Prothrombin complex concentrate
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Sheng Shi, M.D. [2]; Turky Alkathery, M.D. [3]
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Black Box Warning
|
WARNING: ARTERIAL AND VENOUS THROMBOEMBOLIC COMPLICATIONS
See full prescribing information for complete Boxed Warning.
Patients being treated with Vitamin K antagonists (VKA) therapy have underlying disease states that predispose them to thromboembolic events. Potential benefits of reversing VKA should be weighed against the potential risks of thromboembolic events, especially in patients with the history of a thromboembolic event. Resumption of anticoagulation should be carefully considered as soon as the risk of thromboembolic events outweighs the risk of acute bleeding.
|
Overview
Prothrombin complex concentrate is a Warfarin reversal agent that is FDA approved for the treatment of acute major bleeding, need for an urgent surgery/invasive procedure. There is a Black Box Warning for this drug as shown here. Common adverse reactions include headache, nausea/vomiting, hypotension, anemia..
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Urgent Reversal of Acquired Coagulation Factor Deficiency
- Indication
- acute major bleeding
- need for an urgent surgery/invasive procedure.
- Dosing Information
- For intravenous use only.
- Measurement of INR prior to treatment and close to the time of dosing is important because coagulation factors may be unstable in patients with acute major bleeding or an urgent need for surgery and other invasive procedures.
- Individualize Kcentra dosing based on the patient's current pre-dose International Normalized Ratio (INR) value, and body weight (see Table 1).
The actual potency per vial of Factors II, VII, IX and X, Proteins C and S is stated on the carton.
- Administer Vitamin K concurrently to patients receiving Kcentra. Vitamin K is administered to maintain Vitamin K-dependent clotting factor levels once the effects of Kcentra have diminished.
- The safety and effectiveness of repeat dosing have not been established and is not recommended.
- Dose ranging within pre-treatment INR groups has not been studied in randomized clinical trials of Kcentra.

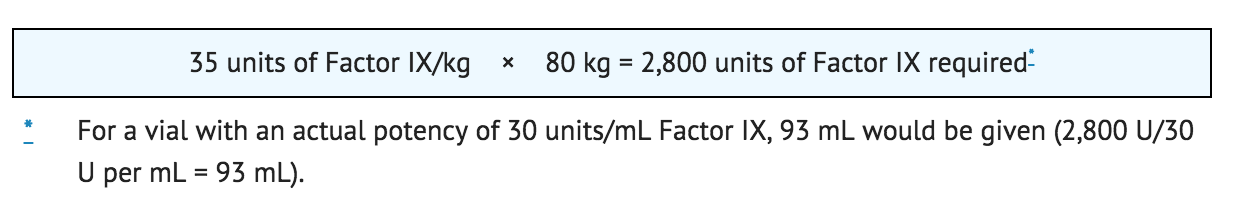
Example dosing calculation for 80 kg patient
For example, an 80 kg patient with a baseline of INR of 5.0, the dose would be 2,800 Factor IX units of Kcentra, calculated as follows based on INR range of 4–6, see Table 1:
Monitor INR and clinical response during and after treatment. In clinical trials, Kcentra decreased the INR to ≤ 1.3 within 30 minutes in most subjects. The relationship between this or other INR values and clinical hemostasis in patients has not been established.
- Preparation and Reconstitution
- Reconstitute using aseptic technique with 20 mL (500 U kit) or 40 mL (1000 U kit) of diluent provided with the kit.
- Visually inspect parenteral drug products for particulate matter and discoloration prior to administration whenever solution and container permit. Reconstituted Kcentra :* solution should be colorless, clear to slightly opalescent, and free from visible particles. Do not use solutions that are cloudy or have deposits.
- Kcentra is for single use only. Contains no preservatives. Discard partially used vials.
- The procedures provided in Table 2 are general guidelines for the preparation and reconstitution of Kcentra.
- Reconstitute at room temperature as follows:

Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information about Off-Label Guideline-Supported Use of Kcentra in adult patients.
Non–Guideline-Supported Use
There is limited information about Off-Label Non–Guideline-Supported Use of Kcentra in adult patients.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
There is limited information regarding Prothrombin complex concentrate FDA-Labeled Indications and Dosage (Pediatric) in the drug label.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information about Off-Label Guideline-Supported Use of Kcentra in pediatric patients.
Non–Guideline-Supported Use
There is limited information about Off-Label Non–Guideline-Supported Use of Kcentra in pediatric patients.
Contraindications
Kcentra is contraindicated in:
- Patients with known anaphylactic or severe systemic reactions to Kcentra or any components in Kcentra including heparin, Factors II, VII, IX, X, Proteins C and S, Antithrombin III and human albumin.
- Patients with disseminated intravascular coagulation (DIC).
- Patients with known heparin-induced thrombocytopenia (HIT). Kcentra contains heparin .
Warnings
|
WARNING: ARTERIAL AND VENOUS THROMBOEMBOLIC COMPLICATIONS
See full prescribing information for complete Boxed Warning.
Patients being treated with Vitamin K antagonists (VKA) therapy have underlying disease states that predispose them to thromboembolic events. Potential benefits of reversing VKA should be weighed against the potential risks of thromboembolic events, especially in patients with the history of a thromboembolic event. Resumption of anticoagulation should be carefully considered as soon as the risk of thromboembolic events outweighs the risk of acute bleeding.
|
Hypersensitivity Reactions
Hypersensitivity reactions including flushing, urticaria, tachycardia, anxiety, angioedema, wheezing, nausea, vomiting, hypotension, tachypnea, dyspnea, pulmonary edema, and bronchospasm have been observed with Kcentra. If severe allergic reaction or anaphylactic type reactions occur, immediately discontinue administration, and institute appropriate treatment.
Thromboembolic Risk/Complications
Both fatal and non-fatal arterial thromboembolic events (including acute myocardial infarction and arterial thrombosis), and venous thromboembolic events (including pulmonary embolism and venous thrombosis) and disseminated intravascular coagulation have been reported with Kcentra in clinical trials and post marketing surveillance. Patients being treated with VKA therapy have underlying disease states that predispose them to thromboembolic events. Reversing VKA therapy exposes patients to the thromboembolic risk of their underlying disease. Resumption of anticoagulation should be carefully considered following administration of Kcentra and Vitamin K once the risk of thromboembolic events outweighs the risk of bleeding. Thromboembolic events occurred more frequently following Kcentra compared to plasma in a randomized, plasma controlled trial in subjects requiring urgent reversal of VKA anticoagulation due to acute major bleeding, and the excess in thromboembolic events was more pronounced among subjects who had a history of prior thromboembolic event, although these differences were not statistically significant. Potential benefits of treatment with Kcentra should be weighed against the potential risks of thromboembolic events. Patients with a history of thrombotic events, myocardial infarction, cerebral vascular accident, transient ischemic attack, unstable angina pectoris, severe peripheral vascular disease, or disseminated intravascular coagulation, within the previous 3 months were excluded from participating in the plasma-controlled RCT. Kcentra may not be suitable in patients with thromboembolic events in the prior 3 months. Because of the risk of thromboembolism associated with reversal of VKA, closely monitor patients for signs and symptoms of thromboembolism during and after administration of Kcentra.
Transmissible Infectious Agents
Because Kcentra is made from human blood, it may carry a risk of transmitting infectious agents, e.g., viruses, the variant Creutzfeldt-Jakob disease (vCJD) agent, and, theoretically, the Creutzfeldt-Jakob disease agent. There is also the possibility that unknown infectious agents may be present in such products. Despite the use of two dedicated virus reduction steps in manufacturing to reduce risks, such products may still potentially transmit disease. Reports of suspected virus transmission of hepatitis A, B, C, and HIV were generally confounded by concomitant administration of blood/blood components and/or other plasma-derived products. No causal relationship to Kcentra administration was established for any of these reports since introduction of a virus filtration step in 1996. All infections thought by a physician to have been possibly transmitted by Kcentra should be reported by the physician or other healthcare provider to the CSL Behring Pharmacovigilance Department at 1-866-915-6958 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Adverse Reactions
Clinical Trials Experience
The most common adverse reactions (ARs) (frequency ≥ 2.8%) observed in subjects receiving Kcentra were headache, nausea/vomiting, hypotension, and anemia. The most serious ARs were thromboembolic events including stroke, pulmonary embolism, and deep vein thrombosis. The following serious adverse reactions are described below and/or elsewhere in the labeling:
- Hypersensitivity Reactions.
- Arterial and venous thromboembolic complications.
- Possible transmission of infectious agents.
Clinical Trials Experience
Because clinical studies are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Randomized, Plasma-Controlled Trial in Acute Major Bleeding
In a prospective, randomized, open-label, active-controlled multicenter non-inferiority trial, 212 subjects who required urgent reversal of VKA therapy due to acute major bleeding were enrolled and randomized to treatment; 103 were treated with Kcentra and 109 with plasma. Subjects with a history of a thrombotic event, myocardial infarction, cerebral vascular accident, transient ischemic attack, unstable angina pectoris, severe peripheral vascular disease, or disseminated intravascular coagulation, within the previous 3 months were excluded from participating. Subjects ranged in age from 26 years to 96 years.
Randomized, Plasma-Controlled Trial in Urgent Surgery/Invasive Procedures
In a prospective, randomized, open-label, active-controlled, multicenter non-inferiority trial, 176 subjects who required urgent reversal of VKA therapy due to the need for an urgent surgical or urgent invasive procedure were enrolled; 88 were treated with Kcentra and 88 with plasma. Subjects ranged in age from 27 years to 94 years. Adverse reactions are summarized for Kcentra and plasma in the Acute Major Bleeding and Urgent Surgery/Invasive Procedures RCTs (see Table 3). Adverse Reactions are defined as adverse events that began during or within 72 hours of test product infusion plus adverse events considered possibly/probably related or related to study treatment according to the investigator, sponsor, or the blinded safety adjudication board (SAB), and with at least a 1.3‐fold difference between treatments.

