Portal hypertension natural history, complications and prognosis
|
Portal Hypertension Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Portal hypertension natural history, complications and prognosis On the Web |
|
American Roentgen Ray Society Images of Portal hypertension natural history, complications and prognosis |
|
FDA on Portal hypertension natural history, complications and prognosis |
|
CDC on Portal hypertension natural history, complications and prognosis |
|
Portal hypertension natural history, complications and prognosis in the news |
|
Blogs on Portal hypertension natural history, complications and prognosis |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Eiman Ghaffarpasand, M.D. [2]
Overview
Portal hypertension is increased hepatic venous pressure gradient (HVPG) above 5 mmHg. The symptoms of portal hypertension usually develop in the third to fourth decades of life, and generally start with symptoms such as esophageal varices, caput medusae, spider angioma, and splenomegaly. Esophageal varices typically developes at the rate of 5-15% per year in cirrhosis patients. Most of the cirrhotic patients will develop the varices, atleast once during the lifetime. Approximately 60% of patients with cirrhosis develop ascites in 10 years. 10% of hospitalized patients with cirrhosis will involve in spontaneous bacterial peritonitis (SBP). If left untreated, 20-40% of patients with SBP may progress to death. The presence of variceal bleeding, spontaneous bacterial peritonitis, and hepatorenal syndrome are associated with a particularly poor prognosis among patients with portal hypertension. They are the leading causes of death among patients with portal hypertension.
Natural History, Complications, and Prognosis
- Portal hypertension is increased hepatic venous pressure gradient (HVPG) above 5 mmHg.
- 90% of the cases are due to hepatic cirrhosis.[1]
- The stage of cirrhosis severity is determined base on Child-Pugh-Turcotte (CPT) scoring system, including Child A if 5-6 points, Child B if 7-9 points, and Child C if 10-15 points.
| Parameter | Points | ||
|---|---|---|---|
| 1 | 2 | 3 | |
| Ascites | None | Mild/Moderate | Tense |
| Hepatic encephalopathy | None | Grade 1-2 | Grade 3-4 |
| Bilirubin μMol/L (mg/dL) | <34.2 (<2) | 34.2–51.3 (2-3) | >51.3 (>3) |
| Albumin g/L (g/dL) | >35 (>3.5) | 28–35 (2.8–3.5) | <28 (<2.8) |
| PT (Sec) or INR |
<4 | 4–6 | >6 |
| <1.7 | 1.7–2.3 | >2.3 | |
Natural History
- The symptoms of portal hypertension usually develop in the third to fourth decades of life, and generally start with symptoms such as esophageal varices, caput medusae, spider angioma, and splenomegaly.
- The hepatic vein pressure gradient (HVPG) threshold for portal hypertension to become clinically symptomatic is 10-12mm Hg.[2]
- Esophageal varices occur when the HVPG reaches 10 mmHg. 40% of Child A and 85% of Child C cirrhosis may progress to esophageal varices.[3]
