Brain tumor: Difference between revisions
No edit summary |
m (Bot: Removing from Primary care) |
||
| (59 intermediate revisions by 10 users not shown) | |||
| Line 1: | Line 1: | ||
<br />__NOTOC__ | |||
{{Infobox_Disease | {{Infobox_Disease | ||
| Name = Brain tumor | | Name = Brain tumor | ||
| Image = | | Image = Hirnmetastase_MRT-T1_KM.jpg | ||
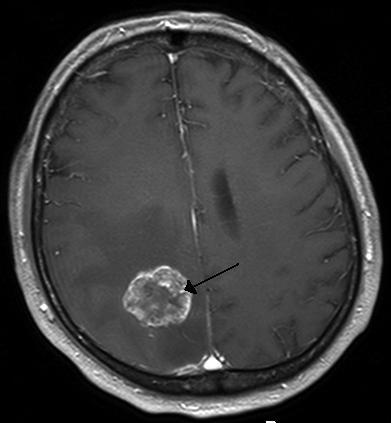
| Caption = [[Computed tomography|CT scan]] of brain showing brain cancer to left [[parietal lobe]] in the [[ventricular system|peri-ventricular]] area. | | Caption = [[Computed tomography|CT scan]] of brain showing brain cancer to left [[parietal lobe]] in the [[ventricular system|peri-ventricular]] area.https://en.wikipedia.org/wiki/File:Hirnmetastase_MRT-T1_KM.jpg | ||
}} | }} | ||
{{ | {{Brain tumor}} | ||
{{ | '''For patient information click [[{{PAGENAME}} (patient information)|here]]''' | ||
{{ | {{CMG}} '''Assosciate editor(s)-In-Chief''' {{Fs}}, [[Prashanth Saddala]], {{SR}} | ||
{{SK}} Brain tumour; brain cancer; intracranial tumor; astrocytoma; glioblastoma; oligodendrocytoma; meningioma; ependymoma; craniopharyngioma. | |||
==[[Brain tumor overview|Overview]]== | |||
==Classification== | ==[[Brain tumor classification|Classification]]== | ||
=== | Brain tumors can be classified as follows: | ||
{{Family tree/start}} | |||
{{Family tree | | | | | | | | | | | | A01 | | | | | | | | | | | | A01=Brain tumors}} | |||
{{Family tree | | | | | | |,|-|-|-|-|-|+|-|-|-|-|-|.| | | | | | | }} | |||
{{Family tree | | | | | | B01 | | | | B02 | | | | B03 | | | | | | B01=Adult primary brain tumor|B02=Childhood primary brain tumor|B03=Brain metastase}} | |||
{{Family tree | | | | | | |!| | | | | |!| | | | | |!| | | | | | | }} | |||
{{Family tree |boxstyle=text-align: left; | | | | | C01 | | | | C02 | | | | | C03 | | | | | | C01=<br>•Glioblastoma multiforme<br>•Oligodendroglioma<br>•Meningioma<br>•Hemangioblastoma<br>•Pituitary adenoma<br>•Schwannoma<br>•Primary CNS lymphoma|C02=<br>•Pilocytic astrocytoma<br>•Medulloblastoma<br>•Ependymoma<br>•Craniopharyngioma<br>•Pinealoma|C03=<br>•Lung cancer<br>•Breast cancer<br>•Melanoma<br>•Gastrointestinal tract cancer<br>•Renal cell carcinoma<br>•Osteosarcoma<br>•Head and neck cancer<br>•Neuroblastoma<br>•Lymphoma<br>•Prostate cancer}} | |||
{{Family tree | | | | | | | | | | | | | | | | | | | | | | | | | | }} | |||
{{Family tree | | | | | | | | | | | | | | | | | | | | | | | | | | }} | |||
{{Family tree | | | | | | | | | | | | | | | | | | | | | | | | | | }} | |||
{{Family tree | | | | | | | | | | | | | | | | | | | | | | | | | | }} | |||
{{Family tree | | | | | | | | | | | | | | | | | | | | | | | | | | }} | |||
{{Family tree | | | | | | | | | | | | | | | | | | | | | | | | | | }} | |||
{{Family tree/end}} | |||
<br /> | |||
==[[Brain tumor causes|Causes]]== | |||
The exact cause of brain tumor is not known. | |||
==[[Brain tumor differential diagnosis|Differentiating Brain Tumor from other Diseases]]== | |||
On the basis of [[seizure]], [[visual disturbance]], and constitutional symptoms, brain tumors must be differentiated from [[Arteriovenous malformation|AV malformation]], [[brain aneurysm]], [[bacterial]] [[brain]] [[abscess]], [[tuberculosis]], [[toxoplasmosis]], [[hydatid cyst]], [[CNS]] [[cryptococcosis]], [[CNS]] [[aspergillosis]], and [[brain metastasis]]. | |||
{| | |||
|- style="background: #4479BA; color: #FFFFFF; text-align: center;" | |||
! rowspan="4" |Diseases | |||
| colspan="5" rowspan="1" style="background: #4479BA; color: #FFFFFF; text-align: center;" |'''Clinical manifestations''' | |||
! colspan="3" rowspan="2" |Para-clinical findings | |||
| colspan="1" rowspan="4" style="background: #4479BA; color: #FFFFFF; text-align: center;" |'''Gold<br>standard''' | |||
! rowspan="4" style="background: #4479BA; color: #FFFFFF; text-align: center;" |Additional findings | |||
|- | |||
| colspan="4" rowspan="2" style="background: #4479BA; color: #FFFFFF; text-align: center;" |'''Symptoms''' | |||
! rowspan="2" style="background: #4479BA; color: #FFFFFF; text-align: center;" |Physical examination | |||
|- | |||
! rowspan="2" style="background: #4479BA; color: #FFFFFF; text-align: center;" |Lab Findings | |||