Serious adverse reactions in subjects receiving Kcentra in both RCTs included ischemic cerebrovascular accident (stroke), DVT, thrombosis, and venous insufficiency. Serious adverse reactions in both RCTs for plasma included myocardial ischemia, myocardial infarction, fluid overload, embolic cerebral infarction, pulmonary edema, respiratory failure, and DVT. There were a total of 10 subjects (9.7%) who died in the Kcentra group (1 additional death occurred on day 46 just after completion of the study reporting period) and 5 (4.6%) who died in the plasma group in the plasma-controlled RCT in acute major bleeding. The 95% confidence interval for the Kcentra minus plasma between-group difference in deaths ranged from -2.7% to 13.5%. From the plasma-controlled RCT in urgent surgery/invasive procedures, there were a total of 3 subjects (3.4%) who died in the Kcentra group (1 additional death occurred on day 48 after completion of the study reporting period) and 8 (9.1%) who died in the Plasma group. The 95% confidence interval for the Kcentra minus plasma between-group difference in deaths in this trial ranged from -14.6% to 2.7%. One death in the Kcentra group in the RCT in Acute Major Bleeding and one death in the plasma group in the RCT in urgent surgery/invasive procedures were considered possibly related to study treatment according to an assessment of masked data by an independent safety adjudication board. No factors common to all deaths were identified, except for the frequent findings of a high comorbidity burden, advanced age, and death after being placed on comfort care. Although, a greater proportion of subjects in the RCT in acute major bleeding than in the RCT in surgery/invasive procedure received the highest two recommended doses of Kcentra because more subjects in the trial in acute major bleeding had a baseline INR in the ranges of 4–6 and > 6.0, an analysis of deaths and factor levels in subjects with major bleeding revealed that subjects who died had similar median factor levels to subjects that did not die. Additionally, outliers with supraphysiologic factor levels did not have a mortality rate out of proportion to the overall population.
Fluid Overload
There were 9 subjects (4.7%, all non-related by investigator assessment) in the Kcentra group who experienced fluid overload in the plasma-controlled RCTs in acute major bleeding and urgent surgery/invasive procedures and 25 (12.7%, 13 events related by investigator assessment) who had fluid overload in the plasma group. The 95% confidence interval for the Kcentra minus Plasma between-group difference in fluid overload event incidence ranged from -14.1% to -2.0%. Subgroup analyses of the RCTs in acute major bleeding and urgent surgery/invasive procedures according to whether subjects with fluid overload events had a prior history of congestive heart failure are presented in Table 4.