- Esophageal varices typically developes at the rate of 5-15% per year in cirrhosis patients.Most of the cirrhotic patients will develop the varices, atleast once during the lifetime.[1]
- Esophageal varices enlarge and progress at the rate of 8% per year.[4] The varices bleeds at the rate of 5-15% per year.[5]
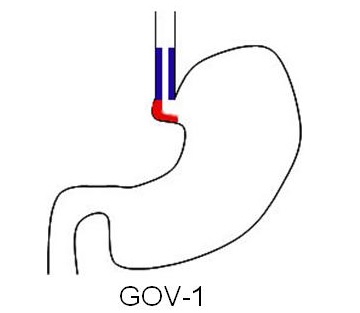 | 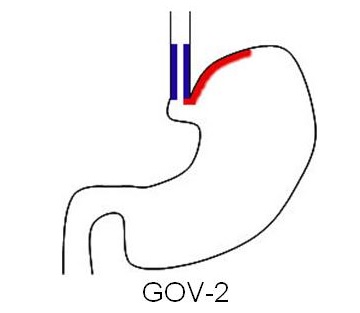 | ||||||||||||||||||||||||||||||||||
| Gastroesophageal varices type 1 Extend along the lesser curvature | Gastroesophageal varices type 2 Extend along the fundus | ||||||||||||||||||||||||||||||||||
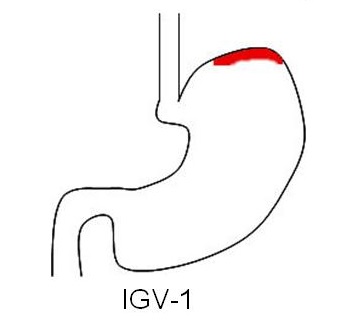 | 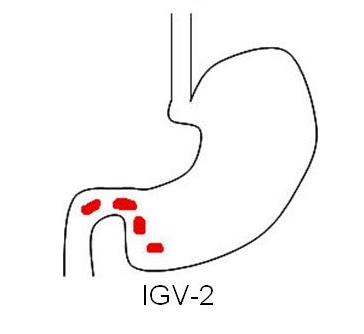 | ||||||||||||||||||||||||||||||||||
| Isolated gastric varices type 1 Located in the fundus and tend to be tortuous and complex | Isolated gastric varices Located in the body, antrum, or around the pylorus | ||||||||||||||||||||||||||||||||||
- Approximately 60% of patients with cirrhosis develop ascites in 10 years.[6]
- At least 1500 cc ascites is necessary to become identifiable through physical exam. The severe increase in intraabdominal pressure may lead to respiratory problems and/or abdominal hernias.[7]
- Based on grade of cirrhosis, international ascites club presented a grading system.[8]
| Grade | Definition |
|---|---|
| Grade 1 | Mild ascites only detectable by ultrasound |
| Grade 2 | Moderate ascites evident by moderate symmetrical distension of abdomen |
| Grade 3 | Large or gross ascites with marked abdominal distension |
- 10% of hospitalized patients with cirrhosis will involve in spontaneous bacterial peritonitis (SBP).[9]
- If left untreated, 20-40% of patients with SBP may progress to death.[10]
- Incidence of hepatorenal syndrome in cirrhotic patients is 20% in 1 year and 40% in 5 years period.[11]
- If left untreated, 100% of patients with type 1 hepatorenal syndrome may progress to death.[12]
- If left untreated, most of the patients with portal hypertension and cirrhosis may progress to hepatic encephalopathy.
| West Haven Criteria hepatic encephalopathy grading | |||||||||||||||||||||||||||||||||||
| Grade 1 | Grade 2 | Grade 3 | Grade 4 | ||||||||||||||||||||||||||||||||
| •Mild loss of consciousness •Euphoria or anxiety • Lowered attention span •Impaired performance of addition | •Lethargy or apathy •Minimal disorientation to time and place •Subtle personality change •Inappropriate behavior •Impaired performance of subtraction | •Somnolence to semi-stupor, but responsive to verbal stimuli •Confusion •Gross disorientation | •Coma (unresponsive to verbal or noxious stimuli) | ||||||||||||||||||||||||||||||||
Complications
- Common complications of portal hypertension include:[14]
Prognosis
- The presence of variceal bleeding, spontaneous bacterial peritonitis, and hepatorenal syndrome are associated with a particularly poor prognosis among patients with portal hypertension. They are the leading causes of death among patients with portal hypertension.