! rowspan="2" style="background: #4479BA; color: #FFFFFF; text-align: center;" |MRI | |||
! rowspan="2" style="background: #4479BA; color: #FFFFFF; text-align: center;" |Immunohistopathology | |||
|- | |||
! style="background: #4479BA; color: #FFFFFF; text-align: center;" |Head-<br>ache | |||
! style="background: #4479BA; color: #FFFFFF; text-align: center;" |Seizure | |||
! style="background: #4479BA; color: #FFFFFF; text-align: center;" |Visual disturbance | |||
! colspan="1" rowspan="1" style="background: #4479BA; color: #FFFFFF; text-align: center;" |Constitutional | |||
! style="background: #4479BA; color: #FFFFFF; text-align: center;" |Focal neurological deficit | |||
|- | |||
! colspan="11" style="background: #7d7d7d; color: #FFFFFF; padding: 5px; text-align: center;" |Adult primary brain tumors | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Glioblastoma multiforme]]<br> | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |− | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Supratentorial]] | |||
* Irregular ring-nodular enhancing lesions | |||
* Central [[necrosis]] | |||
* Surrounding [[vasogenic edema]] | |||
* Cross [[corpus callosum]] ([[butterfly glioma]]) | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Astrocyte]] origin | |||
* [[Pleomorphism|Pleomorphic]] cell | |||
* Pseudopalisading appearance | |||
* [[GFAP]] + | |||
* [[Necrosis]] + | |||
* [[Hemorrhage]] + | |||
* [[Vascular]] prolifration + | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Biopsy]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* Highest [[incidence]] in fifth and sixth decades of life | |||
* Most of the time, focal [[neurological]] deficit is the presenting [[Sign (medical)|sign]]. | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Oligodendroglioma]]<br> | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | − | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | − | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* Almost always in [[Cerebral hemisphere|cerebral hemisphers]] ([[Frontal lobe|frontal lobes]]) | |||
* Hypointense on T1 | |||
* Hyperintense on T2 | |||
* [[Calcification]] | |||
* Chicken wire capillary pattern | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Oligodendrocyte]] origin | |||
* [[Calcification]] + | |||
* Fried egg cell appearance | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Biopsy]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* Highest [[incidence]] is between 40 and 50 years of age. | |||
* Most of the time, [[epileptic seizure]] is the presenting [[Sign (medicine)|sign]]. | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Meningioma]]<br> | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | − | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | − | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* Well circumscribed | |||
* Extra-axial [[mass]] | |||
* [[Meninges|Dural]] attachment | |||
* [[CSF]] [[vascular]] cleft sign | |||
* Sunburst appearance of the [[Vessel|vessels]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Arachnoid]] origin | |||
* [[Psammoma body|Psammoma bodies]] | |||
== | * Whorled spindle cell pattern | ||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Biopsy]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* Highest [[incidence]] is between 40 and 50 years of age. | |||
* Most of the time, focal [[neurological]] deficit and [[epileptic seizure]] are the presenting [[signs]]. | |||
* May be associated with [[Neurofibromatosis type II|NF-2]] | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Hemangioblastoma]]<br> | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | − | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | − | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Infratentorial]] | |||
* [[Cyst|Cystic]] lesion with a solid enhancing mural [[nodule]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Blood vessel]] origin | |||
== | * [[Capillary|Capillaries]] with thin walls | ||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Biopsy]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* Might secret [[erythropoietin]] and cause [[polycythemia]] | |||