Thromboembolic Events
In RCTs, there were 13 subjects (6.8%) in the Kcentra group who experienced possible thromboembolic events (TEEs) and 14 (7.1%) who had TEEs in the plasma group. The incidence of thromboembolic (TE) adverse reactions assessed as at least possibly related to study treatment by the Investigator or, in the case of serious thromboembolic events, the blinded safety adjudication board (SAB) was 9 (4.7%) in the Kcentra group and 7 (3.6%) in the plasma group. When also considering the events which began during or within 72 hours of test product infusion, the incidence was 9 (4.7%) in the Kcentra group and 8 (4.1%) in the plasma group. TE events observed in the acute major bleeding and the urgent surgery/invasive procedures RCTs are shown in Table 5.

Subgroup analyses of the RCTs according to whether subjects with thromboembolic events had a prior history of a thromboembolic event are presented in Table 6.

The European Bleeding and Surgical Study: In a prospective, open label, single-arm, multicenter safety and efficacy trial, 17 subjects who required urgent reversal of VKA due to acute bleeding were enrolled and 26 subjects who required urgent reversal of Vitamin K antagonist due to the need for an urgent surgical/invasive procedure were enrolled, all were treated with Kcentra. Subjects ranged in age from 22 years to 85 years. Serious adverse reactions considered possibly related to Kcentra included a suspected pulmonary embolism which occurred in one subject following a second dose of Kcentra. A single non-fatal TE event occurred in another Kcentra-treated subject in that trial.
Postmarketing Experience
No adverse reactions other than those addressed in Warnings and Adverse Reactions have been observed in the postmarketing use of Kcentra outside the US since 1996.
Drug Interactions
There is no FDA guidance on the use of Kcentra with respect to specific drug interactions.
Use in Specific Populations
Pregnancy
Pregnancy Category (FDA): C
Pregnancy Category C. Animal reproduction studies have not been conducted with Kcentra. It is also not known whether Kcentra can cause fetal harm when administered to a pregnant woman or can affect reproduction capacity. Kcentra should be prescribed for a pregnant woman only if clearly needed.
Pregnancy Category (AUS):
There is no FDA guidance on the use of Kcentra with respect to specific gender populations.
Labor and Delivery
Kcentra has not been studied for use during labor and delivery. Safety and effectiveness in labor and delivery have not been established.
Nursing Mothers
It is not known whether Kcentra is excreted in human milk. Because many drugs are excreted in human milk, use Kcentra only if clearly needed when treating a nursing woman.
Pediatric Use
The safety and efficacy of Kcentra in the pediatric population has not been studied.
Geriatic Use
Of the total number of subjects (431) with acute major bleeding or with the need for an urgent surgery/invasive procedure treated to reverse VKA anticoagulation in three clinical studies, 66% were 65 years old or greater and 39% were 75 years old or greater. There were no clinically significant differences between the safety profile of Kcentra and plasma in any age group.
Gender
There is no FDA guidance on the use of Kcentra with respect to specific gender populations.
Race
There is no FDA guidance on the use of Kcentra with respect to specific racial populations
Renal Impairment
There is no FDA guidance on the use of Kcentra with respect to specific renal impairment.
Hepatic Impairment
There is no FDA guidance on the use of Kcentra with respect to specific hepatic impairment.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Kcentra in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance on the use of Kcentra with respect to speciafic immunocompromised patients.
Congenital Factor Deficiencies
Kcentra has not been studied in patients with congenital factor deficiencies.
Administration and Monitoring
Administration
- Do not mix Kcentra with other medicinal products; administer through a separate infusion line.
- Use aseptic technique when administering Kcentra.
- Administer at room temperature.
- Administer by intravenous infusion at a rate of 0.12 mL/kg/min (~3 units/kg/min), up to a maximum rate of 8.4 mL/min (~210 units/min).
- No blood should enter the syringe, as there is a possibility of fibrin clot formation.
Monitoring
- Monitor INR and clinical response during and after treatment