- When esophageal varices bleed the average rate of 6-week mortality become ≥ 20%, despite improved therapies.[15]
- When ascites occurs the 2-year mortality rate become 50%, without liver transplantation.[16]
- When SBP occurs the mortality rate of 20-40% is expected.[10]
- Prognosis is generally very poor in type 1 hepatorenal syndrome, all of them would die despite appropriate treatments.[12]
- General prognosis in cirrhotic patients is as follows:
| HVPG of 10 mmHg | • Gastroesophageal varices • Hepatocellular carcinoma • Decompensation after hepatocellular carcinoma resection | ||||||||||||||||||||||||||||||||||||||
| Compensated cirrhosis | HVPG of 12 mmHg | • Variceal bleeding | |||||||||||||||||||||||||||||||||||||
| HVPG of 16 mmHg | • First decompensation after varices • Mortality | ||||||||||||||||||||||||||||||||||||||
| Prognostic significance of HVPG in cirrhotic patients | |||||||||||||||||||||||||||||||||||||||
| HVPG of 16 mmHg | • Variceal rebleeding • Mortality | ||||||||||||||||||||||||||||||||||||||
| HVPG of 20 mmHg | • Uncontrollable active variceal bleeding • Low 1-year survival | ||||||||||||||||||||||||||||||||||||||
| Decompensated cirrhosis | |||||||||||||||||||||||||||||||||||||||
| HVPG of 22 mmHg | • Mortality in alcoholic cirrhosis and acute alcoholic hepatitis | ||||||||||||||||||||||||||||||||||||||
| HVPG of 30 mmHg | • Spontaneous bacterial peritonitis (SBP) | ||||||||||||||||||||||||||||||||||||||
References
- ↑ 1.0 1.1 Al-Busafi, Said A.; McNabb-Baltar, Julia; Farag, Amanda; Hilzenrat, Nir (2012). "Clinical Manifestations of Portal Hypertension". International Journal of Hepatology. 2012: 1–10. doi:10.1155/2012/203794. ISSN 2090-3448.
- ↑ Groszmann, Roberto J.; Garcia-Tsao, Guadalupe; Bosch, Jaime; Grace, Norman D.; Burroughs, Andrew K.; Planas, Ramon; Escorsell, Angels; Garcia-Pagan, Juan Carlos; Patch, David; Matloff, Daniel S.; Gao, Hong; Makuch, Robert (2005). "Beta-Blockers to Prevent Gastroesophageal Varices in Patients with Cirrhosis". New England Journal of Medicine. 353 (21): 2254–2261. doi:10.1056/NEJMoa044456. ISSN 0028-4793.
- ↑ Garcia-Tsao, Guadalupe; Groszmann, Roberto J.; Fisher, Rosemarie L.; Conn, Harold O.; Atterbury, Colin E.; Glickman, Morton (1985). "Portal pressure, presence of gastroesophageal varices and variceal bleeding". Hepatology. 5 (3): 419–424. doi:10.1002/hep.1840050313. ISSN 0270-9139.
- ↑ Merli, Manuela; Nicolini, Giorgia; Angeloni, Stefania; Rinaldi, Vittorio; De Santis, Adriano; Merkel, Carlo; Attili, Adolfo Francesco; Riggio, Oliviero (2003). "Incidence and natural history of small esophageal varices in cirrhotic patients". Journal of Hepatology. 38 (3): 266–272. doi:10.1016/S0168-8278(02)00420-8. ISSN 0168-8278.
- ↑ "Prediction of the First Variceal Hemorrhage in Patients with Cirrhosis of the Liver and Esophageal Varices". New England Journal of Medicine. 319 (15): 983–989. 1988. doi:10.1056/NEJM198810133191505. ISSN 0028-4793.
- ↑ Ginés, Pere; Quintero, Enrique; Arroyo, Vicente; Terés, Josep; Bruguera, Miguel; Rimola, Antoni; Caballería, Joan; Rodés, Joan; Rozman, Ciril (1987). "Compensated cirrhosis: Natural history and prognostic factors". Hepatology. 7 (1): 122–128. doi:10.1002/hep.1840070124. ISSN 0270-9139.
- ↑ Cárdenas, Andrés; Arroyo, Vicente (2003). "Mechanisms of water and sodium retention in cirrhosis and the pathogenesis of ascites". Best Practice & Research Clinical Endocrinology & Metabolism. 17 (4): 607–622. doi:10.1016/S1521-690X(03)00052-6. ISSN 1521-690X.
