Unstable angina non ST elevation myocardial infarction risk stratification and prognosis
| Resident Survival Guide |
|
Unstable angina / NSTEMI Microchapters |
|
Differentiating Unstable Angina/Non-ST Elevation Myocardial Infarction from other Disorders |
|
Special Groups |
|
Diagnosis |
|
Laboratory Findings |
|
Treatment |
|
Antitplatelet Therapy |
|
Additional Management Considerations for Antiplatelet and Anticoagulant Therapy |
|
Risk Stratification Before Discharge for Patients With an Ischemia-Guided Strategy of NSTE-ACS |
|
Mechanical Reperfusion |
|
Discharge Care |
|
Case Studies |
|
Unstable angina non ST elevation myocardial infarction risk stratification and prognosis On the Web |
|
FDA on Unstable angina non ST elevation myocardial infarction risk stratification and prognosis |
|
CDC onUnstable angina non ST elevation myocardial infarction risk stratification and prognosis |
|
Unstable angina non ST elevation myocardial infarction risk stratification and prognosis in the news |
|
Blogs on Unstable angina non ST elevation myocardial infarction risk stratification and prognosis |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
To go to the chapter on PCI, click here.
Overview
There are several scoring systems which have been devised as methods of identifying high-risk patients presenting with acute coronary syndrome (ACS). These include, among others, the Braunwald classification system, the Rizik classification system, the TIMI risk score, the GRACE risk score, and the PURSUIT risk score.
Risk Stratification
- There are several scoring systems which have been devised as methods of identifying high-risk patients presenting with acute coronary syndrome (ACS). These include, among others, the Braunwald classification system,[1] the Rizik classification system,[2] the TIMI risk score,[3][4] the GRACE risk score[5][6] and the PURSUIT risk score.[7][8][9][10][11]
- In direct comparisons, the GRACE risk score is superior to TIMI risk score in assessing both prognosis and the severity of coronary artery disease in NSTEMI patients.[12][13]
- Regarding predicting the severity of CAD, a cross-sectional study published in 2018 used coronary angiogram to assess the severity of coronary artery disease using the vessel score & Gensini scores and correlated these scores with the GRACE and TIMI scores. The area under the ROC curve for the GRACE score (0.943; 95% CI = 0.893 - 0,993) was significantly superior to the area under the ROC curve for the TIMI score (0.892; 95% CI = 0.853 - 0.937)[13].
- Regarding 30 day mortality, a 2016 study correlated 30 day mortality in NSTEMI patients with the NT-proBNP biomarker, TIMI score, and GRACE scores. A total of 1324 patients were included in the study, which found both NT-proBNP (0.85) and the GRACE score (0.87) independently predicted mortality at 30 days, while the TIMI score (0.60) did not[12].
TIMI Risk Score
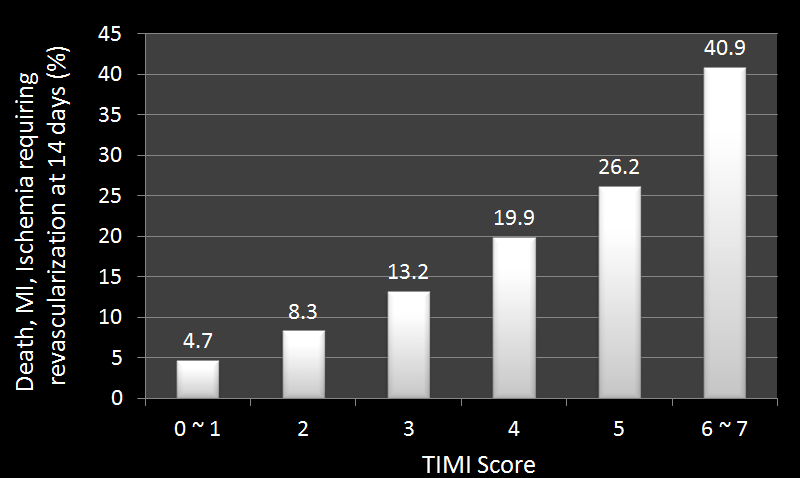
The TIMI Risk Score for UA/non-ST-elevation myocardial infarction (NSTEMI) is based on the TIMI 11B and ESSENCE trials and has been shown to be predictive of all-cause mortality, myocardial infarction, and severe recurrent myocardial ischemia prompting urgent revascularization for the first 14 days after presentation. It has also been validated as a tool for 30-day risk stratification of patients presenting to the emergency room with chest pain.[4] It is very likely the most commonly used tool for risk-stratification as it is the easiest to understand and use of those listed.