- Because of the risk of thromboembolism associated with reversal of VKA, closely monitor patients for signs and symptoms of thromboembolism during and after administration of Kcentra.
IV Compatibility
There is limited information regarding the compatibility of Prothrombin complex concentrate and IV administrations.
Overdosage
There is limited information regarding Prothrombin complex concentrate overdosage. If you suspect drug poisoning or overdose, please contact the National Poison Help hotline (1-800-222-1222) immediately.
Pharmacology
Prothrombin complex concentrate
| |
| Combination of | |
| Factor II | Blood clotting factor |
| Factor VII | Blood clotting factor |
| Factor IX | Blood clotting factor |
| Factor X | Blood clotting factor |
| Identifiers | |
| CAS number | |
| ATC code | B02 |
| PubChem | ? |
| Therapeutic considerations | |
| Pregnancy cat. |
? |
| Legal status |
Template:Unicode Prescription only |
| Routes | Injection |
Mechanism of Action
Kcentra contains the Vitamin K-dependent coagulation Factors II (FII), VII (FVII), IX (FIX), and X (FX), together known as the Prothrombin Complex, and the antithrombotic Protein C and Protein S. A dose-dependent acquired deficiency of the Vitamin K-dependent coagulation factors occurs during Vitamin K antagonist treatment. Vitamin K antagonists exert anticoagulant effects by blocking carboxylation of glutamic acid residues of the Vitamin K-dependent coagulation factors during hepatic synthesis, lowering both factor synthesis and function. The administration of Kcentra rapidly increases plasma levels of the Vitamin K-dependent coagulation Factors II, VII, IX, and X as well as the antithrombotic Proteins C and S.
- Coagulation Factor II
- Factor II (prothrombin) is converted to thrombin by activated FX (FXa) in the presence of Ca2+, FV, and phospholipids.
- Coagulation Factor VII
- Factor VII (proconvertin) is converted to the activated form (FVIIa) by splitting of an internal peptide link. The FVIIa-TF complex activates Factor IX and initiates the primary coagulation
pathway by activating FX in the presence of phospholipids and calcium ions.
- Coagulation Factor IX
- Factor IX (antihemophilic globulin B, or Christmas factor) is activated by the FVIIa-TF complex and by FXIa. Factor IXa in the presence of FVIIIa activates FX to FXa.
- Coagulation Factor X
- Factor X (Stuart-Prower factor) activation involves the cleavage of a peptide bond by the FVIIIa-Factor IXa complex or the TF-FVIIa complex. Factor Xa forms a complex with activated FV (FVa) that converts prothrombin to thrombin in the presence of phospholipids and calcium ions.
- Protein S
Structure
Kcentra is a purified, heat-treated, nanofiltered and lyophilized non-activated four-factor Prothrombin Complex Concentrate (Human) prepared from human U.S. Source Plasma (21 CFR 640.60). It contains the Vitamin K dependent Coagulation Factors II, VII, IX and X, and the antithrombotic Proteins C and S. Factor IX is the lead factor for the potency of the preparation as stated on the vial label. The excipients are human antithrombin III, heparin, human albumin, sodium chloride, and sodium citrate. Kcentra is sterile, pyrogen-free, and does not contain preservatives. The product contents are shown in Table 7 and listed as ranges for the blood coagulation factors.

All plasma used in the manufacture of Kcentra is obtained from US donors and is tested using serological assays for hepatitis B surface antigen and antibodies to HIV-1/2 and HCV. The plasma is tested with Nucleic Acid Testing (NAT) for HCV, HIV-1, HAV, and HBV, and found to be non-reactive (negative), and the plasma is also tested by NAT for human parvovirus B19 (B19V) in order to exclude donations with high titers. The limit for B19V in the fractionation pool is set not to exceed 104 units of B19V DNA per mL. Only plasma that passed virus screening is used for production. The Kcentra manufacturing process includes various steps, which contribute towards the reduction/ inactivation of viruses. Kcentra is manufactured from cryo-depleted plasma that is adsorbed via ion exchange chromatography, heat treated in aqueous solution for 10 hours at 60°C, precipitated, adsorbed to calcium phosphate, virus filtered, and lyophilized. These manufacturing steps were independently validated in a series of in-vitro experiments for their virus inactivation / reduction capacity for both enveloped and non-enveloped viruses. Table 8 shows the virus clearance during the manufacturing process for Kcentra, expressed as the mean log10 reduction factor.

