. Occasional patients may require infusion rates as low as 2 mcg/kg/min or as high as 15 mcg/kg/min.
- The neuromuscular blocking effect of atracurium administered by infusion is potentiated by enflurane or isoflurane and, to a lesser extent, by halothane. Reduction in the infusion rate of atracurium should, therefore, be considered for patients receiving inhalation anesthesia. The rate of atracurium infusion should be reduced by approximately one-third in the presence of steady-state enflurane or isoflurane anesthesia; smaller reductions should be considered in the presence of halothane.
- In patients undergoing cardiopulmonary bypass with induced hypothermia, the rate of infusion of atracurium required to maintain adequate surgical relaxation during hypothermia (25° to 28°C) has been shown to be approximately half the rate required during normothermia.
- Spontaneous recovery from neuromuscular block following discontinuation of atracurium infusion may be expected to proceed at a rate comparable to that following administration of a single bolus dose.
Infusion in the Intensive Care Unit (ICU)
- The principles for infusion of atracurium in the OR are also applicable to use in the ICU.
- An infusion rate of 11 to 13 mcg/kg/min (range: 4.5 to 29.5) should provide adequate neuromuscular block in adult patients in an ICU. Limited information suggests that infusion rates required for pediatric patients in the ICU may be higher than in adult patients. There may be wide interpatient variability in dosage requirements and these requirements may increase or decrease with time (see PRECAUTIONS: Long-Term Use in Intensive Care Unit [ICU]). Following recovery from neuromuscular block, readministration of a bolus dose may be necessary to quickly reestablish neuromuscular block prior to reinstitution of the infusion.
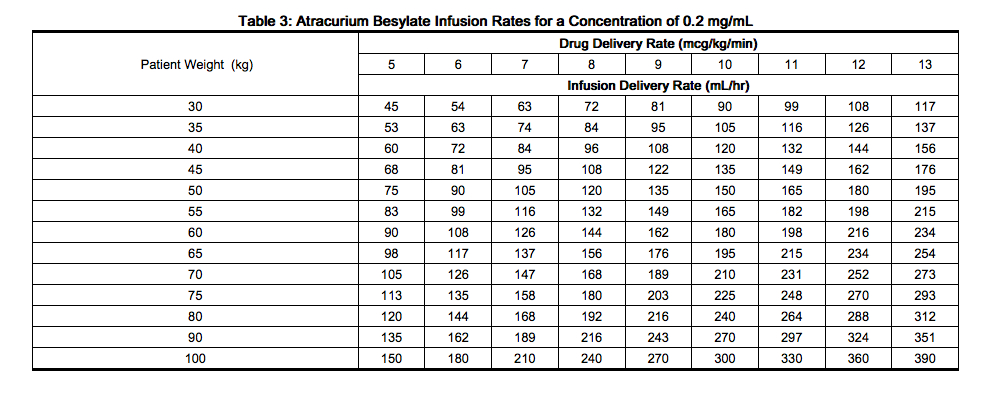
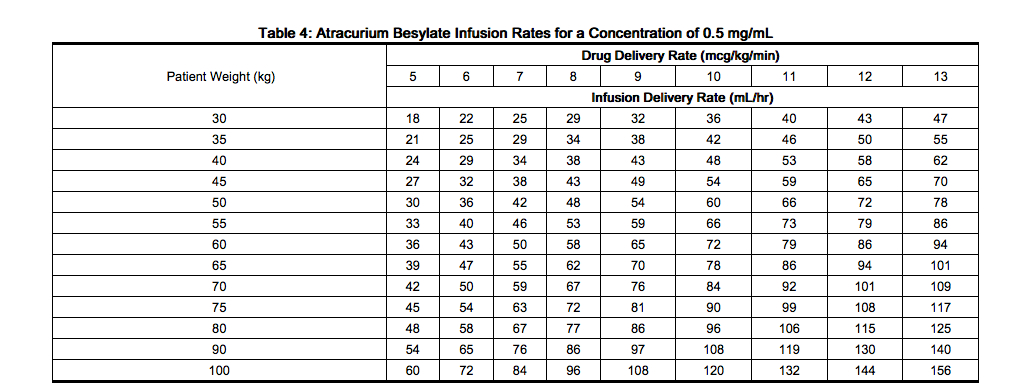
Infusion Rate Tables
- The amount of infusion solution required per minute will depend upon the concentration of atracurium in the infusion solution, the desired dose of atracurium, and the patient’s weight. The following tables provide guidelines for delivery, in mL/hr (equivalent to microdrops/min when 60 microdrops = 1 mL), of atracurium solutions in concentrations of 0.2 mg/mL (20 mg in 100 mL) or 0.5 mg/mL (50 mg in 100 mL) with an infusion pump or a gravity flow device.