The TIMI risk score is determined by the sum of the presence of 7 variables at admission; 1 point is given for each of the following variables:[14]
- Age 65 years or older
- At least 3 risk factors for coronary artery disease
- Prior coronary artery stenosis of 50% or more
- ST segment deviation on EKG presentation
- At least 2 anginal events in prior 24 h
- Use of aspirin in prior 7 days
- Elevated serum levels of cardiac biomarkers
In TIMI risk scoring, prior coronary stenosis of 50% or more remained relatively insensitive to missing information and remained a significant predictor of events.[15][16]
Incidence of adverse events (all-cause mortality, myocardial infarction, and severe recurrent myocardial ischemia prompting urgent revascularization for the first 14 days after presentation):
- TIMI Risk Score 0/1: 4.7%
- TIMI Risk Score 2: 8.3%
- TIMI Risk Score 3: 13.2%
- TIMI Risk Score 4: 19.9%
- TIMI Risk Score 5: 26.2%
- TIMI Risk Score 6/7: 40.9%
Braunwald Classification
The Braunwald Classification of unstable angina pectoris (UAP) stratifies patients according to both the type of anginal pain and the underlying cause of the pain. Increasing class is associated with increasing risk of both recurrent ischemia and death at 6 months.
Characteristics
- Class I: Exertional angina (new onset, severe, or accelerated; angina of less than 2 months duration; more frequent angina; angina precipitated by less exertion; no rest angina in the last 2 months)
- Class II: Rest angina, subacute (rest angina within the last month but none within 48 hours of presentation)
- Class III: Rest angina, acute (rest angina within 48 hours of presentation)
Clinical Circumstances
- Class A: Secondary unstable angina (caused by a noncardiac condition such as anemia, infection, thyrotoxicosis or hypoxemia)
- Class B: Primary unstable angina
- Class C: Post-infarction unstable angina (within 2 weeks of documented myocardial infarction)
Rizik Classification Scheme
The Rizik classification scheme of UAP has been shown to be predictive of in-hospital adverse cardiac events and as such could be used to make decisions regarding hospitalization and intensity of treatment.[2]
- Class IA: Acceleration of previously existent chronic stable angina without new EKG changes
- Class IB: Acceleration of previously existent chronic stable angina with new EKG changes
- Class II: Exertional angina of new onset without respect to EKG morphology
- Class III: New onset resting angina (either with or without history of prior stable angina)
- Class IV: Patients with protracted chest pain of > 20 minutes with EKG changes
The PURSUIT Risk Score
The PURSUIT Risk score has been shown to be predictive of the 30-day incidence of death and the composite of death or myocardial (re)infarction in patients presenting with UA/NSTEMI (patients with ACS but without ST-elevation myocardial infarction). Points are given for each of the 7 below risk factors. The points are then summed to provide a risk score which can then be converted to a probability of either death or a composite of death or MI (from 0% to 50% depending on total points). [7]
- Age (increased probability for age above 60 and above)
- Gender (increased probability for men, no increased probability for women)
- Worst Canadian Cardiovascular Society Classification for angina pectoris in the previous 6 weeks (from angina only during very strenuous activity (Class I) to angina at rest (Class IV), increased probability for Class III or IV)
- Heart rate (increased probability for heart rate 100 and above)
- Systolic blood pressure (increased probability for systolic blood pressure 100 and below)
- Signs of heart failure (i.e., rales)
- ST-segment depression on presenting EKG
GRACE Risk Models
The GRACE model has been shown to be predictive of in-hospital mortality for patients presenting with ACS. The 8 risk factors listed below were shown to be the most strongly predictive. A probability of in-hospital death can be assigned by adding up the points allocated for each risk factor (range from <0.2% for less than 61 points to > 51% for more than 249 points). This model was validated as a tool to predict 6-month mortality in patients who survived hospital admission for ACS as well.[17]
- Increasing age (0-100 points)
- Increasing Killip class (0-59 points)
- Decreasing systolic blood pressure (0-58 points)
- ST-segment deviation (28 points)
- Cardiac arrest during presentation (39 points)
- Increasing serum creatinine level (1-28 points)
- Elevated initial cardiac enzymes (14 points)