Pharmacodynamics
In the plasma-controlled RCT in acute major bleeding, the INR was determined at varying time points after the start or end of infusion, depending upon study design. The median INR was above 3.0 prior to the infusion and dropped to a median value of 1.20 by the 30 minute time point after start of Kcentra infusion. By contrast, the median value for plasma was 2.4 at 30 minutes after the start of infusion. The INR differences between Kcentra and plasma were statistically significant in randomized plasma-controlled trial in bleeding up to 12 hours after start of infusion [see Table 9]. The relationship between these or other INR values and clinical hemostasis in patients has not been established.

Pharmacokinetics
Fifteen healthy subjects received 50 units/kg of Kcentra. No subjects were receiving VKA therapy or were experiencing acute bleeding. A single intravenous Kcentra infusion produced a rapid and sustained increase in plasma concentration of Factors II, VII, IX and X as well as Proteins C and S. The PK analysis [see Table 10] shows that factor II had the longest half-life (59.7 hours) and factor VII the shortest (4.2 hours) in healthy subjects. PK parameters obtained from data derived from the study of healthy subjects may not be directly applicable to patients with INR elevation due to VKA anticoagulation therapy.

The mean in vivo recovery (IVR) of infused factors was calculated in subjects who received Kcentra. The IVR is the increase in measurable factor levels in plasma (units/dL) that may be expected following an infusion of factors (units/kg) administered as a dose of Kcentra. The in vivo recovery ranged from 1.15 (Factor IX) to 2.81 (Protein S) [see Table 11].

Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility
Long-term studies in animals to evaluate the carcinogenic potential of Kcentra, or studies to determine the effects of Kcentra on genotoxicity or fertility have not been performed. An assessment of the carcinogenic potential of Kcentra was completed and suggests minimal carcinogenic risk from product use.
Clinical Studies
Acute Major Bleeding RCT: The efficacy of Kcentra has been evaluated in a prospective, open-label, (blinded assessor), active-controlled, non-inferiority, multicenter RCT in subjects who had been treated with VKA therapy and who required urgent replacement of their Vitamin K-dependent clotting factors to treat acute major bleeding. A total of 216 subjects with acquired coagulation factor deficiency due to oral Vitamin K antagonist therapy were randomized to a single dose of Kcentra or plasma. Two hundred twelve (212) subjects received Kcentra or plasma for acute major bleeding in the setting of a baseline INR ≥ 2.0 and recent use of a VKA anticoagulant. The doses of Kcentra (25 units/kg, 35 units/kg, or 50 units/kg) based on nominal Factor IX content and plasma (10 mL/kg, 12 mL/kg, or 15 mL/kg) were calculated according to the subject's baseline INR (2–< 4, 4–6, > 6, respectively). The observation period lasted for 90 days after the infusion of Kcentra or plasma. The modified efficacy (ITT-E) population for Kcentra included 98 subjects and for plasma included 104 subjects. Additionally, intravenous Vitamin K was administered.
The efficacy endpoint was hemostatic efficacy for the time period from the start of infusion of Kcentra or plasma until 24 hours. Efficacy was adjudicated as "effective" or "not effective" by a blinded, independent Endpoint Adjudication Board for all subjects who received study product. Criteria for effective hemostasis were based upon standard clinical assessments including vital signs, hemoglobin measurements, and CT assessments at pre-defined time points, as relevant to the type of bleeding (i.e., gastrointestinal, intracranial hemorrhage, visible, musculoskeletal, etc.). The proportion of subjects with effective hemostasis was 72.4% in the Kcentra group and 65.4% in the plasma group. The lower limit of the 95% confidence interval (CI) for the difference in proportions of Kcentra minus plasma was -5.8%, which exceeded -10% and thereby demonstrated the non-inferiority of Kcentra versus plasma (the study's primary objective) [see Table 12]. Because the lower limit of the CI was not greater than zero, the prospectively defined criterion for superiority of Kcentra for hemostatic efficacy (a secondary objective) was not met.

