Sandbox:Hamid: Difference between revisions
Hamid Qazi (talk | contribs) No edit summary |
Hamid Qazi (talk | contribs) |
||
| (87 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{Infobox_Disease | |||
| Name = {{PAGENAME}} | |||
| Image = | |||
| Caption = | |||
| DiseasesDB = 23647 | |||
| ICD10 = {{ICD10|K|42||k|40}} | |||
| ICD9 = {{ICD9|551}}-{{ICD9|553}} | |||
| ICDO = | |||
| OMIM = | |||
| MedlinePlus = 000987 | |||
| eMedicineSubj = | |||
| eMedicineTopic = | |||
| MeshID = D006554 | |||
}} | |||
{{HQ}} | |||
Salm.. | |||
==Historical Perspective== [1] | |||
===Discovery=== | |||
*Salmonella was first discovered by Daniel E. Salmon, an American veterinarian, who first isolated Salmonella choleraesuis from pigs in 1884 with hog cholera. | |||
*The association between [important risk factor/cause] and [disease name] was made in/during [year/event]. | |||
*In [year], [scientist] was the first to discover the association between [risk factor] and the development of [disease name]. | |||
*In [year], [gene] mutations were first implicated in the pathogenesis of [disease name]. | |||
==Outbreaks== | |||
*There have been several outbreaks of [disease name], which are summarized below: | |||
==Landmark Events in the Development of Treatment Strategies== | |||
*In [year], [diagnostic test/therapy] was developed by [scientist] to treat/diagnose [disease name]. | |||
==Impact on Cultural History== | |||
==Famous Cases== | |||
*The following are a few famous cases of [[disease name]]: | |||
==Classification== | |||
*[Disease name] may be classified according to Kaufmann-White typing system into [number] subtypes: | |||
**Somatic O | |||
**Surface Vi | |||
**Flagellar H antigens | |||
==Pathophysiology== | |||
After ingestion, infection with salmonellae is characterized by attachment of the bacteria by fimbriae or pili to cells lining the intestinal lumen. Salmonellae selectively attach to specialized epithelial cells (M cells) of the Peyer patches. The bacteria are then internalized by receptor-mediated endocytosis and transported within phagosomes to the lamina propria, where they are released. Once there, salmonellae induce an influx of macrophages (typhoidal strains) or neutrophils (nontyphoidal strains). | |||
The Vi antigen of S typhi is important in preventing antibody-mediated opsonization and complement-mediated lysis. Through the induction of cytokine release and via mononuclear cell migration, S typhi organisms spread through the reticuloendothelial system, mainly to the liver, spleen, and bone marrow. Within 14 days, the bacteria appear in the bloodstream, facilitating secondary metastatic foci (eg, splenic abscess, endocarditis). In some patients, gallbladder infection leads to long-term carriage of S typhi or S paratyphi in bile and secretion to the stool. [17] As a rule, infection with nontyphoidal salmonellae generally precipitates a localized response, while S typhi and other especially virulent strains invade deeper tissues via lymphatics and capillaries and elicit a major immune response. | |||
===Pathogenesis=== | |||
*It is understood that [disease name] is the result of / is mediated by / is produced by / is caused by either [hypothesis 1], [hypothesis 2], or [hypothesis 3]. | |||
*[Pathogen name] is usually transmitted via the [transmission route] route to the human host. | |||
*Following ingestion, salmonella uses the [entry site] to invade the [cell name] cell. | |||
*[Disease or malignancy name] arises from [cell name]s, which are [cell type] cells that are normally involved in [function of cells]. | |||
*The progression to [disease name] usually involves the [molecular pathway]. | |||
*The pathophysiology of [disease/malignancy] depends on the histological subtype. | |||
==Genetics== | |||
*[Disease name] is transmitted in [mode of genetic transmission] pattern. | |||
*Genes involved in the pathogenesis of [disease name] include [gene1], [gene2], and [gene3]. | |||
*The development of [disease name] is the result of multiple genetic mutations. | |||
==Associated Conditions== | |||
==Gross Pathology== | |||
*On gross pathology, [feature1], [feature2], and [feature3] are characteristic findings of [disease name]. | |||
==Microscopic Pathology== | |||
*On microscopic histopathological analysis, [feature1], [feature2], and [feature3] are characteristic findings of [disease name]. | |||
==Overview== | ==Overview== | ||
<figure-inline><figure-inline><figure-inline>[[File:Peutz-Jeghers syndrome polyp.jpg|899x899px]]</figure-inline></figure-inline></figure-inline> | |||
==Historical Perspective== | |||
===Discovery===<ref name="KopacovaTacheci2009">{{cite journal|last1=Kopacova|first1=Marcela|last2=Tacheci|first2=Ilja|last3=Rejchrt|first3=Stanislav|last4=Bures|first4=Jan|title=Peutz-Jeghers syndrome: Diagnostic and therapeuticapproach|journal=World Journal of Gastroenterology|volume=15|issue=43|year=2009|pages=5397|issn=1007-9327|doi=10.3748/wjg.15.5397}}</ref><ref name="GiardielloTrimbath2006">{{cite journal|last1=Giardiello|first1=F|last2=Trimbath|first2=J|title=Peutz-Jeghers Syndrome and Management Recommendations|journal=Clinical Gastroenterology and Hepatology|volume=4|issue=4|year=2006|pages=408–415|issn=15423565|doi=10.1016/j.cgh.2005.11.005}}</ref> | |||
*Peutz-Jeghers syndrome was first discovered by Dr. Connor, a British, in 1895 in identical twin sisters. | |||
*The association between gastrointestinal polyposis with distinctive pigmentation of the skin and Peutz-Jeghers syndrome was made in 1921 by Dr. Johannes Peutz of Holland. | |||
*In 1949, Dr. Harold Jeghers of United States was the first to discover the association between combination of intestinal polyposis and skin pigmentation, and the development of Peutz-Jeghers syndrome. | |||
*In 1954, A. Bruwer used the eponym Peutz-Jeghers syndrome | |||
*In 1998, serine/threonine-protein kinase 11 alias LKB1 (STK11/LKB1) gene mutations were first implicated in the pathogenesis of Peutz-Jeghers syndrome. | |||
==Classification== | |||
*There is no established system for the classification of Peutz-Jeghers syndrome. | |||
==Pathophysiology== | |||
===Pathogenesis=== | |||
*It is thought that Peutz-Jeghers syndrome is the result of deletion or partial deletion of STK11 (LBK1) gene, located on chromosome 19p13.3.<ref name="KopacovaTacheci2009">{{cite journal|last1=Kopacova|first1=Marcela|last2=Tacheci|first2=Ilja|last3=Rejchrt|first3=Stanislav|last4=Bures|first4=Jan|title=Peutz-Jeghers syndrome: Diagnostic and therapeuticapproach|journal=World Journal of Gastroenterology|volume=15|issue=43|year=2009|pages=5397|issn=1007-9327|doi=10.3748/wjg.15.5397}}</ref> | |||
*STK11 protein plays an important role in second messenger signal transduction and is found to regulate cellular proliferation, controls cell polarity, and responds to low energy states. | |||
*In Mammalian studies, STK11 is shown in the inhibition of AMP-activated protein kinase (AMPK), and signals downstream to inhibit the mammalian target of rapamycin (mTOR).<ref name="KopacovaTacheci2009">{{cite journal|last1=Kopacova|first1=Marcela|last2=Tacheci|first2=Ilja|last3=Rejchrt|first3=Stanislav|last4=Bures|first4=Jan|title=Peutz-Jeghers syndrome: Diagnostic and therapeuticapproach|journal=World Journal of Gastroenterology|volume=15|issue=43|year=2009|pages=5397|issn=1007-9327|doi=10.3748/wjg.15.5397}}</ref> | |||
**The mTOR pathway is dysregulated in Peutz-Jeghers syndrome. | |||
===Pathology=== | |||
*Peutz-Jeghers syndrome associated polyps have a unique smooth muscle core that arborizes throughout the polyp.<ref name="KopacovaTacheci2009">{{cite journal|last1=Kopacova|first1=Marcela|last2=Tacheci|first2=Ilja|last3=Rejchrt|first3=Stanislav|last4=Bures|first4=Jan|title=Peutz-Jeghers syndrome: Diagnostic and therapeuticapproach|journal=World Journal of Gastroenterology|volume=15|issue=43|year=2009|pages=5397|issn=1007-9327|doi=10.3748/wjg.15.5397}}</ref> | |||
**These polyps can only be differentiated from other polyp types by histopathology. | |||
===Causes=== | |||
*Peutz-Jeghers syndrome is caused by STK11 gene mutation | |||
*Variable penetrance | |||
* | |||
==Epidemiology and Demographics== | ==Epidemiology and Demographics== | ||
=== | ===Prevalence=== | ||
*The | *The prevalence of Peutz-Jeghers syndrome is estimated to be 1 in 8300 to 250000 | ||
* | *Most likely prevalence is 1 in 100000 | ||
===Age=== | |||
*Peutz-Jeghers syndrome affects individuals between the ages of 10 to 30 years; average age of diagnosis is 23 years for males and 26 years for females. | |||
===Gender=== | |||
*Males and females are equally affected. | |||
==Risk Factors== | |||
*There are no established risk factors for Peutz-Jeghers | |||
==Screening== | |||
*According to the American College of Gastroenterology (ACG) and the National Comprehensive Cancer Network (NCCN), screening for Peutz-Jeghers syndrome by physical exam, complete blood work for iron deficiency anemia, and endoscopy are recommended every year among patients with Peutz-Jeghers Syndrome. | |||
==Natural History, Complications, and Prognosis== | |||
===Natural History=== | |||
*The symptoms of Peutz-Jeghers syndrome usually develop in the first decade of life, and start with symptoms such as hyperpigmentation, abdominal pain, and rectal bleeding. | |||
*If left untreated, patients with Peutz-Jeghers syndrome may progress to develop colon cancer, breast cancer, and gastrointestinal cancers. | |||
*Extraintestinal manifestation include pancreatic, lung, breast, uterine, ovarian and testicular malignancies. | |||
===Complications=== | |||
*Common complications of Peutz-Jeghers syndrome include: | |||