* May be associated with [[Von Hippel-Lindau Disease|von hippel-lindau syndrome]] | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Pituitary adenoma]]<br><ref name=":0" /> | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | − | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | − | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + [[Bitemporal hemianopia]] | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | − | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | − | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Endocrine]] abnormalities as a result of [[Pituitary adenoma|functional adenomas]] or pressure effect of non-functional [[Adenoma|adenomas]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* Isointense to normal [[pituitary gland]] in T1 | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Endocrine]] cell [[hyperplasia]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Biopsy]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* It is associated with [[MEN1]] disease. | |||
* Initialy presents with upper bitemporal quadrantanopsia followed by [[Bitemporal hemianopia|bitemporal hemianopsia]] (pressure on [[Optic chiasm|optic chiasma]] from below) | |||
* | |||
* | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Schwannoma]]<br> | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | − | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | − | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | − | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | − | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | − | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* Split-fat sign | |||
* Fascicular sign | |||
* Often have areas of [[hemosiderin]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Schwann cell]] origin | |||
* S100+ | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Biopsy]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* It causes [[hearing loss]] and [[tinnitus]] | |||
* May be associated with [[Neurofibromatosis type II|NF-2]] (bilateral [[Schwannoma|schwannomas]]) | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Primary central nervous system lymphoma|Primary CNS lymphoma]]<br> | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | − | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | − | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* Usually deep in the [[white matter]] | |||
* Single [[mass]] with ring enhancement | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[B cell]] origin | |||
* Similar to [[Non-Hodgkin lymphoma|non hodgkin lymphoma]] ([[Diffuse large B cell lymphoma|diffuse large B cell]]) | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Biopsy]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* Usually in young [[immunocompromised]] patients ([[HIV]]) or old [[immunocompetent]] person. | |||
* | |||
|- | |||
! colspan="11" style="background: #7d7d7d; color: #FFFFFF; padding: 5px; text-align: center;" |Childhood primary brain tumors | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Pilocytic astrocytoma]]<br> | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | − | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | − | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Infratentorial]] | |||
* Solid and [[Cyst|cystic]] component | |||
* Mostly in [[posterior fossa]] | |||
* Usually in [[Cerebellar hemisphere|cerebellar hemisphers]] and [[Cerebellar vermis|vermis]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Glial cell]] origin | |||
*Solid and [[Cyst|cystic]] component | |||
* [[GFAP]] + | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Biopsy]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* Most of the time, [[Cerebellum|cerebellar]] dysfunction is the presenting [[signs]]. | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Medulloblastoma]]<br> | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | − | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | − | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Infratentorial]] | |||
* Mostly in [[cerebellum]] | |||
== | * Non communicating [[hydrocephalus]] | ||
< | | style="background: #F5F5F5; padding: 5px;" | | ||
* [[Neuroectoderm]] origin | |||