Results of a post-hoc analysis of hemostatic efficacy stratified by actual dose of Kcentra or plasma administered in the acute major bleeding RCT are presented in Table 13.

An additional endpoint was the reduction of INR to ≤ 1.3 at 30 minutes after the end of infusion of Kcentra or plasma for all subjects that received study product. The proportion of subjects with this decrease in INR was 62.2% in the Kcentra group and 9.6% in the plasma group. The 95% confidence interval for the difference in proportions of Kcentra minus plasma was 39.4% to 65.9%. The lower limit of the 95% CI of 39.4% demonstrated superiority of Kcentra versus plasma for this endpoint [see Table 14].

Urgent Surgery/Invasive Procedure RCT: The efficacy of Kcentra has been evaluated in a prospective, open-label, active-controlled, non-inferiority, multicenter RCT in subjects who had been treated with VKA therapy and who required urgent replacement of their Vitamin K-dependent clotting factors because of their need for an urgent surgery/ invasive procedure. A total of 181 subjects with acquired coagulation factor deficiency due to oral Vitamin K antagonist therapy were randomized to a single dose of Kcentra or plasma. One hundred seventy-six (176) subjects received Kcentra or plasma because of their need for an urgent surgery/ invasive procedure in the setting of a baseline INR ≥ 2.0 and recent use of a VKA anticoagulant. The doses of Kcentra (25 units/kg, 35 units/kg, or 50 units/kg) based on nominal Factor IX content and plasma (10 mL/kg, 12 mL/kg, or 15 mL/kg) were calculated according to the subject's baseline INR (2–< 4, 4–6, > 6, respectively). The observation period lasted for 90 days after the infusion of Kcentra or plasma. The modified efficacy (ITT-E) population for Kcentra included 87 subjects and for plasma included 81 subjects. Additionally, oral or intravenous Vitamin K was administered.
The efficacy endpoint was hemostatic efficacy for the time period from the start of infusion of Kcentra or plasma until the end of the urgent surgery/invasive procedure. Criteria for effective hemostasiswere based upon the difference between predicted and actual blood losses, subjective hemostasisrating, and the need for additional blood products containing coagulation factors. The proportion of subjects with effective hemostasiswas 89.7% in the Kcentra group and 75.3% in the plasma group. The lower limit of the 95% confidence interval (CI) for the difference in proportions of Kcentra minus plasma was 2.8%, which exceeded -10% and thereby demonstrated the non-inferiority of Kcentra versus plasma (the study's primary objective) [see Table 15]. Because the lower limit of the CI was greater than 0, the prospectively defined criterion for superiority of Kcentra for hemostatic efficacy (a secondary objective) was also met.

Results of a post-hoc analysis of hemostatic efficacy stratified by actual dose of Kcentra or plasma administered in the urgent surgery/invasive procedure RCT are presented in Table 16.

An additional endpoint was the reduction of INR to ≤ 1.3 at 30 minutes after the end of infusion of Kcentra or plasma for all subjects that received study product. The proportion of subjects with this decrease in INR was 55.2% in the Kcentra group and 9.9% in the plasma group. The 95% confidence interval for the difference in proportions of Kcentra minus plasma was 31.9% to 56.4%. The lower limit of the 95% CI of 31.9% demonstrated superiority of Kcentra versus plasma for this endpoint [see Table 17]. The relationship between a decrease in INR to less than or equal to 1.3 and clinical hemostatic efficacy has not been established.