**Intussusception | |||
**Gastric outlet obstruction | |||
**Extraintestinal polyps | |||
=== | ===Prognosis=== | ||
* | *Prognosis is generally excellent/good/poor, and the 1/5/10-year mortality/survival rate of patients with [disease name] is approximately [#]%. | ||
* | *Depending on the extent of the [tumor/disease progression/etc.] at the time of diagnosis, the prognosis may vary. However, the prognosis is generally regarded as poor/good/excellent. | ||
*The | *The presence of [characteristic of disease] is associated with a particularly [good/poor] prognosis among patients with [disease/malignancy]. | ||
*[Subtype of disease/malignancy] is associated with the most favorable prognosis. | |||
*The prognosis varies with the [characteristic] of tumor; [subtype of disease/malignancy] have the most favorable prognosis. | |||
===Signs and Symptoms Differential compared to Peutz-Jeghers Syndrome=== | |||
{{cite web |url=https://www.ncbi.nlm.nih.gov/books/NBK1266/#pjs.Diagnosis |title=Peutz-Jeghers Syndrome - GeneReviews® - NCBI Bookshelf |format= |work= |accessdate=}} | |||
{| | |||
|- style="background: #4479BA; color: #FFFFFF; text-align: center;" | |||
! rowspan="2" |Diseases | |||
! colspan="4" |History and Symptoms | |||
! colspan="4" |Physical Examination | |||
! colspan="4" |Laboratory Findings | |||
! rowspan="2" |Other Findings | |||
|- style="background: #4479BA; color: #FFFFFF; text-align: center;" | |||
!Abdominal Pain | |||
!Rectal Bleeding | |||
!Hyperpigmentation | |||
!Fatigue | |||
!Abdominal Pain | |||
!Hyperpigmentation | |||
!Anemia | |||
!Physical Finding 4 | |||
!Gene(s) | |||
!Sertoli Cell Tumors | |||
!Gastrointestinal Tumors | |||
!Cancers | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |Juvenile Polyposis Syndrome | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" |SMAD4 | |||
BMPR1A | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" |Adenoma+ | |||
Hamartoma+++ | |||
| style="background: #F5F5F5; padding: 5px;" |Colon | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |Cowden Syndrome | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" |Axillary+ | |||
Inguinal+ | |||
Facial+ | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" |Axillary+ | |||
Inguinal+ | |||
Facial+ | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" |PTEN | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" |Adenoma+ | |||
Hamartoma+++ | |||
| style="background: #F5F5F5; padding: 5px;" |Breast, Thyroid, Endometrium | |||
| style="background: #F5F5F5; padding: 5px;" |Trichilemmoma, skin hamartoma, hyperplastic polyps, macrocephaly, breast fibrosis | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |Carney Syndrome | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" |Facial+ | |||
Mucosal+ | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" |Facial+ | |||
Mucosal+ | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" |PRKAR1A | |||
| style="background: #F5F5F5; padding: 5px;" | ++ | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" |Thyroid | |||
| style="background: #F5F5F5; padding: 5px;" |Myxomas of skin and heart | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |Familial Adenomatous Polyposis | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" |APC | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" |Adenoma+++ | |||
| style="background: #F5F5F5; padding: 5px;" |Colon, brain | |||
| style="background: #F5F5F5; padding: 5px;" |Desmoid tumors, osteomas | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |Hereditary Non-Polyposis Colon Cancer | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" |MLH1 | |||
MSH2 | |||
MSH3 | |||
MSH6 | |||
PMS1 | |||
PMS2 | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" |Adenoma+ | |||
| style="background: #F5F5F5; padding: 5px;" |Endometrial, gastric, renal pelvis, ureter, and ovarian | |||
| style="background: #F5F5F5; padding: 5px;" |Sebaceous adenoma | |||
|} | |||
===Use if the above table can not be made=== | |||
{| style="border: 0px; font-size: 90%; margin: 3px; width: 1000px" align="center" | |||
| valign="top" | | |||
|+ | |||
! style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|Differential Diagnosis}} | |||
! style="background: #4479BA; width: 300px;" | {{fontcolor|#FFF|Similar Features}} | |||
! style="background: #4479BA; width: 300px;" | {{fontcolor|#FFF|Differentiating Features}} | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold; text-align:center;" |Juvenile Polyposis Syndrome | |||
| style="padding: 5px 5px; background: #F5F5F5;" | | |||
* On [physical exam; history; diagnostic test; imaging], [Differential 1] {has; demonstrates} [feature 1], [feature 2], [feature 3] also observed in [disease name]. | |||
| style="padding: 5px 5px; background: #F5F5F5;" | | |||
* On [physical exam; history; diagnostic test; imaging], [Differential 1] {has; demonstrates} [feature 1], [feature 2], [feature 3] that distinguish it from [disease name]. | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold; text-align:center;" |Cowden Syndrome | |||
| style="padding: 5px 5px; background: #F5F5F5;" | | |||
* On [physical exam; history; diagnostic test; imaging], [Differential 1] {has; demonstrates} [feature 1], [feature 2], [feature 3] also observed in [disease name]. | |||
| style="padding: 5px 5px; background: #F5F5F5;" | | |||
* On [physical exam; history; diagnostic test; imaging], [Differential 1] {has; demonstrates} [feature 1], [feature 2], [feature 3] that distinguish it from [disease name]. | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold; text-align:center;" |Carney Syndrome | |||
| style="padding: 5px 5px; background: #F5F5F5;" | | |||
* On [physical exam; history; diagnostic test; imaging], [Differential 1] {has; demonstrates} [feature 1], [feature 2], [feature 3] also observed in [disease name]. | |||
| style="padding: 5px 5px; background: #F5F5F5;" | | |||
* On [physical exam; history; diagnostic test; imaging], [Differential 1] {has; demonstrates} [feature 1], [feature 2], [feature 3] that distinguish it from [disease name]. | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold; text-align:center;" |Familial Adenomatous Polyposis | |||
| style="padding: 5px 5px; background: #F5F5F5;" | | |||
* On [physical exam; history; diagnostic test; imaging], [Differential 1] {has; demonstrates} [feature 1], [feature 2], [feature 3] also observed in [disease name]. | |||
| style="padding: 5px 5px; background: #F5F5F5;" | | |||
* On [physical exam; history; diagnostic test; imaging], [Differential 1] {has; demonstrates} [feature 1], [feature 2], [feature 3] that distinguish it from [disease name]. | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold; text-align:center;" |Hereditary Non-Polyposis Colon Cancer | |||
| style="padding: 5px 5px; background: #F5F5F5;" | | |||
* On [physical exam; history; diagnostic test; imaging], [Differential 1] {has; demonstrates} [feature 1], [feature 2], [feature 3] also observed in [disease name]. | |||
| style="padding: 5px 5px; background: #F5F5F5;" | | |||
* On [physical exam; history; diagnostic test; imaging], [Differential 1] {has; demonstrates} [feature 1], [feature 2], [feature 3] that distinguish it from [disease name]. | |||
|} | |||
==Differentiating Gastrointestinal Bleeding from other Diseases== | |||
{| align="center" | |||
|- | |||
| | |||
{| style="border: 0px; font-size: 90%; margin: 3px;" align="center" | |||
! rowspan="3" style="background:#4479BA; color: #FFFFFF;" align="center" |Disease | |||
| colspan="13" rowspan="1" style="background:#4479BA; color: #FFFFFF;" align="center" |'''Clinical manifestations''' | |||
! colspan="2" rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Diagnosis | |||
! rowspan="3" style="background:#4479BA; color: #FFFFFF;" align="center" |Comments | |||
|- | |||
| colspan="9" rowspan="1" style="background:#4479BA; color: #FFFFFF;" align="center" |'''Symptoms''' | |||
! colspan="4" rowspan="1" style="background:#4479BA; color: #FFFFFF;" align="center" | Signs | |||
|- | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Abdominal Pain | |||
! colspan="1" rowspan="1" style="background:#4479BA; color: #FFFFFF;" align="center" | Fever | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Rigors and chills | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Nausea or vomiting | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Jaundice | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Constipation | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Diarrhea | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Weight loss | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |GI bleeding | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Hypo- | |||
tension | |||
! colspan="1" rowspan="1" style="background:#4479BA; color: #FFFFFF;" align="center" | Guarding | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Rebound Tenderness | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Bowel sounds | |||
! colspan="1" rowspan="1" style="background:#4479BA; color: #FFFFFF;" align="center" | Lab Findings | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Imaging | |||
|- | |||
| colspan="1" rowspan="1" style="padding: 5px 5px; background: #DCDCDC;" align="center" |Peutz-Jeghers syndrome | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |Depends on location of polyps it maybe present | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center"| ± | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center"| - | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center"| ± | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center"| - | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center"| ± | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center"| ± | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center"| ± | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center"| | |||
