Nonsuicidal self-injury: Difference between revisions
| Line 74: | Line 74: | ||
|+Differential diagnosis of Nonsuicidal self-injury<ref name="urlRedirecting">{{cite web |url=https://doi.org/10.1016/j.amjmed.2005.09.027 |title=Redirecting |format= |work= |accessdate=}}</ref><ref name="urlDSM-5">{{cite web |url=https://www.psychiatry.org/psychiatrists/practice/dsm |title=DSM-5 |format= |work= |accessdate=}}</ref><ref name="pmid7802127">{{cite journal |vauthors=Foa EB, Kozak MJ, Goodman WK, Hollander E, Jenike MA, Rasmussen SA |title=DSM-IV field trial: obsessive-compulsive disorder |journal=Am J Psychiatry |volume=152 |issue=1 |pages=90–6 |date=January 1995 |pmid=7802127 |doi=10.1176/ajp.152.1.90 |url=}}</ref> | |+Differential diagnosis of Nonsuicidal self-injury<ref name="urlRedirecting">{{cite web |url=https://doi.org/10.1016/j.amjmed.2005.09.027 |title=Redirecting |format= |work= |accessdate=}}</ref><ref name="urlDSM-5">{{cite web |url=https://www.psychiatry.org/psychiatrists/practice/dsm |title=DSM-5 |format= |work= |accessdate=}}</ref><ref name="pmid7802127">{{cite journal |vauthors=Foa EB, Kozak MJ, Goodman WK, Hollander E, Jenike MA, Rasmussen SA |title=DSM-IV field trial: obsessive-compulsive disorder |journal=Am J Psychiatry |volume=152 |issue=1 |pages=90–6 |date=January 1995 |pmid=7802127 |doi=10.1176/ajp.152.1.90 |url=}}</ref> | ||
|- | |- | ||
! | !Name of the condition !!Characteristic features | ||
|- | |- | ||
|Post-traumatic Stress disorder||Reliving the [[Incident report|incident]] with distressing recollections, [[Flashback (psychological phenomenon)|flashback]]<nowiki/>s, [[dream]]<nowiki/>s, and/or [[Physical activity|physical]] and [[psychological]] distress, [[Avoidance reaction|avoidance]] of events that might trigger experiences or [[memories]] of the [[trauma]], and increased [[arousal]]. | |Post-traumatic Stress disorder||Reliving the [[Incident report|incident]] with distressing recollections, [[Flashback (psychological phenomenon)|flashback]]<nowiki/>s, [[dream]]<nowiki/>s, and/or [[Physical activity|physical]] and [[psychological]] distress, [[Avoidance reaction|avoidance]] of events that might trigger experiences or [[memories]] of the [[trauma]], and increased [[arousal]]. | ||
Revision as of 18:33, 14 August 2021
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1];Associate Editor(s)-in-Chief: Sunita Kumawat, M.B.B.S[2]
Synonyms and keywords: Self-harm (SH), Self-inflicted violence (SIV), self-injury (SI), Non suicidal self injury (NSSI) or self-injurious behavior (SIB),
Overview
Non-suicidal Self Injury means the intentional or conscious effort by someone to destruct his or her own body tissues with out having any intent for suicidality. The most common examples associated with NSSI includes cutting, scratching, burning, banging, self hitting. Mostly the people who self injure themselves are having the history of using two or more methods out of what described before. Because NSSI is frequently connected with emotional and psychiatric discomfort, as well as an increased risk of suicide, correct establishment of conceptual and clinical models of this behavior are critical.
The Non suicidal Self Injury is most commonly seen in young adults and adolescents age groups of around 13-14 years with a lifetime rates of 15-20%. But when the stats studied adult population the rate is 6%. Psychiatric groups, particularly those who report features linked with emotional distress, such as negative emotionality, depression, anxiety, and emotion dysregulation, have the highest incidence of NSSI in both adolescents and adult age group. In addition People who are prone to self-directed negative emotions and self-criticism are more likely to develop NSSI. Although it is typical for people to believe that NSSI is more common in women, general population surveys show that men and women have similar rates. However the sex difference makes the contribution when its comes to the point of methods used for NSSI. The women's are more found to be using cutting whereas the men's more often use the method of hitting and burning.
Historical Perspective
- In early 1844 Bethlem Royal Hospital asylum made clear distinction between "self injury or disposition to suicide"[1][2][3]
- In 20th century, Karl Menninger was the first to decribe self harm as a clinical entity.