|IVCompat======Compatibility and Admixtures=====
- Atracurium besylate infusion solutions may be prepared by admixing atracurium besylate injection with an appropriate diluent such as 5% Dextrose Injection, 0.9% Sodium Chloride Injection, or 5% Dextrose and 0.9% Sodium Chloride Injection. Infusion solutions should be used within 24 hours of preparation. Unused solutions should be discarded. Solutions containing 0.2 mg/mL or 0.5 mg/mL atracurium besylate in the above diluents may be stored either under refrigeration or at room temperature for 24 hours without significant loss of potency. Care should be taken during admixture to prevent inadvertent contamination. Visually inspect prior to administration.
- Spontaneous degradation of atracurium besylate has been demonstrated to occur more rapidly in Lactated Ringer’s solution than in 0.9% sodium chloride solution. Therefore, it is recommended that Lactated Ringer’s Injection not be used as a diluent in preparing solutions of atracurium besylate injection for infusion.
- Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit.
|overdose=* There has been limited experience with overdosage of atracurium besylate. The possibility of iatrogenic overdosage can be minimized by carefully monitoring muscle twitch response to peripheral nerve stimulation. Excessive doses of atracurium can be expected to produce enhanced pharmacological effects. Overdosage may increase the risk of histamine release and cardiovascular effects, especially hypotension. If cardiovascular support is necessary, this should include proper positioning, fluid administration, and the use of vasopressor agents if necessary. The patient’s airway should be assured, with manual or mechanical ventilation maintained as necessary. A longer duration of neuromuscular block may result from overdosage and a peripheral nerve stimulator should be used to monitor recovery. Recovery may be facilitated by administration of an anticholinesterase reversing agent such as neostigmine, edrophonium, or pyridostigmine, in conjunction with an anticholinergic agent such as atropine or glycopyrrolate. The appropriate package inserts should be consulted for prescribing information.
- Three pediatric patients (3 weeks, 4 and 5 months of age) unintentionally received doses of 0.8 mg/kg to 1 mg/kg of atracurium besylate. The time to 25% recovery (50 to 55 minutes) following these doses, which were 5 to 6 times the ED95 dose, was moderately longer than the corresponding time observed following doses 2 to 2.5 times the atracurium ED95 dose in infants (22 to 36 minutes). Cardiovascular changes were minimal. Nonetheless the possibility of cardiovascular changes must be considered in the case of overdose.
- An adult patient (17 years of age) unintentionally received an initial dose of 1.3 mg/kg of atracurium besylate. The time from injection to 25% recovery (83 minutes) was approximately twice that observed following maximum recommended doses in adults (35 to 45 minutes). The patient experienced moderate hemodynamic changes (13% increase in mean arterial pressure and 27% increase in heart rate) which persisted for 40 minutes and did not require treatment.