- ↑ Moore KP, Wong F, Gines P, Bernardi M, Ochs A, Salerno F, Angeli P, Porayko M, Moreau R, Garcia-Tsao G, Jimenez W, Planas R, Arroyo V (2003). "The management of ascites in cirrhosis: report on the consensus conference of the International Ascites Club". Hepatology. 38 (1): 258–66. doi:10.1053/jhep.2003.50315. PMID 12830009.
- ↑ Nousbaum, Jean-Baptiste; Cadranel, Jean-François; Nahon, Pierre; Khac, Eric Nguyen; Moreau, Richard; Thévenot, Thierry; Silvain, Christine; Bureau, Christophe; Nouel, Olivier; Pilette, Christophe; Paupard, Thierry; Vanbiervliet, Geoffroy; Oberti, Frédéric; Davion, Thierry; Jouannaud, Vincent; Roche, Bruno; Bernard, Pierre-Henri; Beaulieu, Sandrine; Danne, Odile; Thabut, Dominique; Chagneau-Derrode, Carinne; de Lédinghen, Victor; Mathurin, Philippe; Pauwels, Arnaud; Bronowicki, Jean-Pierre; Habersetzer, François; Abergel, Armand; Audigier, Jean-Christian; Sapey, Thierry; Grangé, Jean-Didier; Tran, Albert (2007). "Diagnostic accuracy of the Multistix 8 SG reagent strip in diagnosis of spontaneous bacterial peritonitis". Hepatology. 45 (5): 1275–1281. doi:10.1002/hep.21588. ISSN 0270-9139.
- ↑ 10.0 10.1 Tandon P, Garcia-Tsao G (2008). "Bacterial infections, sepsis, and multiorgan failure in cirrhosis". Semin. Liver Dis. 28 (1): 26–42. doi:10.1055/s-2008-1040319. PMID 18293275.
- ↑ Ginès A, Escorsell A, Ginès P, Saló J, Jiménez W, Inglada L, Navasa M, Clària J, Rimola A, Arroyo V (1993). "Incidence, predictive factors, and prognosis of the hepatorenal syndrome in cirrhosis with ascites". Gastroenterology. 105 (1): 229–36. PMID 8514039.
- ↑ 12.0 12.1 Salerno, F.; Gerbes, A.; Gines, P.; Wong, F.; Arroyo, V. (2008). "Diagnosis, prevention and treatment of hepatorenal syndrome in cirrhosis". Postgraduate Medical Journal. 84 (998): 662–670. doi:10.1136/gut.2006.107789. ISSN 0032-5473.
- ↑ Ferenci P, Lockwood A, Mullen K, Tarter R, Weissenborn K, Blei AT (2002). "Hepatic encephalopathy--definition, nomenclature, diagnosis, and quantification: final report of the working party at the 11th World Congresses of Gastroenterology, Vienna, 1998". Hepatology. 35 (3): 716–21. doi:10.1053/jhep.2002.31250. PMID 11870389.
- ↑ Blei AT (2007). "Portal hypertension and its complications". Curr. Opin. Gastroenterol. 23 (3): 275–82. doi:10.1097/MOG.0b013e3280b0841f. PMID 17414843.
- ↑ D'Amico, G (2003). "Upper digestive bleeding in cirrhosis. Post-therapeutic outcome and prognostic indicators". Hepatology. 38 (3): 599–612. doi:10.1053/jhep.2003.50385. ISSN 0270-9139.
- ↑ D'amico, Gennaro; Morabito, Alberto; Pagliaro, Luigi; Marubini, Ettore (1986). "Survival and prognostic indicators in compensated and decompensated cirrhosis". Digestive Diseases and Sciences. 31 (5): 468–475. doi:10.1007/BF01320309. ISSN 0163-2116.