* Rectal bleeding may be present due to polyp | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center"| - | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center"| - | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center"| - | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center"| + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center"| | |||
* Hamartomatous polyps present on endoscopy | |||
* Iron deficiency anemia on CBC | |||
* STK11 mutation | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center"| | |||
* Intra-operative enteroscopy (laparatomy with endoscopy | |||
* Double balloon eneteroscopy | |||
* Colonoscopy | |||
* Barium Swallow | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center"| | |||
* Can lead to colon cancer, breast cancer, ovarian cancer, cervical cancer, and testicular cancer | |||
|- | |||
| colspan="1" rowspan="1" style="padding: 5px 5px; background: #DCDCDC;" align="center" | [[Peptic Ulcer Disease|Peptic ulcer disease]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |Diffuse | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | <nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | <nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
* Gastric ulcer- [[melena]] and [[hematemesis]] | |||
* Duodenal ulcer- [[melena]] and [[hematochezia]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | Positive if perforated | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | Positive if perforated | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | Positive if perforated | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |N | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Ascitic fluid | |||
** [[LDH]] > serum [[LDH]] | |||
** Glucose < 50mg/dl | |||
** Total protein > 1g/dl | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Air under [[diaphragm]] in upright [[CXR]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Upper GI [[endoscopy]] for diagnosis | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Gastritis|Gastritis]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |[[Epigastric]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | <nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | Positive in chronic gastritis | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |N | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* [[H.pylori infection diagnostic tests]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* [[Endoscopy]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* [[H.pylori gastritis guideline recommendation]] | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Gastrointestinal perforation]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |Diffuse | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>-</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |− | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |− | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |Hyperactive/hypoactive | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* WBC> 10,000 | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Air under [[diaphragm]] in upright [[CXR]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* [[Hamman's sign]] | |||
|- | |||
| colspan="1" rowspan="1" style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Diverticulitis|Acute diverticulitis]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |LLQ | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |− | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | Positive in perforated diverticulitis | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |Hypoactive | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* [[Leukocytosis]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* CT scan | |||
* Ultrasound | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* History of [[constipation]] | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Inflammatory bowel disease]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |Diffuse | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |Normal or hyperactive | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* [[Anti-neutrophil cytoplasmic antibody]] ([[P-ANCA]]) in [[Ulcerative colitis]] | |||
* [[Anti saccharomyces cerevisiae antibodies]] (ASCA) in [[Crohn's disease]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* [[String sign]] on [[abdominal x-ray]] in [[Crohn's disease]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
Extra intestinal findings: | |||
* [[Uveitis]] | |||
* [[Arthritis]] | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Infective colitis]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |Diffuse | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | Positive in fulminant colitis | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |Hyperactive | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* [[Stool culture]] and studies | |||
* Shiga toxin in bloody diarrhea | |||
* [[PCR]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |CT scan | |||
* Bowel wall thickening | |||
* Edema | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC;" align="center" |Colon carcinoma | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |Diffuse/localized | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Normal or hyperactive if obstruction present | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* CBC | |||
* Carcinoembryonic antigen (CEA) | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Colonoscopy | |||
* Flexible sigmoidoscopy | |||
* Barium enema | |||
* CT colonography | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* PILLCAM 2: A colon capsule for CRC screening may be used in patients with an incomplete colonoscopy who lacks obstruction | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Budd-Chiari syndrome|Budd-Chiari syndrome]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |[[RUQ]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | Positive in liver failure leading to varices | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |N | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
*Elevated [[Aspartate aminotransferase|serum aspartate aminotransferase]] and [[alanine aminotransferase]] levels may be more than five times the upper limit of the normal range. | |||
*Elevated serum [[alkaline phosphatase]] and [[Bilirubin|bilirubin levels]], decreased [[Albumin|serum albumin level]]. | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
{| style="border: 0px; font-size: 90%; margin: 3px;" align="center" | |||
|- | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |Findings on [[CT scan]] suggestive of Budd-Chiari syndrome include: | |||
*Early enhancement of the [[caudate lobe]] and [[central liver]] around the [[Inferior vena cavae|inferior vena cava]] | |||
*Delayed enhancement of the peripheral [[liver]] with accompanying central low density (flip-flop appearance) | |||
*Peripheral zones of the [[liver]] show reversed [[portal]] [[venous]] [[blood flow]] | |||
*In the [[chronic]] phase, there is [[caudate lobe]] enlargement and [[atrophy]] of the [[Liver|peripheral liver]] in affected areas | |||
|} | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |[[Ascitic tap|Ascitic fluid examination]] shows: | |||
*[[Total protein]] more than 2.5 g per deciliter | |||
*[[White blood cells]] are usually less than 500/μL. | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Hemochromatosis]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |RUQ | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | Positive in cirrhotic patients | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |N | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* >60% TS | |||
* >240 μg/L SF | |||
* Raised LFT <br>Hyperglycemia | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Ultrasound shows evidence of cirrhosis | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |Extra intestinal findings: | |||
* Hyperpigmentation | |||
* Diabetes mellitus | |||
* Arthralgia | |||
* Impotence in males | |||
* Cardiomyopathy | |||
* Atherosclerosis | |||
* Hypopituitarism | |||
* Hypothyroidism | |||
* Extrahepatic cancer | |||
* Prone to specific infections | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Cirrhosis|Cirrhosis]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |[[RUQ]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |N | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* [[Hypoalbuminemia]] | |||
* Prolonged PT | |||
* Abnormal LFTs | |||
* [[Hyponatremia]] | |||
* [[Thrombocytopenia]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |US | |||
* Nodular, shrunken liver | |||
* [[Ascites]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Stigmata of liver disease | |||
* Cruveilhier- Baumgarten murmur | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Mesenteric ischemia]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |Periumbilical | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |Positive if bowel becomes gangrenous | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | Positive if bowel becomes gangrenous | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | Positive if bowel becomes gangrenous | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |Hyperactive to absent | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* [[Leukocytosis]] and [[lactic acidosis]] | |||
* [[Amylase]] levels | |||
* [[D-dimer]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |CT angiography | |||