- Increasing heart rate (0-46 points)
Risk Stratification Approach
The following table demonstrates the approach in a post ACS (unstable angina) patient based on 2007 ACC/AHA guidelines.[18]
| High Risk | Early invasive therapy |
| Intermediate Risk | Exercise ECG or Stress Imaging (after 2 - 3 days) |
| Low Risk | Exercise ECG or Stress Imaging (symptom free interval of 8 - 12 hours) |
2014 AHA/ACC Guideline for the Management of Patients With Non–ST-Elevation Acute Coronary Syndromes (DO NOT EDIT) [19]
Clinical Assessment and Initial Evaluation
| Class I |
| "1. Patients with suspected ACS should be risk stratified based on the likelihood of ACS and adverse outcome(s) to decide on the need for hospitalization and assist in the selection of treatment options. (Level of Evidence: B)" |
Emergency Department or Outpatient Facility Presentation
| Class I |
| "1. Patients with suspected ACS and high-risk features such as continuing chest pain, severe dyspnea, syncope/presyncope, or palpitations should be referred immediately to the emergency department (ED) and transported by emergency medical services when available. (Level of Evidence: C)" |
| Class IIb |
| "1. Patients with less severe symptoms may be considered for referral to the ED, a chest pain unit, or a facility capable of performing adequate evaluation depending on clinical circumstances. (Level of Evidence: C)" |
Early Risk Stratification
| Class I |
| "1. In patients with chest pain or other symptoms suggestive of ACS, a 12-lead ECG should be performed and evaluated for ischemic changes within 10 minutes of the patient’s arrival at an emergency facility. (Level of Evidence: C)" |
| "2. If the initial ECG is not diagnostic but the patient remains symptomatic and there is a high clinical suspicion for ACS, serial ECGs (e.g., 15- to 30-minute intervals during the first hour) should be performed to detect ischemic changes. (Level of Evidence: C)" |
| "3. Serial cardiac troponin I or T levels (when a contemporary assay is used) should be obtained at presentation and 3 to 6 hours after symptom onset in all patients who present with symptoms consistent with ACS to identify a rising and/or falling pattern of values. (Level of Evidence: A)" |
| "4. Additional troponin levels should be obtained beyond 6 hours after symptom onset in patients with normal troponin levels on serial examination when changes on ECG and/or clinical presentation confer an intermediate or high index of suspicion for ACS. (Level of Evidence: A)" |
| "5. Risk scores should be used to assess prognosis in patients with NSTE-ACS. (Level of Evidence: A)" |
| Class IIa |
| "1. Risk-stratification models can be useful in management. (Level of Evidence: B)" |
| "2. It is reasonable to obtain supplemental electrocardiographic leads V7 to V9 in patients whose initial ECG is nondiagnostic and who are at intermediate/high risk of ACS. (Level of Evidence: B)" |
| Class IIb |
| "1. Continuous monitoring with 12-lead ECG may be a reasonable alternative in patients whose initial ECG is nondiagnostic and who are at intermediate/high risk of ACS. (Level of Evidence: B)" |
| "2. Measurement of B-type natriuretic peptide or N-terminal pro–B-type natriuretic peptide may be considered to assess risk in patients with suspected ACS. (Level of Evidence: B)" |
2011 ACCF/AHA Focused Update Incorporated Into the ACC/AHA 2007 Guidelines for the Management of Patients With Unstable Angina/Non -ST-Elevation Myocardial Infarction (DO NOT EDIT)[18][20]
| Class I |
| "1. A rapid clinical determination of the likelihood risk of obstructive CAD (i.e., high, intermediate, or low) should be made in all patients with chest discomfort or other symptoms suggestive of an ACS and considered in patient management. (Level of Evidence: C)" |
| "2. Patients who present with chest discomfort or other ischemic symptoms should undergo early risk stratification for the risk of cardiovascular events (e.g., death or [re]MI) that focuses on history, including anginal symptoms, physical findings, ECG findings, and biomarkers of cardiac injury and results should be considered in patient management. (Level of Evidence: C)" |
| "3. A 12-lead ECG should be performed and shown to an experienced emergency physician as soon as possible after ED arrival, with a goal of within 10 min of ED arrival for all patients with chest discomfort (or anginal equivalent) or other symptoms suggestive of ACS. (Level of Evidence: B)" |