- The intravenous LD50s determined in non-ventilated male and female albino mice and male Wistar rats were 1.9, 2.01 and 1.31 mg/kg, respectively. Deaths occurred within 2 minutes and were caused by respiratory paralysis. The subcutaneous LD50 determined in non-ventilated male Wistar rats was 282.8 mg/kg. Tremors, ptosis, loss of reflexes and respiratory failure preceded death which occurred 45 to 120 minutes after injection.
|drugBox={{Drugbox2 | Verifiedfields = changed | verifiedrevid = 470456499 | IUPAC_name = 2,2'-{1,5-Pentanediylbis[oxy(3-oxo-3,1-propanediyl)]}bis[1-(3,4-dimethoxybenzyl)-6,7-dimethoxy-2-methyl-1,2,3,4-tetrahydroisoquinolinium] dibenzenesulphonate | image = Atracurium wiki.svg.png
| tradename = | Drugs.com = International Drug Names | pregnancy_category = | legal_status = Worldwide: Prescription only medicine | routes_of_administration = IV
| bioavailability = 100% (IV) | protein_bound = 82% | metabolism = Hofmann elimination (retro-Michael addition) and ester hydrolysis by nonspecific esterases | elimination_half-life = 17–21 minutes | excretion =
| CASNo_Ref =
| CAS_number_Ref =
| CAS_number = 64228-79-1
| ATC_prefix = M03
| ATC_suffix = AC04
| PubChem = 47319
| DrugBank_Ref =
| DrugBank = DB00732
| ChemSpiderID_Ref =
| ChemSpiderID = 43067
| UNII_Ref =
| UNII = 40AX66P76P
| ChEBI_Ref =
| ChEBI = 2914
| ChEMBL_Ref =
| ChEMBL = 1360
| C=53 | H=72 | N=2 | O=12 | charge = 2+
| molecular_weight = 929.145 g/mol
| smiles = O=C(OCCCCCOC(=O)CC[N+]2(C(c1c(cc(OC)c(OC)c1)CC2)Cc3ccc(OC)c(OC)c3)C)CC[N+]5(C)C(c4cc(OC)c(OC)cc4CC5)Cc6ccc(OC)c(OC)c6
| InChI = 1/C53H72N2O12/c1-54(22-18-38-32-48(62-7)50(64-9)34-40(38)42(54)28-36-14-16-44(58-3)46(30-36)60-5)24-20-52(56)66-26-12-11-13-27-67-53(57)21-25-55(2)23-19-39-33-49(63-8)51(65-10)35-41(39)43(55)29-37-15-17-45(59-4)47(31-37)61-6/h14-17,30-35,42-43H,11-13,18-29H2,1-10H3/q+2
| InChIKey = YXSLJKQTIDHPOT-UHFFFAOYAF
| StdInChI_Ref =
| StdInChI = 1S/C53H72N2O12/c1-54(22-18-38-32-48(62-7)50(64-9)34-40(38)42(54)28-36-14-16-44(58-3)46(30-36)60-5)24-20-52(56)66-26-12-11-13-27-67-53(57)21-25-55(2)23-19-39-33-49(63-8)51(65-10)35-41(39)43(55)29-37-15-17-45(59-4)47(31-37)61-6/h14-17,30-35,42-43H,11-13,18-29H2,1-10H3/q+2
| StdInChIKey_Ref =
| StdInChIKey = YXSLJKQTIDHPOT-UHFFFAOYSA-N
}}
|mechAction=* Atracurium besylate is a nondepolarizing skeletal muscle relaxant. Nondepolarizing agents antagonize the neurotransmitter action of acetylcholine by binding competitively with cholinergic receptor sites on the motor end-plate. This antagonism is inhibited, and neuromuscular block reversed, by acetylcholinesterase inhibitors such as neostigmine, edrophonium, and pyridostigmine.
|structure=* Atracurium besylate is an intermediate-duration, nondepolarizing, skeletal muscle relaxant for intravenous administration. Atracurium besylate is designated as 2-(2-Carboxyethyl)-1,2,3,4-tetrahydro-6,7-dimethoxy-2-methyl-1-veratrylisoquinolinium benzenesulfonate, pentamethylene ester. It has a molecular weight of 1243.49, and its molecular formula is C65H82N2O18S2. The structural formula is:
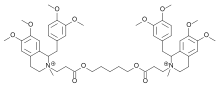
- Atracurium besylate is a complex molecule containing four sites at which different stereochemical configurations can occur. The symmetry of the molecule, however, results in only ten, instead of sixteen, possible different isomers. The manufacture of atracurium besylate results in these isomers being produced in unequal amounts but with a consistent ratio. Those molecules in which the methyl group attached to the quaternary nitrogen projects on the opposite side to the adjacent substituted-benzyl moiety predominate by approximately 3:1.