The European Bleeding and Surgical Study was an open-label, single-arm, multicenter study.1 Forty-three (43) subjects who were receiving VKA were treated with Kcentra, because they either (1) required a surgical or an invasive diagnostic intervention (26 subjects), or (2) experienced an acute bleeding event (17 subjects). The dose of Kcentra (25 units/kg, 35 units/kg, or 50 units/kg) based on nominal Factor IX content was calculated according to the subject's baseline INR value (2–< 4, 4–6, > 6). The endpoint was the decrease of the INR to ≤ 1.3 within 30 minutes after end of Kcentra infusion in subjects who received any portion of study product. Of the 17 evaluable subjects receiving Kcentra for acute bleeding, 16 subjects (94%) experienced a decrease in INR to ≤ 1.3 within 30 minutes after the end of the Kcentra infusion. In RCTs, levels of Coagulation Factors II, VII, IX, X, and Antithrombotic Proteins C and S were measured after the infusion of Kcentra or plasma and the results were similar for subjects with acute major bleeding or subjects requiring an urgent surgery or invasive procedure. In the plasma-controlled RCT in acute major bleeding, the mean duration of Kcentra infusion was 24 minutes (± 32 minutes) and the mean duration of infusion for plasma was 169 minutes (± 143 minutes). The mean infusion volume of Kcentra was 105 mL ± 37 mL and the mean infusion volume of plasma was 865 mL ± 269 mL. In the plasma-controlled RCT for patients needing urgent surgery/invasive procedures, the mean duration of Kcentra infusion was 21 minutes (± 14 minutes) and the mean duration of infusion for plasma was 141 minutes (± 113 minutes). The mean infusion volume of Kcentra was 90 mL ± 32 mL and the mean infusion volume of plasma was 819 mL ± 231 mL. The increase in mean factor levels over time following Kcentra and plasma administration in the plasma-controlled RCT in acute major bleeding is shown in Figure 9 below (the mean factor levels over time following Kcentra and plasma administration in the plasma-controlled RCT for patients needing urgent surgery/invasive procedures are not shown, but showed similar profiles). Levels of some factors continued to increase at later time points, consistent with the effect of concomitant Vitamin K treatment. Formal pharmacokinetic parameters were not derived because of the effect of Vitamin K on factor levels at time points required for pharmacokinetic profiling.

How Supplied
Kcentra is supplied in a single-use vial. The actual units of potency of all coagulation factors (Factors II, VII, IX and X), Proteins C and S in units are stated on each Kcentra carton. The Kcentra packaging components are not made with natural rubber latex. Each kit consists of the following:

Storage
- Prior to Reconstitution
- Kcentra is for single use only. Contains no preservatives.
- Store Kcentra between 2–25°C (36–77°F), this includes room temperature, not to exceed 25°C (77°F). Do not freeze.
- Kcentra is stable for 36 months from the date of manufacture, up to the expiration date on the carton and vial labels.
- Do not use Kcentra beyond the expiration date on the vial label and carton.
- Store the vial in the original carton to protect it from light.
- After Reconstitution
- The product must be used within 4 hours following reconstitution. Reconstituted product can be stored at 2–25°C. If cooled, the solution should be warmed to 20–25°C prior to administration. Do not freeze the reconstituted product. Discard partially used vials.
Images
Drug Images
{{#ask: Page Name::Prothrombin complex concentrate |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
{{#ask: Label Page::Prothrombin complex concentrate |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
- Inform patients of the signs and symptoms of allergic hypersensitivity reactions, such as urticaria, rash, tightness of the chest, wheezing, hypotension and/or anaphylaxis experienced during or after injection of Kcentra.
- Inform patients of signs and symptoms of thrombosis, such as limb or abdomen swelling and/or pain, chest pain or pressure, shortness of breath, loss of sensation or motor power, altered consciousness, vision, or speech.
- Inform patients that, because Kcentra is made from human blood, it may carry a risk of transmitting infectious agents, e.g., viruses, the variant Creutzfeldt-Jakob disease (vCJD) agent, and theoretically, the Creutzfeldt-Jakob disease (CJD) agent.
Precautions with Alcohol
Alcohol-Kcentra interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
Beriplex, Octaplex, Kcentra, Cofact
Look-Alike Drug Names
There is limited information regarding Prothrombin complex concentrate Look-Alike Drug Names in the drug label.
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
{{#subobject:
|Label Page=Prothrombin complex concentrate |Label Name=Kcentra_label_01.jpg
}}
{{#subobject:
|Label Page=Prothrombin complex concentrate |Label Name=Kcentra_label_02.jpg
}}
{{#subobject:
|Label Page=Prothrombin complex concentrate |Label Name=Kcentra_panel_01.jpg
}}