| "4. If the initial ECG is not diagnostic but the patient remains symptomatic and there is high clinical suspicion for ACS, serial ECGs, initially at 15- to 30-min intervals, should be performed to detect the potential for development of ST-segment elevation or depression. (Level of Evidence: B)" |
| "5. Cardiac biomarkers should be measured in all patients who present with chest discomfort consistent with ACS. (Level of Evidence: B)" |
| "6. A cardiac-specific troponin is the preferred marker, and if available, it should be measured in all patients who present with chest discomfort consistent with ACS. (Level of Evidence: B)" |
| "7. Patients with negative cardiac biomarkers within 6 h of the onset of symptoms consistent with ACS should have biomarkers remeasured in the time frame of 8 to 12 h after symptom onset. (The exact timing of serum marker measurement should take into account the uncertainties often present with the exact timing of onset of pain and the sensitivity, precision, and institutional norms of the assay being utilized as well as the release kinetics of the marker being measured.) (Level of Evidence: B)" |
|
"8. The initial evaluation of the patient with suspected ACS should include the consideration of noncoronary causes for the development of unexplained symptoms. (Level of Evidence: C)" |
| Class III |
| "1. Total CK (without MB), aspartate aminotransferase (AST, SGOT), alanine transaminase, beta-hydroxybutyric dehydrogenase, and/or lactate dehydrogenase should not be utilized as primary tests for the detection of myocardial injury in patients with chest discomfort suggestive of ACS. (Level of Evidence: C)" |
| Class IIa |
| "1. Use of risk-stratification models, such as the Thrombolysis In Myocardial Infarction (TIMI) or Global Registry of Acute Coronary Events (GRACE) risk score or the Platelet Glycoprotein IIb/IIIa in Unstable Angina: Receptor Suppression Using Integrilin Therapy (PURSUIT) risk model, can be useful to assist in decision making with regard to treatment options in patients with suspected ACS. (Level of Evidence: B)" |
| "2. It is reasonable to remeasure positive biomarkers at 6- to 8-h intervals 2 to 3 times or until levels have peaked, as an index of infarct size and dynamics of necrosis. (Level of Evidence: B)" |
| "3. It is reasonable to obtain supplemental ECG leads V7 through V9 in patients whose initial ECG is nondiagnostic to rule out MI due to left circumflex occlusion. (Level of Evidence: B)" |
| "4. Continuous 12-lead ECG monitoring is a reasonable alternative to serial 12-lead recordings in patients whose initial ECG is nondiagnostic. (Level of Evidence: B)" |
| Class IIb |
| "1. For patients who present within 6 h of the onset of symptoms consistent with ACS, assessment of an early marker of cardiac injury (e.g., myoglobin) in conjunction with a late marker (e.g., troponin) may be considered. (Level of Evidence: B)" |
| "2. For patients who present within 6 h of symptoms suggestive of ACS, a 2-h delta CK-MB mass in conjunction with 2-h delta troponin may be considered. (Level of Evidence: B)" |
| "3. For patients who present within 6 h of symptoms suggestive of ACS, myoglobin in conjunction with CK-MB mass or troponin when measured at baseline and 90 min may be considered. (Level of Evidence: B)" |
| "4. Measurement of B-type natriuretic peptide (BNP) or NT-pro-BNP may be considered to supplement assessment of global risk in patients with suspected ACS. (Level of Evidence: B)" |
| Class I |
| "1. Noninvasive stress testing is recommended in low-risk patients who have been free of ischemia at rest or with low-level activity and of heart failure for a minimum of 12 to 24 h. (Level of Evidence: C)" |
| "2. Noninvasive stress testing is recommended in patients at intermediate risk who have been free of ischemia at rest or with low-level activity and of heart failure for a minimum of 12 to 24 h. (Level of Evidence: C)" |
| "3. Choice of stress test is based on the resting ECG, ability to perform exercise, local expertise, and technologies available. Treadmill exercise is useful in patients able to exercise in whom the ECG is free of baseline ST segment abnormalities, bundle branch block, left ventricular hypertrophy, intraventricular conduction defect, paced rhythm, pre-excitation, and digoxin effect. (Level of Evidence: C)" |
| "4. An imaging modality should be added in patients with resting ST segment depression (≥0.10 mV), left ventricular hypertrophy, bundle branch block, intraventricular conduction defect, pre-excitation, or on digoxin treatment who are able to exercise. In patients undergoing a low level exercise test, an imaging modality can add sensitivity. (Level of Evidence: B)" |