- In 1871, G. Fielding Blandford, MD, differentiated between, "will harm or mutilate portion of their bodies" and those who "attempt in every manner to put an end to themselves". He defined self mutilations as nail biting, face or hand picking, and hair plucking are common in nervous people.
- In 1896, George Gould and Walter Pyle, divided self mutilation cases into those committed:
In a period of temporary insanity from melancholia or hallucinations
With suicidal purpose, and
In a religious frenzy or passion.
- In 1883, 1892 James Adam distinguished between self injury with and without psychotic symptoms.
- In 1878, Walter Channing, published a case report of Helen Miller, who was possessed with urges to cut. She resided in an asylum and cut repetitively for 3 years.[4]
Classification

The Non Suicidal Self Injury also known as Self-harm, Self Injury, Self-inflicted violence, Self Injurious Behavior. [5] These are the common term used interchangeably by various authors and practioners to name the disease. The behavior entails intentional tissue injury that is usually carried out without a suicidal motive. Cutting the skin with a sharp item, such as a knife or razor blade, is the most prevalent type of self-harm. The word "self-mutilation" is also occasionally used, albeit it has connotations that some people find alarming, inaccurate, or unpleasant.
Soldiers use the term "self-inflicted wounds" to describe non-lethal injuries they cause in order to be released from combat sooner. But this damage is inflicted for a defined secondary aim, which differs from the standard definition of self-harm. We can also say the people who injure their bodies through disordered eating may be included in the definition of self-harm when broader aspect of the disease is considered.
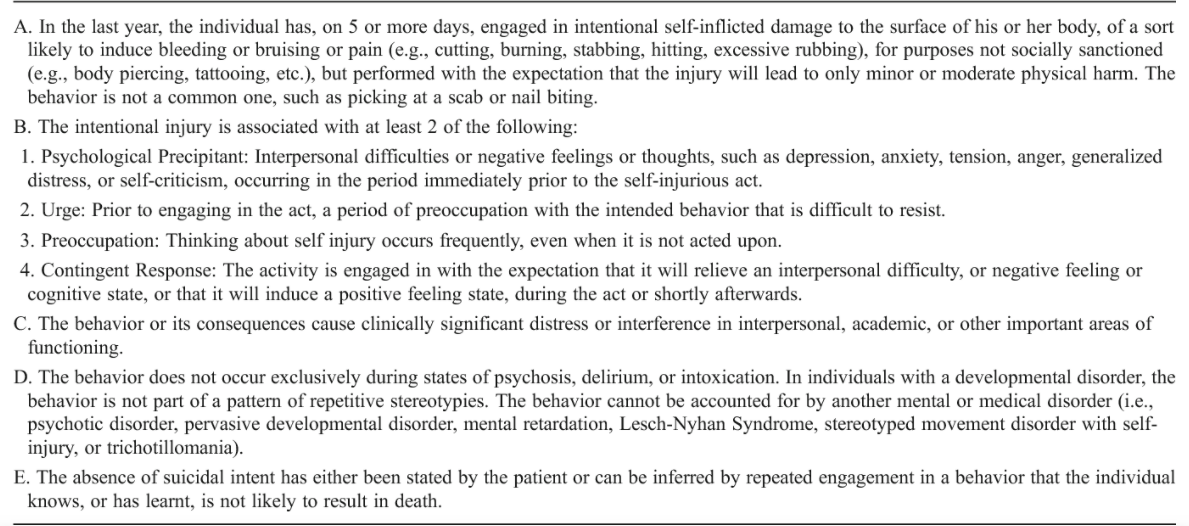
NSSI has been proposed as a disorder in the DSM-5's "Conditions for Further Study" category. It should be noted that this proposed diagnostic criteria for a future diagnosis is not an officially approved diagnosis and should not be utilized in clinical practice; rather, it is intended solely for research purposes. The NSSI is classified as deliberate self-inflicted harm without the intent to commit suicide. The criteria for diagnosing and identifying NSSI includes 5 or more days of self inflicted harm over the duration of one year without having any intention to commit the suicide and along with that the person must have been having a motivation to relief from the negative state or to achieve a positive state.