* SMA or SMV thrombosis | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Also known as abdominal angina that worsens with eating | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Ischemic colitis|Acute ischemic colitis]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | Diffuse | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |Hyperactive then absent | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* [[Leukocytosis]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |[[Abdominal x-ray]] | |||
* Distension and pneumatosis | |||
CT scan | |||
* Double halo appearance, thumbprinting | |||
* Thickening of bowel | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* May lead to shock | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Ruptured abdominal aortic aneurysm]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | Diffuse | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |N | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* [[Fibrinogen]] | |||
* [[D-dimer]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Focused Assessment with Sonography in Trauma (FAST) | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Unstable hemodynamics | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC;" align="center" |Intra-abdominal or [[retroperitoneal hemorrhage]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | Diffuse | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |N | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* ↓ Hb | |||
* ↓ Hct | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* CT scan | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* History of [[trauma]] | |||
|- | |||
|} | |||
|} | |||
==References== | |||
{{Reflist|2}} | |||
== Overview == | |||
* The page name should be '''"[Disease name] diagnostic study of choice"''', with only the first letter of the title capitalized. Note that the page is called "Diagnostic study of choice." | |||
* '''Goal:''' | |||
**To describe the most efficient/sensitive/specific test that is utilized for diagnosis of [disease name]. | |||
**To describe the gold standard test for the diagnosis of [disease name]. | |||
**To describe the diagnostic criteria, which may be based on clinical findings, physical exam signs, pathological findings, lab findings, findings on imaging, or even findings that exclude other diseases. | |||
* As with all microchapter pages linking to the main page, at the top of the edit box put <nowiki>{{CMG}}</nowiki>, your name template, and the microchapter navigation template you created at the beginning. | |||
* Remember to create links within WikiDoc by placing <nowiki>[[square brackets]]</nowiki> around key words which you want to link to other pages. Make sure you makes your links as specific as possible. For example, if a sentence contained the phrase anterior spinal artery syndrome, the link should be to [[anterior spinal artery syndrome]] not [[anterior]] or [[artery]] or [[syndrome]]. For more information on how to create links, click [[here]]. | |||
* Remember to follow the same format and capitalization of letters as outlined in the template below. | |||
* You should include the name of the disease in the first sentence of every subsection. | |||
== Diagnostic Study of Choice == | |||
===== Template statements ===== | |||
=== Gold standard/Study of choice: === | |||
* [Name of the investigation] is the gold standard test for the diagnosis of [disease name]. | |||
* The following result of [gold standard test] is confirmatory of [disease name]: | |||
** Result 1 | |||
** Result 2 | |||
* The [name of investigation] should be performed when: | |||
** The patient presented with symptoms/signs 1. 2, 3. | |||
** A positive [test] is detected in the patient. | |||
* [Name of the investigation] is the gold standard test for the diagnosis of [disease name]. | |||
* The diagnostic study of choice for [disease name] is [name of investigation]. | |||
* There is no single diagnostic study of choice for the diagnosis of [disease name]. | |||
* There is no single diagnostic study of choice for the diagnosis of [disease name], but [disease name] can be diagnosed based on [name of the investigation 1] and [name of the investigation 2]. | |||
* [Disease name] is mainly diagnosed based on clinical presentation. | |||
* Investigations: | |||
** Among patients who present with clinical signs of [disease name], the [investigation name] is the most specific test for the diagnosis. | |||
** Among patients who present with clinical signs of [disease name], the [investigation name] is the most sensitive test for diagnosis. | |||
** Among patients who present with clinical signs of [disease name], the [investigation name] is the most efficient test for diagnosis. | |||
==== The comparison table for diagnostic studies of choice for [disease name] ==== | |||
{| | |||
|- style="background: #4479BA; color: #FFFFFF; text-align: center;" | |||
! style="background: #FFFFFF; color: #FFFFFF; text-align: center;" | | |||
! style="background: #4479BA; color: #FFFFFF; text-align: center;" |Sensitivity | |||
! style="background: #4479BA; color: #FFFFFF; text-align: center;" |Specificity | |||
|- | |||
! style="background: #696969; color: #FFFFFF; text-align: center;" |Test 1 | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |✔ | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |...% | |||
|- | |||
! style="background: #696969; color: #FFFFFF; text-align: center;" |Test 2 | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |...% | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |✔ | |||
|} | |||
<small> ✔= The best test based on the feature </small> | |||
===== Diagnostic results ===== | |||
The following result of [investigation name] is confirmatory of [disease name]: | |||
* Result 1 | |||
* Result 2 | |||
===== Sequence of Diagnostic Studies ===== | |||
The [name of investigation] should be performed when: | |||
* The patient presented with symptoms/signs 1, 2, and 3 as the first step of diagnosis. | |||
* A positive [test] is detected in the patient, to confirm the diagnosis. | |||
=== Diagnostic Criteria === | |||
* Here you should describe the details of the diagnostic criteria. | |||
*Always mention the name of the criteria/definition you are about to list (e.g. modified Duke criteria for diagnosis of endocarditis / 3rd universal definition of MI) and cite the primary source of where this criteria/definition is found. | |||
*Although not necessary, it is recommended that you include the criteria in a table. Make sure you always cite the source of the content and whether the table has been adapted from another source. | |||
*Be very clear as to the number of criteria (or threshold) that needs to be met out of the total number of criteria. | |||
*Distinguish criteria based on their nature (e.g. clinical criteria / pathological criteria/ imaging criteria) before discussing them in details. | |||
*To view an example (endocarditis diagnostic criteria), click [[Endocarditis diagnosis|here]] | |||
*If relevant, add additional information that might help the reader distinguish various criteria or the evolution of criteria (e.g. original criteria vs. modified criteria). | |||
*You may also add information about the sensitivity and specificity of the criteria, the pre-test probability, and other figures that may help the reader understand how valuable the criteria are clinically. | |||
* [Disease name] is mainly diagnosed based on clinical presentation. There are no established criteria for the diagnosis of [disease name]. | |||
* There is no single diagnostic study of choice for [disease name], though [disease name] may be diagnosed based on [name of criteria] established by [...]. | |||
* The diagnosis of [disease name] is made when at least [number] of the following [number] diagnostic criteria are met: [criterion 1], [criterion 2], [criterion 3], and [criterion 4]. | |||
* The diagnosis of [disease name] is based on the [criteria name] criteria, which includes [criterion 1], [criterion 2], and [criterion 3]. | |||
* [Disease name] may be diagnosed at any time if one or more of the following criteria are met: | |||
** Criteria 1 | |||
** Criteria 2 | |||
** Criteria 3 | |||
IF there are clear, established diagnostic criteria: | |||
*The diagnosis of [disease name] is made when at least [number] of the following [number] diagnostic criteria are met: [criterion 1], [criterion 2], [criterion 3], and [criterion 4]. | |||
*The diagnosis of [disease name] is based on the [criteria name] criteria, which include [criterion 1], [criterion 2], and [criterion 3]. | |||
*The diagnosis of [disease name] is based on the [definition name] definition, which includes [criterion 1], [criterion 2], and [criterion 3]. | |||
IF there are no established diagnostic criteria: | |||
*There are no established criteria for the diagnosis of [disease name]. | |||
==References== | |||
* References should be cited for the material that you have put on your page. Type in <nowiki>{{reflist|2}}</nowiki>.This will generate your references in small font, in two columns, with links to the original article and abstract. | |||
* For information on how to add references into your page, click [[Adding References to Articles|here]]. | |||
{{CMG}}; {{AE}} | |||
==Overview== | |||
The majority of patients with [disease name] are asymptomatic. | |||
OR | |||
The hallmark of [disease name] is [finding]. A positive history of [finding 1] and [finding 2] is suggestive of [disease name]. The most common symptoms of [disease name] include [symptom 1], [symptom 2], and [symptom 3]. Common symptoms of [disease] include [symptom 1], [symptom 2], and [symptom 3]. Less common symptoms of [disease name] include [symptom 1], [symptom 2], and [symptom 3]. | |||