* Homer wright rosettes | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Biopsy]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Drop metastasis]] ([[metastasis]] through [[CSF]]) | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Ependymoma]]<br><ref name=":0" /> | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | − | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | − | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Infratentorial]] | |||
* Usually found in [[Fourth ventricle|4th ventricle]] | |||
* Mixed [[Cyst|cystic]]/solid [[lesion]] | |||
* Hydrocephalus | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Ependymal cell]] origin | |||
* Peri[[vascular]] pseudorosette | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Biopsy]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* Causes an unusually persistent, continuous [[headache]] in children. | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Craniopharyngioma]]<br><ref name=":0" /> | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + [[Bitemporal hemianopia]] | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | − | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Hypopituitarism]] as a result of pressure effect on [[pituitary gland]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Calcification]] | |||
* Lobulated contour | |||
* Motor-oil like fluid within [[tumor]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Ectoderm|Ectodermal]] origin ([[Rathke's pouch|Rathkes pouch]]) | |||
* [[Calcification]] + | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Biopsy]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* Initialy presents with lower bitemporal quadrantanopsia followed by [[Bitemporal hemianopia|bitemporal hemianopsia]] (pressure on [[Optic chiasm|optic chiasma]] from above) | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Pinealoma]]<br> | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | − | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + vertical gaze palsy | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* B-hCG rise leads to [[precocious puberty]] in [[Male|males]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Hydrocephalus]] (compression of [[cerebral aqueduct]]) | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* Similar to [[testicular seminoma]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Biopsy]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* May cause prinaud syndrome ([[Vertical gaze center|vertical gaze]] palsy, pupillary light-near dissociation, lid retraction and convergence-retraction [[nystagmus]] | |||
|- | |||
! colspan="11" style="background: #7d7d7d; color: #FFFFFF; padding: 5px; text-align: center;" |Vascular | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Arteriovenous malformation|AV malformation]]<br><ref name=":0" /> | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | − | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | − | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Supratentorial]]: ~85% | |||
* Flow voids on T2 weighted images | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* We do not perform [[biopsy]] for [[AVM]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Angiography]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* We may see bag of worms appearance in [[CT angiography]] | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Brain aneurysm]]<br> | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | − | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | − | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* In [[magnetic resonance angiography]], we may see [[aneurysm]] mostly in anterior circulation (~85%) | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* We do not perform [[biopsy]] for [[brain aneurysm]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* MRA and CTA | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* It is associated with [[autosomal dominant polycystic kidney disease]], [[Ehlers-Danlos syndrome]], [[pseudoxanthoma elasticum]] and [[Bicuspid aortic valve]] | |||
* ([[Angiography]] is reserved for patients who have negative [[Magnetic resonance angiography|MRA]] and [[CT angiography|CTA]]) | |||
|- | |||