| "5. Pharmacological stress testing with imaging is recommended when physical limitations (e.g., arthritis, amputation, severe peripheral vascular disease, severe chronic obstructive pulmonary disease, or general debility) preclude adequate exercise stress. (Level of Evidence: B)" |
| "6. Prompt angiography without noninvasive risk stratification should be performed for failure of stabilization with intensive medical treatment. (Level of Evidence: B)" |
| "7. A non invasive test (echocardiogram or radionuclide angiogram) is recommended to evaluate left ventricular function in patients with definite acute coronary syndromes who are not scheduled for coronary angiography and left ventriculography. (Level of Evidence: B)" |
References
- ↑ Lee, DS & Roe, MT (2004). Unstable angina and non-ST-elevation myocardial infarction, In Griffin & Topol Eds, Manual of Cardiovascular Medicine, 2nd ed. Lippincott Williams & Williams: Philadelphia, PA, pp 27-44. ISBN 9780781759984
- ↑ 2.0 2.1 Rizik DG, Healy S, Margulis A, Vandam D, Bakalyar D, Timmis G, Grines C, O'Neill WW, Schreiber TL. A new clinical classification for hospital prognosis of unstable angina pectoris. Am J Cardiol. 1995 May 15;75(15):993-7. PMID 7747701
- ↑ Antman EM, Cohen M, Bernink PJ, et al. The TIMI risk score for unstable angina/non-ST elevation MI: a method for prognostication and therapeutic decision making. JAMA 2000; 284: 835–42. PMID 10938172
- ↑ 4.0 4.1 Pollack CV Jr, Sites FD, Shofer FS, Sease KL, Hollander JE. Application of the TIMI risk score for unstable angina and non-ST elevation acute coronary syndrome to an unselected emergency department chest pain population. Acad Emerg Med. 2006 Jan;13(1):13-8. Epub 2005 Dec 19. PMID 16365321
- ↑ Granger CB, Goldberg RJ, Dabbous O, Pieper KS, Eagle KA, Cannon CP, Van De Werf F, Avezum A, Goodman SG, Flather MD, Fox KA; Global Registry of Acute Coronary Events Investigators. Predictors of hospital mortality in the global registry of acute coronary events. Arch Intern Med. 2003 Oct 27;163(19):2345-53. PMID 14581255
- ↑ Eagle KA, Lim MJ, Dabbous OH, Pieper KS, Goldberg RJ, Van de Werf F, Goodman SG, Granger CB, Steg PG, Gore JM, Budaj A, Avezum A, Flather MD, Fox KA; GRACE Investigators. Predictors of outcome in patients with acute coronary syndromes without persistent ST-segment elevation. Results from an international trial of 9461 patients. The PURSUIT Investigators. JAMA. 2004 Jun 9;291(22):2727-33. PMID 15187054
- ↑ 7.0 7.1 Boersma E, Pieper KS, Steyerberg EW, Wilcox RG, Chang WC, Lee KL, Akkerhuis KM, Harrington RA, Deckers JW, Armstrong PW, Lincoff AM, Califf RM, Topol EJ, Simoons ML. Predictors of outcome in patients with acute coronary syndromes without persistent ST-segment elevation. Results from an international trial of 9461 patients. The PURSUIT Investigators. Circulation. 2000 Jun 6;101(22):2557-67. PMID 10840005
- ↑ Lindahl B, Diderholm E, Lagerqvist B, et al: Mechanisms behind the prognostic value of troponin T in unstable coronary artery disease: A FRISC II substudy. J Am Coll Cardiol 2001; 38:979-986.* Lenderink T, Boersma E, Heeschen C, et al: Elevated troponin T and C-reactive protein predict impaired outcome for 4 years in patients with refractory unstable angina, and troponin T predicts benefit of treatment with abciximab in combination with PTCA. Eur Heart J 2003; 24:77-85. PMID 11583868
- ↑ Heeschen C, Hamm CW, Bruemmer J, Simoons ML, for the Chimeric c7E3 AntiPlatelet Therapy in Unstable angina REfractory to standard treatment trial (CAPTURE) Investigators: Predictive value of C-reactive protein and troponin T in patients with unstable angina: A comparative analysis. J Am Coll Cardiol 2000; 35:1535-1542. PMID 10807457
- ↑ Gibson CM, Pinto DS, Murphy SA, et al: Association of creatinine and creatinine clearance on presentation in acute myocardial infarction with subsequent mortality. J Am Coll Cardiol 2003; 42:1535-1543. PMID 14607434
- ↑ The RISC Group: Risk of myocardial infarction and death during treatment with low-dose aspirin and intravenous heparin in men with unstable coronary artery disease. Lancet 1990; 336:827-830. PMID 1976875
- ↑ 12.0 12.1 Schellings DA, Adiyaman A, Dambrink JE, Gosselink AM, Kedhi E, Roolvink V; et al. (2016). "Predictive value of NT-proBNP for 30-day mortality in patients with non-ST-elevation acute coronary syndromes: a comparison with the GRACE and TIMI risk scores". Vasc Health Risk Manag. 12: 471–476. doi:10.2147/VHRM.S117204. PMC 5123586. PMID 27920547.