==History and Symptoms== | |||
*Symptoms of Peutz-Jegher syndrome include abnormal pigmentation of the oral mucosa, abdominal pain, blood in stool, and extrusion of anal polyp. | |||
===History=== | |||
Patients with Peutz-Jegher syndrome may have a positive history of: | |||
*Intussesception at a young age | |||
==References== | |||
{{Reflist|2}} | |||
{{WH}} | |||
{{WS}} | |||
[[Category: (name of the system)]] | |||
{{CMG}}; {{AE}} | |||
==Overview== | |||
Patients with [disease name] usually appear [general appearance]. Physical examination of patients with [disease name] is usually remarkable for [finding 1], [finding 2], and [finding 3]. | |||
OR | |||
Common physical examination findings of [disease name] include [finding 1], [finding 2], and [finding 3]. | |||
OR | |||
The presence of [finding(s)] on physical examination is diagnostic of [disease name]. | |||
OR | |||
The presence of [finding(s)] on physical examination is highly suggestive of [disease name]. | |||
==Physical Examination== | |||
*Physical examination of patients with [disease name] is usually remarkable for:[finding 1], [finding 2], and [finding 3]. | |||
*The presence of [finding(s)] on physical examination is diagnostic of [disease name]. | |||
*The presence of [finding(s)] on physical examination is highly suggestive of [disease name]. | |||
===Appearance of the Patient=== | |||
*Patients with [disease name] usually appear [general appearance]. | |||
===Vital Signs=== | |||
*High-grade / low-grade fever | |||
*[[Hypothermia]] / hyperthermia may be present | |||
*[[Tachycardia]] with regular pulse or (ir)regularly irregular pulse | |||
*[[Bradycardia]] with regular pulse or (ir)regularly irregular pulse | |||
*Tachypnea / bradypnea | |||
*Kussmal respirations may be present in _____ (advanced disease state) | |||
*Weak/bounding pulse / pulsus alternans / paradoxical pulse / asymmetric pulse | |||
*High/low blood pressure with normal pulse pressure / [[wide pulse pressure]] / [[narrow pulse pressure]] | |||
===Skin=== | |||
*[[Cyanosis]] | |||
*[[Jaundice]] | |||
* [[Pallor]] | |||
* Bruises | |||
<gallery widths="150px"> | |||
UploadedImage-01.jpg | Description {{dermref}} | |||
UploadedImage-02.jpg | Description {{dermref}} | |||
</gallery> | |||
===HEENT=== | |||
* Abnormalities of the head/hair may include ___ | |||
* Evidence of trauma | |||
* Icteric sclera | |||
* [[Nystagmus]] | |||
* Extra-ocular movements may be abnormal | |||
*Pupils non-reactive to light / non-reactive to accomodation / non-reactive to neither light nor accomodation | |||
*Ophthalmoscopic exam may be abnormal with findings of ___ | |||
* Hearing acuity may be reduced | |||
*[[Weber test]] may be abnormal (Note: A positive Weber test is considered a normal finding / A negative Weber test is considered an abnormal finding. To avoid confusion, you may write "abnormal Weber test".) | |||
*[[Rinne test]] may be positive (Note: A positive Rinne test is considered a normal finding / A negative Rinne test is considered an abnormal finding. To avoid confusion, you may write "abnormal Rinne test".) | |||
* [[Exudate]] from the ear canal | |||
* Tenderness upon palpation of the ear pinnae / tragus (anterior to ear canal) | |||
*Inflamed nares / congested nares | |||
* [[Purulent]] exudate from the nares | |||
* Facial tenderness | |||
* Erythematous throat with/without tonsillar swelling, exudates, and/or petechiae | |||
===Neck=== | |||
*[[Jugular venous distension]] | |||
*[[Carotid bruits]] may be auscultated unilaterally/bilaterally using the bell/diaphragm of the otoscope | |||
*[[Lymphadenopathy]] (describe location, size, tenderness, mobility, and symmetry) | |||
*[[Thyromegaly]] / thyroid nodules | |||
*[[Hepatojugular reflux]] | |||
===Lungs=== | |||
* Asymmetric chest expansion / Decreased chest expansion | |||
*Lungs are hypo/hyperresonant | |||
*Fine/coarse [[crackles]] upon auscultation of the lung bases/apices unilaterally/bilaterally | |||
*Rhonchi | |||
*Vesicular breath sounds / Distant breath sounds | |||
*Expiratory/inspiratory wheezing with normal / delayed expiratory phase | |||
*[[Wheezing]] may be present | |||
*[[Egophony]] present/absent | |||
*[[Bronchophony]] present/absent | |||
*Normal/reduced [[tactile fremitus]] | |||
===Heart=== | |||
*Chest tenderness upon palpation | |||
*PMI within 2 cm of the sternum (PMI) / Displaced point of maximal impulse (PMI) suggestive of ____ | |||
*[[Heave]] / [[thrill]] | |||
*[[Friction rub]] | |||
*[[Heart sounds#First heart tone S1, the "lub"(components M1 and T1)|S1]] | |||
*[[Heart sounds#Second heart tone S2 the "dub"(components A2 and P2)|S2]] | |||
*[[Heart sounds#Third heart sound S3|S3]] | |||
*[[Heart sounds#Fourth heart sound S4|S4]] | |||
*[[Heart sounds#Summation Gallop|Gallops]] | |||
*A high/low grade early/late [[systolic murmur]] / [[diastolic murmur]] best heard at the base/apex/(specific valve region) may be heard using the bell/diaphgram of the otoscope | |||
===Abdomen=== | |||
*[[Abdominal distention]] | |||
*[[Abdominal tenderness]] in the right/left upper/lower abdominal quadrant | |||
*[[Rebound tenderness]] (positive Blumberg sign) | |||
*A palpable abdominal mass in the right/left upper/lower abdominal quadrant | |||
*Guarding may be present | |||
*[[Hepatomegaly]] / [[splenomegaly]] / [[hepatosplenomegaly]] | |||
*Additional findings, such as obturator test, psoas test, McBurney point test, Murphy test | |||
===Back=== | |||
*Point tenderness over __ vertebrae (e.g. L3-L4) | |||
*Sacral edema | |||
*Costovertebral angle tenderness bilaterally/unilaterally | |||
*Buffalo hump | |||
===Genitourinary=== | |||
*A pelvic/adnexal mass may be palpated | |||
*Inflamed mucosa | |||
*Clear/(color), foul-smelling/odorless penile/vaginal discharge | |||
===Neuromuscular=== | |||
*Patient is usually oriented to persons, place, and time | |||
* Altered mental status | |||
* Glasgow coma scale is ___ / 15 | |||
* Clonus may be present | |||
* Hyperreflexia / hyporeflexia / areflexia | |||
* Positive (abnormal) Babinski / plantar reflex unilaterally/bilaterally | |||
* Muscle rigidity | |||
* Proximal/distal muscle weakness unilaterally/bilaterally | |||
* ____ (finding) suggestive of cranial nerve ___ (roman numerical) deficit (e.g. Dilated pupils suggestive of CN III deficit) | |||
*Unilateral/bilateral upper/lower extremity weakness | |||
*Unilateral/bilateral sensory loss in the upper/lower extremity | |||
*Positive straight leg raise test | |||
*Abnormal gait (describe gait: e.g. ataxic (cerebellar) gait / steppage gait / waddling gait / choeiform gait / Parkinsonian gait / sensory gait) | |||
*Positive/negative Trendelenburg sign | |||
*Unilateral/bilateral tremor (describe tremor, e.g. at rest, pill-rolling) | |||
*Normal finger-to-nose test / Dysmetria | |||
*Absent/present dysdiadochokinesia (palm tapping test) | |||
===Extremities=== | |||
*[[Clubbing]] | |||
*[[Cyanosis]] | |||
*Pitting/non-pitting [[edema]] of the upper/lower extremities | |||
*Muscle atrophy | |||
*Fasciculations in the upper/lower extremity | |||
==References== | |||
{{Reflist|2}} | |||
{{WH}} | |||
{{WS}} | |||
[[Category: (name of the system)]] | |||
{{CMG}}; {{AE}} | |||
==Overview== | |||
An elevated/reduced concentration of serum/blood/urinary/CSF/other [lab test] is diagnostic of [disease name]. | |||
OR | |||
Laboratory findings consistent with the diagnosis of [disease name] include [abnormal test 1], [abnormal test 2], and [abnormal test 3]. | |||
OR | OR | ||
[Test] is usually normal among patients with [disease name]. | |||
OR | OR | ||
Some patients with [disease name] may have elevated/reduced concentration of [test], which is usually suggestive of [progression/complication]. | |||
OR | OR | ||
There are no diagnostic laboratory findings associated with [disease name]. | |||
== | |||
*There are no | ==Laboratory Findings== | ||
*There are no diagnostic laboratory findings associated with [disease name]. | |||
OR | OR | ||
* | *An elevated/reduced concentration of serum/blood/urinary/CSF/other [lab test] is diagnostic of [disease name]. | ||
*[Test] is usually normal among patients with [disease name]. | |||
*Laboratory findings consistent with the diagnosis of [disease name] include: | |||
**[Abnormal test 1] | |||
**[Abnormal test 2] | |||
**[Abnormal test 3] | |||
* | *Some patients with [disease name] may have elevated/reduced concentration of [test], which is usually suggestive of [progression/complication]. | ||
== | ==References== | ||
{{Reflist|2}} | |||
{{WH}} | |||
{{WS}} | |||
[[Category: (name of the system)]] | |||
{{CMG}}; {{AE}} | |||
==Overview== | |||
There are no ECG findings associated with [disease name]. | |||
OR | |||
An ECG may be helpful in the diagnosis of [disease name]. Findings on an ECG suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3]. | |||
==Electrocardiogram== | |||
*There are no ECG findings associated with [disease name]. | |||
OR | |||
*An ECG may be helpful in the diagnosis of [disease name]. Findings on an ECG suggestive of/diagnostic of [disease name] include | |||
**[Finding 1] | |||
**[Finding 2] | |||
**[Finding 3] | |||
==References== | ==References== | ||
{{Reflist|2}} | {{Reflist|2}} | ||
{{WH}} | |||
{{WS}} | |||
Latest revision as of 04:13, 16 April 2018
| Sandbox:Hamid | |
| ICD-10 | K42 |
|---|---|
| ICD-9 | 551-553 |
| DiseasesDB | 23647 |
| MedlinePlus | 000987 |
| MeSH | D006554 |
Salm.. ==Historical Perspective== [1]
Discovery
- Salmonella was first discovered by Daniel E. Salmon, an American veterinarian, who first isolated Salmonella choleraesuis from pigs in 1884 with hog cholera.