! colspan="11" style="background: #7d7d7d; color: #FFFFFF; padding: 5px; text-align: center;" |Infectious | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |Bacterial [[brain abscess]]<br> | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Leukocytosis]] | |||
* Elevated [[ESR]] | |||
* [[Blood culture]] may be positive for underlying [[organism]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* Central hypodense signal and surrounding ring-enhancement in T1 | |||
* Central hyperintense area surrounded by a well-defined hypointense capsule with surrounding [[edema]] in T2 | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* We do not perform [[biopsy]] for [[brain abscess]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* History/ imaging | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* The most common causes of [[brain abscess]] are [[Streptococcus]] and [[Staphylococcus]]. | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Tuberculosis]]<br><ref name=":0" /> | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* Positive [[acid-fast bacilli]] ([[AFB]]) smear in [[CSF]] specimen | |||
* Positive [[CSF]] [[nucleic acid]] amplification testing | |||
* [[Hyponatremia]] (inappropriate secretion of [[antidiuretic hormone]]) | |||
* Mild [[anemia]] | |||
* [[Leukocytosis]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Hydrocephalus]] combined with marked basilar [[Meninges|meningeal]] enhancement | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* We do not perform [[biopsy]] for [[brain]] [[tuberculosis]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* Lab data/ Imaging | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* It is associated with [[HIV]] [[infection]] | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Toxoplasmosis]]<br> | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | − | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* Normal [[CSF]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* Multifocal [[Mass|masses]] with ring enhancement | |||
* Mostly in [[basal ganglia]], [[thalami]], and corticomedullary junction. | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* We do not perform [[biopsy]] for brain [[toxoplasmosis]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* History/ imaging | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* It is associated with [[HIV]] [[infection]] | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Hydatid cyst]]<br><ref name=":0" /> | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align: left;" | | |||
* Positive [[serology]] ([[Antibody]] detection for [[E. granulosus]]'')'' | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* Honeycomb appearance | |||
* [[Necrotic]] area | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* We do not perform [[biopsy]] for [[Hydatid cyst|hydatid cysts]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* Imaging | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Brain]], [[eye]], and [[Spleen|splenic]] [[Cyst|cysts]] may not produce detectable amount of [[antibodies]] | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[CNS]] [[cryptococcosis]]<br> | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* Positive [[CSF]] [[antigen]] testing ([[coccidioidomycosis]]) | |||
* [[CSF]] [[Lymphocyte|lymphocytic]] [[pleocytosis]] | |||
* Elevated [[CSF]] [[Protein|proteins]] and [[lactate]] | |||
* Low [[CSF]] [[glucose]] | |||
* | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* Dilated peri[[vascular]] spaces | |||
* [[Basal ganglia]] [[Pseudocyst|pseudocysts]] | |||
* Soap bubble brain lesions ([[cryptococcus neoformans]]) | |||
* | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* We may see numerous acutely branching septate [[Hypha|hyphae]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Laboratory|Lab]] data/ Imaging | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* It is the most common [[brain]] [[fungal infection]] | |||
* It is associated with [[HIV]], [[Immunosuppressive therapy|immunosuppressive therapies]], and [[Organ transplant|organ transplants]] | |||
* In may happen in [[immunocompetent]] patients undergoing invasive procedures ( [[neurosurgery]]) or exposed to [[Contamination|contaminated]] devices or [[drugs]] | |||