Self-harm is commonly misunderstood as an attention-seeking behavior; however, this is not always the case. Many self-harmers are self-conscious about their scars and wounds, and they feel bad about their actions, therefore they go to great measures to hide their actions from others. They try to give the alternate reasoning for their scars or try to hide them with clothing. Self-harmers aren't usually trying to take their own lives; instead, it's thought that they're using it as a coping method to ease emotional anguish or discomfort, or as a way to communicate their distress.
Self-harm is dependent on environmental circumstances such as receiving attention or escaping expectations, according to studies of people with developmental disabilities (such as intellectual disability). Some people suffer from dissociation because they want to feel authentic or fit to society's rules.
Pathophysiology
- Emotional and physical pain activates the same regions of the brain which in some people is the reason for the intolerance of emotional stress. Some of this is attributable to environmental, while others are caused by physiological variations in response. [6][7][8][9][10][11]
- The autonomic nervous system is composed of:
- The sympathetic nervous system- controls arousal and physical activation.
- The parasympathetic nervous system-controls automatic physical activation.
- Self-injuring adolescents exhibit higher physiological response to stress (e.g., skin conductance) than non self-injuring adolescents. Over time this stress response stays same and sometimes it even increases.
- Self-harmers think that self-injury can lead to relief. For some, relief comes largely from psychological factors, whereas for others, it comes through the release of beta endorphins in the brain. Endorphins are endogenous opioids that are released in reaction to physical damage, functioning as natural analgesics and producing pleasurable sensations, and would also be released in response to self-harm, reducing tension and mental anguish. Self-harm may become psychologically addictive as a coping technique because it allows the self harmers to deal with extreme anxiety, stress, depression, emotional numbness, and a sense of self-loathing or failure. in the present moment. Its patterns, such as particular time intervals between acts of self-harm, can also result in a behavioural pattern that leads to a desire or urge to act on self-harming ideas.
- Many persons who self-harm claim that it permits them to "get away" or "dissociate," removing their minds from painful sensations. This can be accomplished by convincing the mind that the current suffering is due to the self-harm rather than the difficulties they were dealing with previously: the physical pain serves as a diversion from the initial mental agony.To add to this notion, one can think how important it is to "stop" feeling emotional anguish and mental irritation. "A person may be hypersensitive and overloaded, with a plethora of thoughts whirling about in their heads, and they may get triggered or may decide to stop the overpowering sensations."
- Alternatively, self-harm, on the other hand, might be a way of feeling something, even if it's unpleasant and painful. Anhedonia is a sense of emptiness or numbness experienced by those who self-harm, and physical pain may provide relief from these feelings. "A person might be aloof from oneself, aloof from life, numb and unfeeling."They develop a desire to feel something, and try to create a sesation and "wake up".
Causes
Self-injury is a complicated condition without any simple explanation. Most people use it as a coping mechanism to deal with the feelings of unreality or numbness, to express distressful emotions, to punish themselves, to stop flashbacks and to relieve tension.[12][13][14][15][16]
Common causes of Non Suicidal Self Injury
- Psychological factors: Abuse during childhood, troubled relationships with parents or partner, bereavement. Lack of belonging, considering oneself as a burden, feelings of entrapment,defeat, with the onset of pubertal period and sexual activity because of neurodevelopmental vulnerability. Associated with autism spectrum disorders, borderline personality disorder. As an experience of dissociative state and depersonalisation. Unemployment, war and poverty are other contributing factors.
- Mental disorder:The mental illnesses which have an increased associated risk of self-injury are depression, dissociative disorders, borderline personality disorder, autism spectrum disorders, bipolar disorder, conduct disorders and phobias. OCD, PTSD, Schizophrenia, Substance abuse, poor problem-solving skills and impulsivity, Münchausen syndrome. Eating disorders and anxiety disorders.
- Genetics: The rare genetic condition, Lesch–Nyhan syndrome is characterised by self harm which includes biting and head-banging. Genetics is involved in the development of psychological conditions such as anxiety and depression which may contribute to self-injuring behaviour.
- Drugs and alcohol: Self-harm is linked to chronic substance abuse, dependency, and withdrawal.
- Benzodiazepine dependence as well as benzodiazepine withdrawal.
- Alcohol addiction.
- Cannabis use and intentional self-injury.