- The association between [important risk factor/cause] and [disease name] was made in/during [year/event].
- In [year], [scientist] was the first to discover the association between [risk factor] and the development of [disease name].
- In [year], [gene] mutations were first implicated in the pathogenesis of [disease name].
Outbreaks
- There have been several outbreaks of [disease name], which are summarized below:
Landmark Events in the Development of Treatment Strategies
- In [year], [diagnostic test/therapy] was developed by [scientist] to treat/diagnose [disease name].
Impact on Cultural History
Famous Cases
- The following are a few famous cases of disease name:
Classification
- [Disease name] may be classified according to Kaufmann-White typing system into [number] subtypes:
- Somatic O
- Surface Vi
- Flagellar H antigens
Pathophysiology
After ingestion, infection with salmonellae is characterized by attachment of the bacteria by fimbriae or pili to cells lining the intestinal lumen. Salmonellae selectively attach to specialized epithelial cells (M cells) of the Peyer patches. The bacteria are then internalized by receptor-mediated endocytosis and transported within phagosomes to the lamina propria, where they are released. Once there, salmonellae induce an influx of macrophages (typhoidal strains) or neutrophils (nontyphoidal strains).
The Vi antigen of S typhi is important in preventing antibody-mediated opsonization and complement-mediated lysis. Through the induction of cytokine release and via mononuclear cell migration, S typhi organisms spread through the reticuloendothelial system, mainly to the liver, spleen, and bone marrow. Within 14 days, the bacteria appear in the bloodstream, facilitating secondary metastatic foci (eg, splenic abscess, endocarditis). In some patients, gallbladder infection leads to long-term carriage of S typhi or S paratyphi in bile and secretion to the stool. [17] As a rule, infection with nontyphoidal salmonellae generally precipitates a localized response, while S typhi and other especially virulent strains invade deeper tissues via lymphatics and capillaries and elicit a major immune response.
Pathogenesis
- It is understood that [disease name] is the result of / is mediated by / is produced by / is caused by either [hypothesis 1], [hypothesis 2], or [hypothesis 3].
- [Pathogen name] is usually transmitted via the [transmission route] route to the human host.
- Following ingestion, salmonella uses the [entry site] to invade the [cell name] cell.
- [Disease or malignancy name] arises from [cell name]s, which are [cell type] cells that are normally involved in [function of cells].
- The progression to [disease name] usually involves the [molecular pathway].
- The pathophysiology of [disease/malignancy] depends on the histological subtype.
Genetics
- [Disease name] is transmitted in [mode of genetic transmission] pattern.
- Genes involved in the pathogenesis of [disease name] include [gene1], [gene2], and [gene3].
- The development of [disease name] is the result of multiple genetic mutations.
Associated Conditions
Gross Pathology
- On gross pathology, [feature1], [feature2], and [feature3] are characteristic findings of [disease name].
Microscopic Pathology
- On microscopic histopathological analysis, [feature1], [feature2], and [feature3] are characteristic findings of [disease name].
Overview
<figure-inline><figure-inline><figure-inline>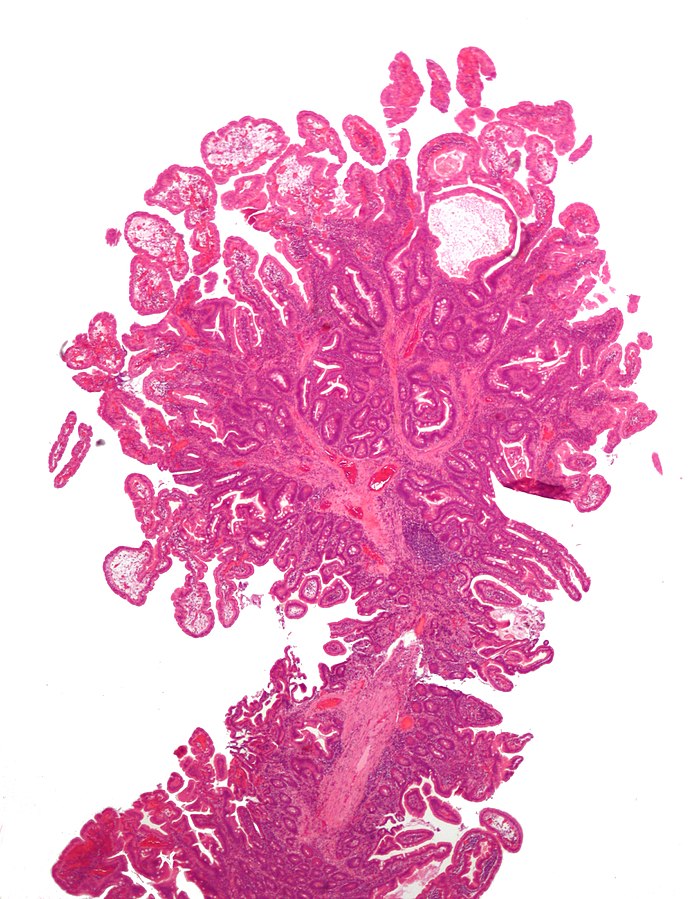 </figure-inline></figure-inline></figure-inline>
</figure-inline></figure-inline></figure-inline>
Historical Perspective
- Peutz-Jeghers syndrome was first discovered by Dr. Connor, a British, in 1895 in identical twin sisters.
- The association between gastrointestinal polyposis with distinctive pigmentation of the skin and Peutz-Jeghers syndrome was made in 1921 by Dr. Johannes Peutz of Holland.
- In 1949, Dr. Harold Jeghers of United States was the first to discover the association between combination of intestinal polyposis and skin pigmentation, and the development of Peutz-Jeghers syndrome.
- In 1954, A. Bruwer used the eponym Peutz-Jeghers syndrome
- In 1998, serine/threonine-protein kinase 11 alias LKB1 (STK11/LKB1) gene mutations were first implicated in the pathogenesis of Peutz-Jeghers syndrome.
Classification
- There is no established system for the classification of Peutz-Jeghers syndrome.
Pathophysiology
Pathogenesis
- It is thought that Peutz-Jeghers syndrome is the result of deletion or partial deletion of STK11 (LBK1) gene, located on chromosome 19p13.3.[1]
- STK11 protein plays an important role in second messenger signal transduction and is found to regulate cellular proliferation, controls cell polarity, and responds to low energy states.
- In Mammalian studies, STK11 is shown in the inhibition of AMP-activated protein kinase (AMPK), and signals downstream to inhibit the mammalian target of rapamycin (mTOR).[1]
- The mTOR pathway is dysregulated in Peutz-Jeghers syndrome.
Pathology
- Peutz-Jeghers syndrome associated polyps have a unique smooth muscle core that arborizes throughout the polyp.[1]
- These polyps can only be differentiated from other polyp types by histopathology.
Causes
- Peutz-Jeghers syndrome is caused by STK11 gene mutation
- Variable penetrance
Epidemiology and Demographics
Prevalence
- The prevalence of Peutz-Jeghers syndrome is estimated to be 1 in 8300 to 250000
- Most likely prevalence is 1 in 100000
Age
- Peutz-Jeghers syndrome affects individuals between the ages of 10 to 30 years; average age of diagnosis is 23 years for males and 26 years for females.
Gender
- Males and females are equally affected.
Risk Factors
- There are no established risk factors for Peutz-Jeghers
Screening
- According to the American College of Gastroenterology (ACG) and the National Comprehensive Cancer Network (NCCN), screening for Peutz-Jeghers syndrome by physical exam, complete blood work for iron deficiency anemia, and endoscopy are recommended every year among patients with Peutz-Jeghers Syndrome.