* Since [[brain]] [[Biopsy|biopsies]] are highly invasive and may may cause [[neurological]] deficits, we [[diagnose]] [[CNS]] [[fungal]] [[Infection|infections]] based on [[laboratory]] and imaging findings | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[CNS]] [[aspergillosis]]<br> | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* Positive [[galactomannan]] [[antigen]] testing ([[aspergillosis]]) | |||
* [[CSF]] [[Lymphocyte|lymphocytic]] [[pleocytosis]] | |||
* Elevated [[CSF]] [[Protein|proteins]] and [[lactate]] | |||
* Low [[CSF]] [[glucose]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* Multiple [[Abscess|abscesses]] | |||
* Ring enhancement | |||
* Peripheral low signal intensity on T2 | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* We may see numerous acutely branching septate [[Hypha|hyphae]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Laboratory|Lab]] data/ Imaging | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* It is associated with [[HIV]], [[Immunosuppressive therapy|immunosuppressive therapies]], and [[Organ transplant|organ transplants]] | |||
* In may happen in [[immunocompetent]] patients undergoing invasive procedures ( [[neurosurgery]]) or exposed to [[Contamination|contaminated]] devices or [[drugs]] | |||
* Since [[brain]] [[Biopsy|biopsies]] are highly invasive and may may cause [[neurological]] deficits, we [[diagnose]] [[CNS]] [[fungal]] [[Infection|infections]] based on [[laboratory]] and imaging findings | |||
|- | |||
! colspan="11" style="background: #7d7d7d; color: #FFFFFF; padding: 5px; text-align: center;" |Other | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Brain metastasis]]<br><ref name=":0" /> | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | − | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* Multiple [[Lesion|lesions]] | |||
* [[Vasogenic edema]] | |||
* | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* Based on the primary [[cancer]] type we may have different immunohistopathology findings. | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* History/ imaging | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* Most common primary [[Tumor|tumors]] that [[metastasis]] to [[brain]]: | |||
** [[Lung cancer]] | |||
** [[Renal cell carcinoma]] | |||
** [[Breast cancer]] | |||
** [[Melanoma]] | |||
** [[Gastrointestinal tract]] | |||
* If there is any uncertainty about [[etiology]], [[biopsy]] should be performed | |||
|} | |||
'''ABBREVIATIONS''' | |||
[[ | [[CNS]]=[[Central nervous system]], AV=Arteriovenous, [[CSF]]=[[Cerebrospinal fluid]], [[NF-2]]=[[Neurofibromatosis type 2]], [[MEN1|MEN-1]]=[[Multiple endocrine neoplasia]], [[GFAP]]=[[Glial fibrillary acidic protein]], [[HIV]]=[[Human Immunodeficiency Virus|Human immunodeficiency virus]], BhCG=[[Human chorionic gonadotropin]], [[ESR]]=[[Erythrocyte sedimentation rate]], [[AFB]]=Acid fast bacilli, [[Magnetic resonance angiography|MRA]]=[[Magnetic resonance angiography]], [[CT angiography|CTA]]=[[CT angiography]] | ||
[[ | |||
[[ | |||
[[ | |||
[[ | |||
== References == | |||
[[fr:Tumeur du cerveau]] | [[fr:Tumeur du cerveau]] | ||
[[ja:脳腫瘍]] | [[ja:脳腫瘍]] | ||
[[pt:Tumor cerebral]] | [[pt:Tumor cerebral]] | ||
[[ru:Опухоли мозга]] | [[ru:Опухоли мозга]] | ||
[[tr:Beyin tümörü]] | [[tr:Beyin tümörü]] | ||
[[zh:腦癌]] | [[zh:腦癌]] | ||
{{WikiDoc Help Menu}} | {{WikiDoc Help Menu}} | ||
{{WikiDoc Sources}} | {{WikiDoc Sources}} | ||
<references /> | |||
[[Category:Disease]] | |||
[[Category:Brain]] | |||
[[Category:Oncology]] | |||
[[Category:Neurology]] | |||
[[Category:Up-To-Date]] | |||
[[Category:Medicine]] | |||
[[Category:Neurosurgery]] | |||
Latest revision as of 20:41, 29 July 2020
| Brain tumor | |
 | |
|---|---|
| CT scan of brain showing brain cancer to left parietal lobe in the peri-ventricular area.https://en.wikipedia.org/wiki/File:Hirnmetastase_MRT-T1_KM.jpg |
|
Brain tumor Microchapters |
For patient information click here
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Assosciate editor(s)-In-Chief Fahimeh Shojaei, M.D., Prashanth Saddala, Sujit Routray, M.D. [2]
Synonyms and keywords: Brain tumour; brain cancer; intracranial tumor; astrocytoma; glioblastoma; oligodendrocytoma; meningioma; ependymoma; craniopharyngioma.