- Smoking
Differentiating Nonsuicidal self-injury from other Diseases
| Name of the condition | Characteristic features |
|---|---|
| Post-traumatic Stress disorder | Reliving the incident with distressing recollections, flashbacks, dreams, and/or physical and psychological distress, avoidance of events that might trigger experiences or memories of the trauma, and increased arousal. |
| Dissociative disorder | An unintentional escape from reality characterized by separation between identity, thoughts, memory and awareness. |
| Obsessive-compulsive disorder | Obsessions which are repetitive and persistent urges, thoughts or images followed by compulsions which are repetitive behaviors or mental acts that the individual feels driven to perform. |
| Conduct disorder | Deceitfulness and theft, destruction of property, aggression against people and animals, and serious violations of rules. |
| Intermittent explosive disorder | Unable to stop impulses which leads to physical and verbal aggression. These are out of proportion to the provocation, unplanned and cause subjective and psychosocial distress. |
| Substance use disorder | Use of tobacco, alcohol, and/or legal and illegal drugs causes disability, health problems,or failure to meet major responsibilities at work, school or home. Leads to problems with social interactions, impaired control, and risky behaviors. |
| Bulimia | Consuming huge amounts of food while losing control of one's appetite and then attempting to burn off the excess calories in an unhealthy manner. |
| Dissociative identity disorder | The existence of two or more distinct personality states, as well as repeated gaps in recollection of personal information or experiences, characterizes identity disruption. |
Epidemiology and Demographics
- The prevalence of NSSI varies between 7.5 and 46.5 percent in teenagers, rising to 38.9 percent among students and 4–23% among adults. Despite the fact that self-injurious behaviour is a common occurrence, results from different studies differ significantly.[8][20][8][21][22][23][24]
- The beginning of NSSI is most common in early adolescence, between the ages of 12 and 14, however NSSI behavior has also been seen in children under the age of 12.
- Self-cutting is the most prevalent method, followed by burning, head banging, hitting, and sctratching. Most people who engage in NSSI, use a combination of methods to affect their wrists, arms, stomach and legs.
- The findings of several research studies showed that women exhibited more NSSI behaviors than men.
- Self-cutting is the most prevalent way among women, who are more prone than males to participate in NSSI methods that typically entail blood, whereas burning, hitting and banging are the most common means among men. Among college students, adolescents and adults equal incidence of NSSI has been reported.
- No differences in the race have been seen in the university and adolescent population.
- Multiracial college students have the highest incidence rates in the ethnically varied sample, followed by Caucasian (16.8), and Hispanic (17%). Prevalence rates in Chinese students for NSSI is in the range of 24.9-29.2%. In the Turkish adolescent group it is 21.4%.
Risk Factors
The common risk factors involved in Non Suicidal Self Injury are as follows:[25][17]
- Hopelessness
- Prior history of nonsuicidal self-injury
- Cluster B personality disorders: antisocial personality disorders, histrionic, Borderline, narcissistic.
- Psychopathology
- Emotional/internalizing problems (eg, depressed affect,negative attributional and style social withdrawal)
- Depression
- Behavioral/externalizing problems (eg, aggression, substance use and delinquent behaviors)
- Disordered eating
- Distress
- Affect dysregulation
- Sleep problems
- Impulsivity assessed by self-report (rather than laboratory testing)
- Impaired family functioning
- Self-reported likelihood of engaging in future nonsuicidal self-injury
- Prior suicidal thoughts and/or behaviors
- Other negative life events or stressors, including bullying and peer victimization
- History of childhood maltreatment
- Exposure to peer’s nonsuicidal self-injury
- Parental psychopathology
Screening
The screening for Non Suicidal Self Injury is done by using the The Functional Assessment of Self-Mutilation (FASM). It gives us an assessment if the person was involved in self harming behaviour in the past one year. The person answers a set of questionnaire in terms of yes, no, how many times if its a positive response and if received any treatment.[26][27][28]
- Scraped the skin
- Cut or carve on the skin
- "Erased" the skin
- Gave themselves a tattoo
- Hit oneself on purpose
- Picked at a wound
- Pulled hair out
- Bit themselves (eg, lip or mouth)
- Burned the skin (ie, with a match, cigarette, or other hot object)
- Picked areas of the body to the point of drawing blood
- Inserted objects under the nails or skin
Natural History, Complications, and Prognosis
If left untreated, [#]% of patients with [disease name] may progress to develop [manifestation 1], [manifestation 2], and [manifestation 3].
OR
Common complications of [disease name] include [complication 1], [complication 2], and [complication 3].
OR
Prognosis is generally excellent/good/poor, and the 1/5/10-year mortality/survival rate of patients with [disease name] is approximately [#]%.