Natural History, Complications, and Prognosis
Natural History
- The symptoms of Peutz-Jeghers syndrome usually develop in the first decade of life, and start with symptoms such as hyperpigmentation, abdominal pain, and rectal bleeding.
- If left untreated, patients with Peutz-Jeghers syndrome may progress to develop colon cancer, breast cancer, and gastrointestinal cancers.
- Extraintestinal manifestation include pancreatic, lung, breast, uterine, ovarian and testicular malignancies.
Complications
- Common complications of Peutz-Jeghers syndrome include:
- Intussusception
- Gastric outlet obstruction
- Extraintestinal polyps
Prognosis
- Prognosis is generally excellent/good/poor, and the 1/5/10-year mortality/survival rate of patients with [disease name] is approximately [#]%.
- Depending on the extent of the [tumor/disease progression/etc.] at the time of diagnosis, the prognosis may vary. However, the prognosis is generally regarded as poor/good/excellent.
- The presence of [characteristic of disease] is associated with a particularly [good/poor] prognosis among patients with [disease/malignancy].
- [Subtype of disease/malignancy] is associated with the most favorable prognosis.
- The prognosis varies with the [characteristic] of tumor; [subtype of disease/malignancy] have the most favorable prognosis.
Signs and Symptoms Differential compared to Peutz-Jeghers Syndrome
"Peutz-Jeghers Syndrome - GeneReviews® - NCBI Bookshelf".
| Diseases | History and Symptoms | Physical Examination | Laboratory Findings | Other Findings | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Abdominal Pain | Rectal Bleeding | Hyperpigmentation | Fatigue | Abdominal Pain | Hyperpigmentation | Anemia | Physical Finding 4 | Gene(s) | Sertoli Cell Tumors | Gastrointestinal Tumors | Cancers | ||
| Juvenile Polyposis Syndrome | + | - | + | - | - | SMAD4
BMPR1A |
- | Adenoma+
Hamartoma+++ |
Colon | ||||
| Cowden Syndrome | - | - | Axillary+
Inguinal+ Facial+ |
- | Axillary+
Inguinal+ Facial+ |
- | PTEN | - | Adenoma+
Hamartoma+++ |
Breast, Thyroid, Endometrium | Trichilemmoma, skin hamartoma, hyperplastic polyps, macrocephaly, breast fibrosis | ||
| Carney Syndrome | - | - | Facial+
Mucosal+ |
- | Facial+
Mucosal+ |
- | PRKAR1A | ++ | Thyroid | Myxomas of skin and heart | |||
| Familial Adenomatous Polyposis | + | + | - | + | - | + | APC | - | Adenoma+++ | Colon, brain | Desmoid tumors, osteomas | ||
| Hereditary Non-Polyposis Colon Cancer | - | + | - | + | - | + | MLH1
MSH2 MSH3 MSH6 PMS1 PMS2 |
- | Adenoma+ | Endometrial, gastric, renal pelvis, ureter, and ovarian | Sebaceous adenoma | ||
Use if the above table can not be made
| Differential Diagnosis | Similar Features | Differentiating Features |
|---|---|---|
| Juvenile Polyposis Syndrome |
|
|
| Cowden Syndrome |
|
|
| Carney Syndrome |
|
|
| Familial Adenomatous Polyposis |
|
|
| Hereditary Non-Polyposis Colon Cancer |
|
|
Differentiating Gastrointestinal Bleeding from other Diseases
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
References
- ↑ 1.0 1.1 1.2 1.3 Kopacova, Marcela; Tacheci, Ilja; Rejchrt, Stanislav; Bures, Jan (2009). "Peutz-Jeghers syndrome: Diagnostic and therapeuticapproach". World Journal of Gastroenterology. 15 (43): 5397. doi:10.3748/wjg.15.5397. ISSN 1007-9327.
- ↑ Giardiello, F; Trimbath, J (2006). "Peutz-Jeghers Syndrome and Management Recommendations". Clinical Gastroenterology and Hepatology. 4 (4): 408–415. doi:10.1016/j.cgh.2005.11.005. ISSN 1542-3565.
Overview
- The page name should be "[Disease name] diagnostic study of choice", with only the first letter of the title capitalized. Note that the page is called "Diagnostic study of choice."
- Goal:
- To describe the most efficient/sensitive/specific test that is utilized for diagnosis of [disease name].
- To describe the gold standard test for the diagnosis of [disease name].
- To describe the diagnostic criteria, which may be based on clinical findings, physical exam signs, pathological findings, lab findings, findings on imaging, or even findings that exclude other diseases.
- As with all microchapter pages linking to the main page, at the top of the edit box put {{CMG}}, your name template, and the microchapter navigation template you created at the beginning.
- Remember to create links within WikiDoc by placing [[square brackets]] around key words which you want to link to other pages. Make sure you makes your links as specific as possible. For example, if a sentence contained the phrase anterior spinal artery syndrome, the link should be to anterior spinal artery syndrome not anterior or artery or syndrome. For more information on how to create links, click here.
- Remember to follow the same format and capitalization of letters as outlined in the template below.
- You should include the name of the disease in the first sentence of every subsection.
Diagnostic Study of Choice
Template statements
Gold standard/Study of choice:
- [Name of the investigation] is the gold standard test for the diagnosis of [disease name].
- The following result of [gold standard test] is confirmatory of [disease name]:
- Result 1
- Result 2
- The [name of investigation] should be performed when:
- The patient presented with symptoms/signs 1. 2, 3.
- A positive [test] is detected in the patient.
- [Name of the investigation] is the gold standard test for the diagnosis of [disease name].
- The diagnostic study of choice for [disease name] is [name of investigation].
- There is no single diagnostic study of choice for the diagnosis of [disease name].
- There is no single diagnostic study of choice for the diagnosis of [disease name], but [disease name] can be diagnosed based on [name of the investigation 1] and [name of the investigation 2].
- [Disease name] is mainly diagnosed based on clinical presentation.
- Investigations:
- Among patients who present with clinical signs of [disease name], the [investigation name] is the most specific test for the diagnosis.
- Among patients who present with clinical signs of [disease name], the [investigation name] is the most sensitive test for diagnosis.
- Among patients who present with clinical signs of [disease name], the [investigation name] is the most efficient test for diagnosis.
The comparison table for diagnostic studies of choice for [disease name]
| Sensitivity | Specificity | |
|---|---|---|
| Test 1 | ✔ | ...% |
| Test 2 | ...% | ✔ |
✔= The best test based on the feature
Diagnostic results
The following result of [investigation name] is confirmatory of [disease name]:
- Result 1
- Result 2
Sequence of Diagnostic Studies
The [name of investigation] should be performed when:
- The patient presented with symptoms/signs 1, 2, and 3 as the first step of diagnosis.
- A positive [test] is detected in the patient, to confirm the diagnosis.
Diagnostic Criteria
- Here you should describe the details of the diagnostic criteria.
- Always mention the name of the criteria/definition you are about to list (e.g. modified Duke criteria for diagnosis of endocarditis / 3rd universal definition of MI) and cite the primary source of where this criteria/definition is found.
- Although not necessary, it is recommended that you include the criteria in a table. Make sure you always cite the source of the content and whether the table has been adapted from another source.
- Be very clear as to the number of criteria (or threshold) that needs to be met out of the total number of criteria.
- Distinguish criteria based on their nature (e.g. clinical criteria / pathological criteria/ imaging criteria) before discussing them in details.
- To view an example (endocarditis diagnostic criteria), click here
- If relevant, add additional information that might help the reader distinguish various criteria or the evolution of criteria (e.g. original criteria vs. modified criteria).
- You may also add information about the sensitivity and specificity of the criteria, the pre-test probability, and other figures that may help the reader understand how valuable the criteria are clinically.
- [Disease name] is mainly diagnosed based on clinical presentation. There are no established criteria for the diagnosis of [disease name].
- There is no single diagnostic study of choice for [disease name], though [disease name] may be diagnosed based on [name of criteria] established by [...].
- The diagnosis of [disease name] is made when at least [number] of the following [number] diagnostic criteria are met: [criterion 1], [criterion 2], [criterion 3], and [criterion 4].
- The diagnosis of [disease name] is based on the [criteria name] criteria, which includes [criterion 1], [criterion 2], and [criterion 3].
- [Disease name] may be diagnosed at any time if one or more of the following criteria are met:
- Criteria 1
- Criteria 2
- Criteria 3
IF there are clear, established diagnostic criteria:
- The diagnosis of [disease name] is made when at least [number] of the following [number] diagnostic criteria are met: [criterion 1], [criterion 2], [criterion 3], and [criterion 4].