Overview
Classification
Brain tumors can be classified as follows:
| Brain tumors | |||||||||||||||||||||||||||||||||||||||||||||||||||
| Adult primary brain tumor | Childhood primary brain tumor | Brain metastase | |||||||||||||||||||||||||||||||||||||||||||||||||
•Glioblastoma multiforme •Oligodendroglioma •Meningioma •Hemangioblastoma •Pituitary adenoma •Schwannoma •Primary CNS lymphoma | •Pilocytic astrocytoma •Medulloblastoma •Ependymoma •Craniopharyngioma •Pinealoma | •Lung cancer •Breast cancer •Melanoma •Gastrointestinal tract cancer •Renal cell carcinoma •Osteosarcoma •Head and neck cancer •Neuroblastoma •Lymphoma •Prostate cancer | |||||||||||||||||||||||||||||||||||||||||||||||||
Causes
The exact cause of brain tumor is not known.
Differentiating Brain Tumor from other Diseases
On the basis of seizure, visual disturbance, and constitutional symptoms, brain tumors must be differentiated from AV malformation, brain aneurysm, bacterial brain abscess, tuberculosis, toxoplasmosis, hydatid cyst, CNS cryptococcosis, CNS aspergillosis, and brain metastasis.
| Diseases | Clinical manifestations | Para-clinical findings | Gold standard |
Additional findings | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Symptoms | Physical examination | |||||||||
| Lab Findings | MRI | Immunohistopathology | ||||||||
| Head- ache |
Seizure | Visual disturbance | Constitutional | Focal neurological deficit | ||||||
| Adult primary brain tumors | ||||||||||
| Glioblastoma multiforme |
+ | +/− | +/− | − | + | − |
|
|
| |
| Oligodendroglioma |
+ | + | +/− | − | + | − |
|
|
| |
| Meningioma |
+ | +/− | +/− | − | + | − |
|
|
| |
| Hemangioblastoma |
+ | +/− | +/− | − | + | − |
|
| ||
| Pituitary adenoma [1] |
− | − | + Bitemporal hemianopia | − | − |
|
|
|
| |
| Schwannoma |
− | − | − | − | + | − |
|
|
| |
| Primary CNS lymphoma |
+ | +/− | +/− | − | + | − |
|
|
| |
| Childhood primary brain tumors | ||||||||||
| Pilocytic astrocytoma |
+ | +/− | +/− | − | + | − |
|
|
| |
| Medulloblastoma |
+ | +/− | +/− | − | + | − |
|
|
| |
| Ependymoma [1] |
+ | +/− | +/− | − | + | − |
|
|
| |
| Craniopharyngioma [1] |
+ | +/− | + Bitemporal hemianopia | − | + |
|
|
|
| |
| Pinealoma |
+ | +/− | +/− | − | + vertical gaze palsy |
|
|
|
| |
| Vascular | ||||||||||
| AV malformation [1] |
+ | + | +/− | − | +/− | − |
|
| ||
| Brain aneurysm |
+ | +/− | +/− | − | +/− | − |
|
|
|
|
| Infectious | ||||||||||
| Bacterial brain abscess |
+ | +/− | +/− | + | + |
|
|
|
|
|
| Tuberculosis [1] |
+ | +/− | +/− | + | + |
|
|
|
|
|
| Toxoplasmosis |
+ | +/− | +/− | − | + |
|
|
|
|
|
| Hydatid cyst [1] |
+ | +/− | +/− | +/− | + |
|
|
|
|
|
| CNS cryptococcosis |
+ | +/− | +/− | + | + |
|
|
|
|
|
| CNS aspergillosis |
+ | +/− | +/− | + | + |
|
|
|
|
|
| Other | ||||||||||
| Brain metastasis [1] |
+ | +/− | +/− | + | + | − |
|
|
|
|
ABBREVIATIONS
CNS=Central nervous system, AV=Arteriovenous, CSF=Cerebrospinal fluid, NF-2=Neurofibromatosis type 2, MEN-1=Multiple endocrine neoplasia, GFAP=Glial fibrillary acidic protein, HIV=Human immunodeficiency virus, BhCG=Human chorionic gonadotropin, ESR=Erythrocyte sedimentation rate, AFB=Acid fast bacilli, MRA=Magnetic resonance angiography, CTA=CT angiography