Diagnosis
Diagnostic Study of Choice
Most of the people who show self-harming behaviour meet the DSM-5 criteria for Non Suicidal Self Injury.
History and Symptoms
Eighty percent of self-injury includes stabbing or cutting the skin with a sharp tool, sometimes completely piercing the skin. Self-harm is frequently committed in regions of the body that are readily hidden and undetectable to others. Most often it is a symptom of an underlying disorder and these people look for help to get out of this.
Common signs and symptoms that a person may be engaging in self-harm include the following:[29][30]
- Self-poisoning, self-embedding of objects, hair pulling, burning, alcohol abuse, bruising/hitting one's self,
- Fresh cuts, bruises, scratches, bite marks or other wounds.
- Knowingly abusing over the counter or prescription drugs,
- Scars, often in patterns
- Excessive rubbing of an area to create a burn
- Self-harm related to anorexia and bulimia.
- Frequent reports of accidental injury
- Keeping sharp objects close by or on hand
- Wearing long sleeves or long pants, even in hot weather
- Statements of helplessness, worthlessness or hopelessness
- Emotional and behavioral instability, unpredictability and impulsivity
- Difficulties in interpersonal relationships
Physical Examination
During physical examination special attention must be given to orientation and level of consciousness, vital signs and toxidrome manifestations. In addition to this physicians should check for the following: [31]
- Remote or recent suicide attempts (eg, bruises from hanging or scars from cutting)
- Sexual or physical abuse (eg, genital trauma or characteristic bruising patterns)
- Substance abuse (eg, perioral blisters or nosebleeds from inhalant use or track marks from intravenous drug use)
- General medical illness (eg, thyroid disease)
Laboratory Findings
The laboratory evaluation of a suicidal child or adolescent should be tailored to the circumstances of the ideation or attempt, as well as the clinical risk assessment for illicit drug use and complicating medical issues, such as pregnancy and the presence of sexually transmitted diseases.[32] Screening laboratory tests that are often conducted and typically needed by hospitals before they consider patients for admission are.
- Urine toxicology screen for drugs of abuse, acetaminophen and aspirin
- Serum chemistry panels
- Complete blood count
- Thyroid stimulating hormone
- Urinalysis
- Human chorionic gonadotropin (pregnancy) in girls
MRI
Resting state fMRI (rsfMRI or R-fMRI) is a method of functional magnetic resonance imaging (fMRI). When fMRI was done on a patient with NSSI, the findings were:[33]
- atypical amygdala-frontal connectivity
- greater amygdala RSFC in dorsal anterior cingulate and supplementary motor area (SMA)
- differential amygdala-occipital connectivity
Treatment
Short term psychotherapy and pharmacotherapy are effective in decreasing NSSI.[34][35][36][37][38][39][40] It is important to manage comorbid disorders before giving a trial of medications for self injury. Always those interventions are tried first which have greater evidence based effectiveness
| Type of Psychotherapy | Description |
|---|---|
| Dialectical behavioral therapy (DBT) | It's a combination of individual and group therapy, as well as a therapist consultation team. DBT causes larger decreases in NSSI and SSI, which last for 6 to 12 months following therapy. DBT lowers the frequency, rate, and desire to participate in NSSI. |
| Emotion Regulation Group Therapy (ERGT) | ERGT is a 14-week group therapy program that focuses on developing emotion control and acceptance skills, as well as identifying and pursuing significant objectives and values. In comparison to treatment as usual (TAU) , there were considerably larger decreases in NSSI frequency. Studies involving a follow up period indicated that therapy effects are long-lasting. |
| Manual-assisted cognitive-behaviour therapy (MACT) | MACT is a systematic, problem-solving treatment that includes individual counseling and bibliotherapy and is generally completed in six sessions. MACT has a substantial benefit over TAU (treatment as usaul) in lowering the frequency of NSSI in female adults with BPD. |
| Transference–Focused Therapy(TPF) | TFP is a psychodynamic therapy that involves twice-weekly individual sessions that use relationship transference for therapeutic change. TFP for females with BPD found substantial decreases in severity from pre- to posttreatment. |
| Dyadic developmental psychotherapy (DDP) | DDP is a manualized psychodynamic therapy that employs weekly individual sessions for BPD patients with difficult co-occurring disorders to help hem explain affective and interpersonal experiences in coherent narratives. The frequency of NSSI in the last three months of DDP therapy was considerably lower than before the treatment. |
| Voice movement therapy (VMT) | VMT is an and expressive arts therapy that integrates sound-making, expressive writing, singing, movement, massage, and drama activities to minimize emotion dysregulation and enhance self-awareness. When compared to the 10-week pretreatment period, young females engaged in less frequent NSSI while receiving 10 weeks of VMT. |
- Pharmacotherapy for Nonsuicidal Self-Injury: There are 5 classes of drugs which are effective for NSSI treatment:
- SSRIs (for example, fluoxetine)
- Atypical antipsychotics
- SNRIs (venlafaxine),
- Opioids (buprenorphine), and
- Opioid antagonists (naltrexone).