- Atracurium Besylate Injection USP is a sterile, non-pyrogenic aqueous solution. Each mL contains 10 mg atracurium besylate. The pH is adjusted to 3.00 to 3.65 with benzenesulfonic acid. The multiple dose vial contains 0.9% benzyl alcohol added as a preservative. Atracurium besylate injection slowly loses potency with time at the rate of approximately 6% per year under refrigeration (5°C). Atracurium besylate injection should be refrigerated at 2°C to 8°C (36°F to 46°F) to preserve potency. Rate of loss in potency increases to approximately 5% per month at 25°C (77°F). Upon removal from refrigeration to room temperature storage conditions (25°C / 77°F), use atracurium besylate injection within 14 days even if rerefrigerated.
|PD=* Atracurium can be used most advantageously if muscle twitch response to peripheral nerve stimulation is monitored to assess degree of muscle relaxation.
- The duration of neuromuscular block produced by atracurium is approximately one-third to one-half the duration of block by d-tubocurarine, metocurine, and pancuronium at initially equipotent doses. As with other nondepolarizing neuromuscular blockers, the time to onset of paralysis decreases and the duration of maximum effect increases with increasing atracurium doses.
- The ED95 (dose required to produce 95% suppression of the muscle twitch response with balanced anesthesia) has averaged 0.23 mg/kg (0.11 to 0.26 mg/kg in various studies). An initial atracurium dose of 0.4 to 0.5 mg/kg generally produces maximum neuromuscular block within 3 to 5 minutes of injection, with good or excellent intubation conditions within 2 to 2.5 minutes in most patients. Recovery from neuromuscular block (under balanced anesthesia) can be expected to begin approximately 20 to 35 minutes after injection. Under balanced anesthesia, recovery to 25% of control is achieved approximately 35 to 45 minutes after injection, and recovery is usually 95% complete approximately 60 to 70 minutes after injection. The neuromuscular blocking action of atracurium is enhanced in the presence of potent inhalation anesthetics. Isoflurane and enflurane increase the potency of atracurium and prolong neuromuscular block by approximately 35%; however, halothane’s potentiating effect (approximately 20%) is marginal (see Dosage and administration).
- Repeated administration of maintenance doses of atracurium has no cumulative effect on the duration of neuromuscular block if recovery is allowed to begin prior to repeat dosing. Moreover, the time needed to recover from repeat doses does not change with additional doses. Repeat doses can therefore be administered at relatively regular intervals with predictable results. After an initial dose of 0.4 to 0.5 mg/kg under balanced anesthesia, the first maintenance dose (suggested maintenance dose is 0.08 to 0.10 mg/kg) is generally required within 20 to 45 minutes, and subsequent maintenance doses are usually required at approximately 15 to 25 minute intervals.
- Once recovery from atracurium’s neuromuscular blocking effects begins, it proceeds more rapidly than recovery from d-tubocurarine, metocurine, and pancuronium. Regardless of the atracurium dose, the time from start of recovery (from complete block) to complete (95%) recovery is approximately 30 minutes under balanced anesthesia, and approximately 40 minutes under halothane, enflurane or isoflurane. Repeated doses have no cumulative effect on recovery rate.