- ↑ 13.0 13.1 Roy SS, Abu Azam STM, Khalequzzaman M, Ullah M, Arifur Rahman M (2018). "GRACE and TIMI risk scores in predicting the angiographic severity of non-ST elevation acute coronary syndrome". Indian Heart J. 70 Suppl 3: S250–S253. doi:10.1016/j.ihj.2018.01.026. PMC 6309119. PMID 30595268.
- ↑ Antman EM, Cohen M, Bernink PJ, et al. The TIMI risk score for unstable angina/non-ST elevation MI: a method for prognostication and therapeutic decision making. JAMA 2000; 284: 835–42. PMID 10938172
- ↑ Anderson JL, Adams CD, Antman EM, Bridges CR, Califf RM, Casey DE Jr, Chavey WE II, Fesmire FM, Hochman JS, Levin TN, Lincoff AM, Peterson ED, Theroux P, Wenger NK, Wright RS. ACC/AHA 2007 guidelines for the management of patients with unstable angina/non–ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines for the Management of Patients With Unstable Angina/Non–ST-Elevation Myocardial Infarction). Circulation 2007 116: e148 – e304. PMID 17679616
- ↑ Anderson JL, Adams CD, Antman EM, Bridges CR, Califf RM, Casey DE Jr, Chavey WE II, Fesmire FM, Hochman JS, Levin TN, Lincoff AM, Peterson ED, Theroux P, Wenger NK, Wright RS. Correction of ACC/AHA 2007 guidelines for the management of patients with unstable angina/non–ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines for the Management of Patients With Unstable Angina/Non–ST-Elevation Myocardial Infarction). J Am Coll Cardiol. 2008 Mar 4; 51(9): 974. PMID 17692738
- ↑ Eagle KA, Lim MJ, Dabbous OH, Pieper KS, Goldberg RJ, Van de Werf F, Goodman SG, Granger CB, Steg PG, Gore JM, Budaj A, Avezum A, Flather MD, Fox KA; GRACE Investigators. Predictors of outcome in patients with acute coronary syndromes without persistent ST-segment elevation. Results from an international trial of 9461 patients. The PURSUIT Investigators. JAMA. 2004 Jun 9;291(22):2727-33. PMID 15187054
- ↑ 18.0 18.1 18.2 18.3 Anderson JL, Adams CD, Antman EM; et al. (2007). "ACC/AHA 2007 guidelines for the management of patients with unstable angina/non-ST-Elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines for the Management of Patients With Unstable Angina/Non-ST-Elevation Myocardial Infarction) developed in collaboration with the American College of Emergency Physicians, the Society for Cardiovascular Angiography and Interventions, and the Society of Thoracic Surgeons endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation and the Society for Academic Emergency Medicine". JACC. 50 (7): e1–e157. PMID 17692738. Text "doi:10.1016/j.jacc.2007.02.013 " ignored (help); Unknown parameter
|month=ignored (help) - ↑ Ezra A. Amsterdam, MD, FACC; Nanette K. Wenger, MD et al.2014 AHA/ACC Guideline for the Management of Patients With Non–ST-Elevation Acute Coronary Syndromes. A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. JACC. September 2014 (ahead of print)
- ↑ 20.0 20.1 20.2 Wright RS, Anderson JL, Adams CD, Bridges CR, Casey DE, Ettinger SM; et al. (2011). "2011 ACCF/AHA focused update incorporated into the ACC/AHA 2007 Guidelines for the Management of Patients with Unstable Angina/Non-ST-Elevation Myocardial Infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines developed in collaboration with the American Academy of Family Physicians, Society for Cardiovascular Angiography and Interventions, and the Society of Thoracic Surgeons". J Am Coll Cardiol. 57 (19): e215–367. doi:10.1016/j.jacc.2011.02.011. PMID 21545940.
- CS1 maint: Explicit use of et al.
- CS1 maint: Multiple names: authors list
- Pages with citations using unnamed parameters
- Pages with citations using unsupported parameters
- Ischemic heart diseases
- Intensive care medicine
- Disease
- Patient information
- Cardiology
- Emergency medicine
- Mature chapter
- Up-To-Date
- Up-To-Date cardiology
- Best pages