- Treatment of adults with BPD with SSRI, demonstrated abstinence from NSSI during the treatment and the 18-month follow up period. Atypical antipsychotics (such as aripiprazole and ziprasidone) resulted in reduction in rates and frequency of NSSI among self-injuring teenagers.
- Nonantipsychotics treatment in adults with BPD resulted in decrease in the rates and frequency of NSSI significantly compared with the baseline. There has been reported benefits of fluoxetine, venlafaxine, naltrexone and buprenorphine in increasing the rates of NSSI abstinence and (or) in reducing NSSI frequency.
- Combination Treatments for Nonsuicidal Self-Injury
- There has been a reporting of benefits of combing CBT and antidepressants together in the treatment of major depressive disorder in adolescents
- Comprehensive Therapeutic Programs for Nonsuicidal Self-Injury
- The effectiveness of comprehensive treatment programs for people with BPD or mixed personality disorders can be seen as a significant decreases in NSSI rates after intervention. These customized programs comprised pharmacotherapy, psychoeducation, group and individual therapy incorporated with DBT skills training as part of treatment.
- Other Interventions for Nonsuicidal Self-Injury
- Following purposeful self-poisoning, a structured postcard intervention dramatically decreased suicide-related consequences.
- Patients attending assertiveness training classes biweekly led by a psychiatrist improved their self-acceptance and capacity to calmly communicate their needs and desires.
- Auricular acupuncture was linked to a substantial reduction in the incidence of NSSI in depressed adolescents.
References
- ↑ "Chaney | Anaesthetic Bodies and the Absence of Feeling: Pain and Self-Mutilation in Later Nineteenth-Century Psychiatry | 19: Interdisciplinary Studies in the Long Nineteenth Century".
- ↑ "core.ac.uk" (PDF).
- ↑ Vahia VN (July 2013). "Diagnostic and statistical manual of mental disorders 5: A quick glance". Indian J Psychiatry. 55 (3): 220–3. doi:10.4103/0019-5545.117131. PMC 3777342. PMID 24082241.
- ↑ "Case of Helen Miller: self-mutilaton, tracheotomy - Digital Collections - National Library of Medicine".
- ↑ "APA PsycNet".
- ↑ Ballard E, Bosk A, Pao M (April 2010). "Invited commentary: understanding brain mechanisms of pain processing in adolescents' non-suicidal self-injury". J Youth Adolesc. 39 (4): 327–34. doi:10.1007/s10964-009-9457-1. PMID 19830534.
- ↑ Bohus M, Limberger M, Ebner U, Glocker FX, Schwarz B, Wernz M, Lieb K (September 2000). "Pain perception during self-reported distress and calmness in patients with borderline personality disorder and self-mutilating behavior". Psychiatry Res. 95 (3): 251–60. doi:10.1016/s0165-1781(00)00179-7. PMID 10974364.
- ↑ 8.0 8.1 8.2 Briere J, Gil E (October 1998). "Self-mutilation in clinical and general population samples: prevalence, correlates, and functions". Am J Orthopsychiatry. 68 (4): 609–20. doi:10.1037/h0080369. PMID 9809120.
- ↑ Deliberto TL, Nock MK (2008). "An exploratory study of correlates, onset, and offset of non-suicidal self-injury". Arch Suicide Res. 12 (3): 219–31. doi:10.1080/13811110802101096. PMID 18576203.
- ↑ Eisenberger NI, Jarcho JM, Lieberman MD, Naliboff BD (December 2006). "An experimental study of shared sensitivity to physical pain and social rejection". Pain. 126 (1–3): 132–8. doi:10.1016/j.pain.2006.06.024. PMID 16890354.