- Reversal of neuromuscular block produced by atracurium can be achieved with an anti-cholinesterase agent such as neostigmine, edrophonium, or pyridostigmine, in conjunction with an anticholinergic agent such as atropine or glycopyrrolate. Under balanced anesthesia, reversal can usually be attempted approximately 20 to 35 minutes after an initial atracurium besylate dose of 0.4 to 0.5 mg/kg, or approximately 10 to 30 minutes after a 0.08 to 0.10 mg/kg maintenance dose, when recovery of muscle twitch has started. Complete reversal is usually attained within 8 to 10 minutes of the administration of reversing agents. Rare instances of breathing difficulties, possibly related to incomplete reversal, have been reported following attempted pharmacologic antagonism of atracurium-induced neuromuscular block. As with other agents in this class, the tendency for residual neuromuscular block is increased if reversal is attempted at deep levels of block or if inadequate doses of reversal agents are employed.
- The pharmacokinetics of atracurium in humans are essentially linear within the 0.3 to 0.6 mg/kg dose range. The elimination half-life is approximately 20 minutes. The duration of neuromuscular block produced by atracurium besylate does not correlate with plasma pseudocholinesterase levels and is not altered by the absence of renal function. This is consistent with the results of in vitro studies which have shown that atracurium is inactivated in plasma via two nonoxidative pathways: ester hydrolysis, catalyzed by nonspecific esterases; and Hofmann elimination, a nonenzymatic chemical process which occurs at physiological pH. Some placental transfer occurs in humans.
- Radiolabel studies demonstrated that atracurium undergoes extensive degradation in cats, and that neither kidney nor liver plays a major role in this elimination. Biliary and urinary excretion were the major routes of excretion of radioactivity (totaling >90% of the labeled dose within 7 hours of dosing), of which atracurium represented only a minor fraction. The metabolites in bile and urine were similar, including products of Hofmann elimination and ester hydrolysis.
- Elderly patients may have slightly altered pharmacokinetic parameters compared to younger patients, with a slightly decreased total plasma clearance which is offset by a corresponding increase in volume of distribution. The net effect is that there has been no significant difference in clinical duration and recovery from neuromuscular block observed between elderly and younger patients receiving atracurium besylate.
- Atracurium is a less potent histamine releaser than d-tubocurarine or metocurine. Histamine release is minimal with initial atracurium besylate doses up to 0.5 mg/kg, and hemodynamic changes are minimal within the recommended dose range. A moderate histamine release and significant falls in blood pressure have been seen following 0.6 mg/kg of atracurium besylate. The histamine and hemodynamic responses were poorly correlated. The effects were generally short-lived and manageable, but the possibility of substantial histamine release in sensitive individuals or in patients in whom substantial histamine release would be especially hazardous (e.g., patients with significant cardiovascular disease) must be considered.
- It is not known whether the prior use of other nondepolarizing neuromuscular blocking agents has any effect on the activity of atracurium. The prior use of succinylcholine decreases by approximately 2 to 3 minutes the time to maximum block induced by atracurium besylate, and may increase the depth of block. Atracurium should be administered only after a patient recovers from succinylcholine-induced neuromuscular block.
|howSupplied=* Atracurium Besylate Injection USP, each mL containing 10 mg atracurium besylate, is supplied as follows:
- NDC 0409-1109-01. 5 mL Single Dose Vial (50 mg atracurium besylate per vial). Carton of 10.
- NDC 0409-1105-02. 10 mL Multiple Dose Vial (100 mg atracurium besylate per vial). Contains benzyl alcohol (see Warnings). Carton of 10.
- Atracurium Besylate Injection should be refrigerated at 2°C to 8°C (36°F to 46°F) to preserve potency. Do not freeze. Protect from light. Keep vials in carton until time of use.
- Upon removal from refrigeration to room temperature storage conditions (25°C/77°F), use Atracurium Besylate Injection within 14 days even if rerefrigerated.
- Manufactured by:
- Gland Pharma Limited;
- Hyderabad 500043, India
- Manufactured for:
- Hospira, Inc.
- Lake Forest, IL 60045 USA
- Product of India
- M.L.No.: 103/AP/RR/97/F/R
- Revised: February 2012
- EN-3011
|alcohol=Alcohol-Atracurium interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication. }} {{#subobject:
|Label Page=Atracurium |Label Name=Atracurium label.png
}}