- The diagnosis of [disease name] is based on the [criteria name] criteria, which include [criterion 1], [criterion 2], and [criterion 3].
- The diagnosis of [disease name] is based on the [definition name] definition, which includes [criterion 1], [criterion 2], and [criterion 3].
IF there are no established diagnostic criteria:
- There are no established criteria for the diagnosis of [disease name].
References
- References should be cited for the material that you have put on your page. Type in {{reflist|2}}.This will generate your references in small font, in two columns, with links to the original article and abstract.
- For information on how to add references into your page, click here.
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [2]; Associate Editor(s)-in-Chief:
Overview
The majority of patients with [disease name] are asymptomatic.
OR
The hallmark of [disease name] is [finding]. A positive history of [finding 1] and [finding 2] is suggestive of [disease name]. The most common symptoms of [disease name] include [symptom 1], [symptom 2], and [symptom 3]. Common symptoms of [disease] include [symptom 1], [symptom 2], and [symptom 3]. Less common symptoms of [disease name] include [symptom 1], [symptom 2], and [symptom 3].
History and Symptoms
- Symptoms of Peutz-Jegher syndrome include abnormal pigmentation of the oral mucosa, abdominal pain, blood in stool, and extrusion of anal polyp.
History
Patients with Peutz-Jegher syndrome may have a positive history of:
- Intussesception at a young age
References
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [3]; Associate Editor(s)-in-Chief:
Overview
Patients with [disease name] usually appear [general appearance]. Physical examination of patients with [disease name] is usually remarkable for [finding 1], [finding 2], and [finding 3].
OR
Common physical examination findings of [disease name] include [finding 1], [finding 2], and [finding 3].
OR
The presence of [finding(s)] on physical examination is diagnostic of [disease name].
OR
The presence of [finding(s)] on physical examination is highly suggestive of [disease name].
Physical Examination
- Physical examination of patients with [disease name] is usually remarkable for:[finding 1], [finding 2], and [finding 3].
- The presence of [finding(s)] on physical examination is diagnostic of [disease name].
- The presence of [finding(s)] on physical examination is highly suggestive of [disease name].
Appearance of the Patient
- Patients with [disease name] usually appear [general appearance].
Vital Signs
- High-grade / low-grade fever
- Hypothermia / hyperthermia may be present
- Tachycardia with regular pulse or (ir)regularly irregular pulse
- Bradycardia with regular pulse or (ir)regularly irregular pulse
- Tachypnea / bradypnea
- Kussmal respirations may be present in _____ (advanced disease state)
- Weak/bounding pulse / pulsus alternans / paradoxical pulse / asymmetric pulse
- High/low blood pressure with normal pulse pressure / wide pulse pressure / narrow pulse pressure
Skin
-
Description (Adapted from Dermatology Atlas)
-
Description (Adapted from Dermatology Atlas)
HEENT
- Abnormalities of the head/hair may include ___
- Evidence of trauma
- Icteric sclera
- Nystagmus
- Extra-ocular movements may be abnormal
- Pupils non-reactive to light / non-reactive to accomodation / non-reactive to neither light nor accomodation
- Ophthalmoscopic exam may be abnormal with findings of ___
- Hearing acuity may be reduced
- Weber test may be abnormal (Note: A positive Weber test is considered a normal finding / A negative Weber test is considered an abnormal finding. To avoid confusion, you may write "abnormal Weber test".)
- Rinne test may be positive (Note: A positive Rinne test is considered a normal finding / A negative Rinne test is considered an abnormal finding. To avoid confusion, you may write "abnormal Rinne test".)
- Exudate from the ear canal
- Tenderness upon palpation of the ear pinnae / tragus (anterior to ear canal)
- Inflamed nares / congested nares
- Purulent exudate from the nares
- Facial tenderness
- Erythematous throat with/without tonsillar swelling, exudates, and/or petechiae
Neck
- Jugular venous distension
- Carotid bruits may be auscultated unilaterally/bilaterally using the bell/diaphragm of the otoscope
- Lymphadenopathy (describe location, size, tenderness, mobility, and symmetry)
- Thyromegaly / thyroid nodules
- Hepatojugular reflux
Lungs
- Asymmetric chest expansion / Decreased chest expansion
- Lungs are hypo/hyperresonant
- Fine/coarse crackles upon auscultation of the lung bases/apices unilaterally/bilaterally
- Rhonchi
- Vesicular breath sounds / Distant breath sounds
- Expiratory/inspiratory wheezing with normal / delayed expiratory phase
- Wheezing may be present
- Egophony present/absent
- Bronchophony present/absent
- Normal/reduced tactile fremitus
Heart
- Chest tenderness upon palpation
- PMI within 2 cm of the sternum (PMI) / Displaced point of maximal impulse (PMI) suggestive of ____
- Heave / thrill
- Friction rub
- S1
- S2
- S3
- S4
- Gallops
- A high/low grade early/late systolic murmur / diastolic murmur best heard at the base/apex/(specific valve region) may be heard using the bell/diaphgram of the otoscope
Abdomen
- Abdominal distention
- Abdominal tenderness in the right/left upper/lower abdominal quadrant
- Rebound tenderness (positive Blumberg sign)
- A palpable abdominal mass in the right/left upper/lower abdominal quadrant
- Guarding may be present
- Hepatomegaly / splenomegaly / hepatosplenomegaly
- Additional findings, such as obturator test, psoas test, McBurney point test, Murphy test
Back
- Point tenderness over __ vertebrae (e.g. L3-L4)
- Sacral edema
- Costovertebral angle tenderness bilaterally/unilaterally
- Buffalo hump
Genitourinary
- A pelvic/adnexal mass may be palpated
- Inflamed mucosa
- Clear/(color), foul-smelling/odorless penile/vaginal discharge
Neuromuscular
- Patient is usually oriented to persons, place, and time
- Altered mental status
- Glasgow coma scale is ___ / 15
- Clonus may be present
- Hyperreflexia / hyporeflexia / areflexia
- Positive (abnormal) Babinski / plantar reflex unilaterally/bilaterally
- Muscle rigidity
- Proximal/distal muscle weakness unilaterally/bilaterally
- ____ (finding) suggestive of cranial nerve ___ (roman numerical) deficit (e.g. Dilated pupils suggestive of CN III deficit)
- Unilateral/bilateral upper/lower extremity weakness
- Unilateral/bilateral sensory loss in the upper/lower extremity
- Positive straight leg raise test
- Abnormal gait (describe gait: e.g. ataxic (cerebellar) gait / steppage gait / waddling gait / choeiform gait / Parkinsonian gait / sensory gait)
- Positive/negative Trendelenburg sign
- Unilateral/bilateral tremor (describe tremor, e.g. at rest, pill-rolling)
- Normal finger-to-nose test / Dysmetria
- Absent/present dysdiadochokinesia (palm tapping test)
Extremities
- Clubbing
- Cyanosis
- Pitting/non-pitting edema of the upper/lower extremities
- Muscle atrophy
- Fasciculations in the upper/lower extremity
References
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [4]; Associate Editor(s)-in-Chief:
Overview
An elevated/reduced concentration of serum/blood/urinary/CSF/other [lab test] is diagnostic of [disease name].
OR
Laboratory findings consistent with the diagnosis of [disease name] include [abnormal test 1], [abnormal test 2], and [abnormal test 3].
OR
[Test] is usually normal among patients with [disease name].
OR
Some patients with [disease name] may have elevated/reduced concentration of [test], which is usually suggestive of [progression/complication].
OR
There are no diagnostic laboratory findings associated with [disease name].
Laboratory Findings
- There are no diagnostic laboratory findings associated with [disease name].
OR
- An elevated/reduced concentration of serum/blood/urinary/CSF/other [lab test] is diagnostic of [disease name].
- [Test] is usually normal among patients with [disease name].
- Laboratory findings consistent with the diagnosis of [disease name] include:
- [Abnormal test 1]
- [Abnormal test 2]
- [Abnormal test 3]
- Some patients with [disease name] may have elevated/reduced concentration of [test], which is usually suggestive of [progression/complication].
References
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [5]; Associate Editor(s)-in-Chief:
Overview
There are no ECG findings associated with [disease name].
OR
An ECG may be helpful in the diagnosis of [disease name]. Findings on an ECG suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
Electrocardiogram
- There are no ECG findings associated with [disease name].
OR
- An ECG may be helpful in the diagnosis of [disease name]. Findings on an ECG suggestive of/diagnostic of [disease name] include
- [Finding 1]
- [Finding 2]
- [Finding 3]