- ↑ Eisenberger NI, Lieberman MD (July 2004). "Why rejection hurts: a common neural alarm system for physical and social pain". Trends Cogn Sci. 8 (7): 294–300. doi:10.1016/j.tics.2004.05.010. PMID 15242688.
- ↑ Joyce PR, Light KJ, Rowe SL, Cloninger CR, Kennedy MA (March 2010). "Self-mutilation and suicide attempts: relationships to bipolar disorder, borderline personality disorder, temperament and character". Aust N Z J Psychiatry. 44 (3): 250–7. doi:10.3109/00048670903487159. PMID 20180727.
- ↑ Rossow I, Hawton K, Ystgaard M (2009). "Cannabis use and deliberate self-harm in adolescence: a comparative analysis of associations in England and Norway". Arch Suicide Res. 13 (4): 340–8. doi:10.1080/13811110903266475. PMID 19813111.
- ↑ Urnes O (April 2009). "[Self-harm and personality disorders]". Tidsskr Nor Laegeforen (in Norwegian). 129 (9): 872–6. doi:10.4045/tidsskr.08.0140. PMID 19415088.
- ↑ Humphries SR (March 1988). "Munchausen syndrome. Motives and the relation to deliberate self-harm". Br J Psychiatry. 152: 416–7. doi:10.1192/bjp.152.3.416. PMID 3167380.
- ↑ Johnson CP, Myers SM (November 2007). "Identification and evaluation of children with autism spectrum disorders". Pediatrics. 120 (5): 1183–215. doi:10.1542/peds.2007-2361. PMID 17967920.
- ↑ 17.0 17.1 "Redirecting".
- ↑ "DSM-5".
- ↑ Foa EB, Kozak MJ, Goodman WK, Hollander E, Jenike MA, Rasmussen SA (January 1995). "DSM-IV field trial: obsessive-compulsive disorder". Am J Psychiatry. 152 (1): 90–6. doi:10.1176/ajp.152.1.90. PMID 7802127.
- ↑ Archer S, Zayed AH, Rej R, Rugino TA (September 1983). "Analogues of hycanthone and lucanthone as antitumor agents". J Med Chem. 26 (9): 1240–6. doi:10.1021/jm00363a007. PMID 6887199.
- ↑ Muehlenkamp JJ, Gutierrez PM (2007). "Risk for suicide attempts among adolescents who engage in non-suicidal self-injury". Arch Suicide Res. 11 (1): 69–82. doi:10.1080/13811110600992902. PMID 17178643.
- ↑ Sornberger MJ, Heath NL, Toste JR, McLouth R (June 2012). "Nonsuicidal self-injury and gender: patterns of prevalence, methods, and locations among adolescents". Suicide Life Threat Behav. 42 (3): 266–78. doi:10.1111/j.1943-278X.2012.0088.x. PMID 22435988.
- ↑ Kuentzel JG, Arble E, Boutros N, Chugani D, Barnett D (July 2012). "Nonsuicidal self-injury in an ethnically diverse college sample". Am J Orthopsychiatry. 82 (3): 291–7. doi:10.1111/j.1939-0025.2012.01167.x. PMID 22880967.
- ↑ Wan Y, Chen J, Sun Y, Tao F (2015). "Impact of Childhood Abuse on the Risk of Non-Suicidal Self-Injury in Mainland Chinese Adolescents". PLoS One. 10 (6): e0131239. doi:10.1371/journal.pone.0131239. PMC 4482708. PMID 26114574.
- ↑ Fox KR, Franklin JC, Ribeiro JD, Kleiman EM, Bentley KH, Nock MK (December 2015). "Meta-analysis of risk factors for nonsuicidal self-injury". Clin Psychol Rev. 42: 156–67. doi:10.1016/j.cpr.2015.09.002. PMC 4772426. PMID 26416295.
- ↑ Izadi-Mazidi M, Yaghubi H, Mohammadkhani P, Hassanabadi H (July 2019). "Assessing the Functions of Non-Suicidal Self-Injury: Factor Analysis of Functional Assessment of Self-Mutilation among Adolescents". Iran J Psychiatry. 14 (3): 184–191. PMC 6778602 Check
|pmc=value (help). PMID 31598120. - ↑ Calvete E, Orue I, Aizpuru L, Brotherton H (2015). "Prevalence and functions of non-suicidal self-injury in Spanish adolescents". Psicothema. 27 (3): 223–8. doi:10.7334/psicothema2014.262. PMID 26260928.
- ↑ Leong CH, Wu AM, Poon MM (2014). "Measurement of perceived functions of non-suicidal self-injury for Chinese adolescents". Arch Suicide Res. 18 (2): 193–212. doi:10.1080/13811118.2013.824828. PMID 24568552.
- ↑ Greydanus DE, Shek D (September 2009). "Deliberate self-harm and suicide in adolescents". Keio J Med. 58 (3): 144–51. doi:10.2302/kjm.58.144. PMID 19826208.
- ↑ [+https://doi.org/10.1111/j.1475-682X.2004.00085.x "Cutting through the Silence: A Sociological Construction of Self‐Injury - Hodgson - 2004 - Sociological Inquiry - Wiley Online Library"] Check
|url=value (help). - ↑ Burke TA, Hamilton JL, Cohen JN, Stange JP, Alloy LB (February 2016). "Identifying a physical indicator of suicide risk: Non-suicidal self-injury scars predict suicidal ideation and suicide attempts". Compr Psychiatry. 65: 79–87. doi:10.1016/j.comppsych.2015.10.008. PMC 4715861. PMID 26773994.
- ↑ "Assessing Non-Suicidal Self-Injury in the Laboratory: Archives of Suicide Research: Vol 22, No 2".
- ↑ Westlund Schreiner M, Klimes-Dougan B, Mueller BA, Eberly LE, Reigstad KM, Carstedt PA, Thomas KM, Hunt RH, Lim KO, Cullen KR (October 2017). "Multi-modal neuroimaging of adolescents with non-suicidal self-injury: Amygdala functional connectivity". J Affect Disord. 221: 47–55. doi:10.1016/j.jad.2017.06.004. PMC 5555154. PMID 28628767.
- ↑ Hawton K, Witt KG, Taylor Salisbury TL, Arensman E, Gunnell D, Hazell P, Townsend E, van Heeringen K (July 2015). "Pharmacological interventions for self-harm in adults". Cochrane Database Syst Rev (7): CD011777. doi:10.1002/14651858.CD011777. PMID 26147958.
- ↑ Stoffers J, Völlm BA, Rücker G, Timmer A, Huband N, Lieb K (June 2010). "Pharmacological interventions for borderline personality disorder". Cochrane Database Syst Rev (6): CD005653. doi:10.1002/14651858.CD005653.pub2. PMC 4169794. PMID 20556762.
- ↑ Ougrin D, Tranah T, Stahl D, Moran P, Asarnow JR (February 2015). "Therapeutic interventions for suicide attempts and self-harm in adolescents: systematic review and meta-analysis". J Am Acad Child Adolesc Psychiatry. 54 (2): 97–107.e2. doi:10.1016/j.jaac.2014.10.009. PMID 25617250.
- ↑ Brent DA, Emslie GJ, Clarke GN, Asarnow J, Spirito A, Ritz L, Vitiello B, Iyengar S, Birmaher B, Ryan ND, Zelazny J, Onorato M, Kennard B, Mayes TL, Debar LL, McCracken JT, Strober M, Suddath R, Leonard H, Porta G, Keller MB (April 2009). "Predictors of spontaneous and systematically assessed suicidal adverse events in the treatment of SSRI-resistant depression in adolescents (TORDIA) study". Am J Psychiatry. 166 (4): 418–26. doi:10.1176/appi.ajp.2008.08070976. PMC 3593721. PMID 19223438.
- ↑ Taylor LM, Oldershaw A, Richards C, Davidson K, Schmidt U, Simic M (October 2011). "Development and pilot evaluation of a manualized cognitive-behavioural treatment package for adolescent self-harm". Behav Cogn Psychother. 39 (5): 619–25. doi:10.1017/S1352465811000075. PMID 21392417.
- ↑ Hawton K, Witt KG, Taylor Salisbury TL, Arensman E, Gunnell D, Hazell P, Townsend E, van Heeringen K (May 2016). "Psychosocial interventions for self-harm in adults". Cochrane Database Syst Rev (5): CD012189. doi:10.1002/14651858.CD012189. PMID 27168519.
- ↑ Fischer G, Brunner R, Parzer P, Resch F, Kaess M (September 2013). "Short-term psychotherapeutic treatment in adolescents engaging in non-suicidal self-injury: a randomized controlled trial". Trials. 14: 294. doi:10.1186/1745-6215-14-294. PMC 3848593. PMID 24034810.