Niacin/lovastatin warnings and precautions
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Sheng Shi, M.D. [2]
Warnings Aad Precautions
WARNINGS
ADVICOR should not be substituted for equivalent doses of immediate-release (crystalline) niacin. For patients switching from immediate-release niacin to NIASPAN, therapy with NIASPAN should be initiated with low doses (i.e., 500 mg once daily at bedtime) and the NIASPAN dose should then be titrated to the desired therapeutic response (see DOSAGE AND ADMINISTRATION).
Liver Dysfunction
Cases of severe hepatic toxicity, including fulminant hepatic necrosis, have occurred in patients who have substituted sustained-release (modified-release, timed-release) niacin products for immediate-release (crystalline) niacin at equivalent doses.
ADVICOR should be used with caution in patients who consume substantial quantities of alcohol and/or have a past history of liver disease. Active liver disease or unexplained transaminase elevations are contraindications to the use of ADVICOR.
Niacin preparations and lovastatin preparations have been associated with abnormal liver tests. In studies using NIASPAN alone, 0.8% of patients were discontinued for transaminase elevations. In studies using lovastatin alone, 0.2% of patients were discontinued for transaminase elevations.2 In three safety and efficacy studies involving titration to final daily ADVICOR doses ranging from 500 mg/10 mg to 2500 mg/40 mg, ten of 1028 patients (1.0%) experienced reversible elevations in AST/ALT to more than 3 times the upper limit of normal (ULN). Three of ten elevations occurred at doses outside the recommended dosing limit of 2000 mg/40 mg; no patient receiving 1000 mg/20 mg had 3-fold elevations in AST/ALT.
In clinical studies with ADVICOR, elevations in transaminases did not appear to be related to treatment duration; elevations in AST and ALT levels did appear to be dose related. Transaminase elevations were reversible upon discontinuation of ADVICOR.
It is recommended that liver enzyme tests be obtained prior to initiating therapy with ADVICOR and repeated as clinically indicated.
There have been rare postmarketing reports of fatal and non-fatal hepatic failure in patients taking statins, including lovastatin. If serious liver injury with clinical symptoms and/or hyperbilirubinemia or jaundice occurs during treatment with ADVICOR, promptly interrupt therapy. If an alternate etiology is not found do not restart ADVICOR.
Lovastatin and other inhibitors of HMG-CoA reductase occasionally cause myopathy, which is manifested as muscle pain or weakness associated with grossly elevated creatine kinase (> 10 times ULN). rhabdomyolysis, with or without acute renal failure secondary to myoglobinuria, has been reported rarely and can occur at any time. In a large, long-term, clinical safety and efficacy study (the EXCEL study)3,4 with lovastatin, myopathy occurred in up to 0.2% of patients treated with lovastatin 20 to 80 mg for up to 2 years. When drug treatment was interrupted or discontinued in these patients, muscle symptoms and creatine kinase (CK) increases promptly resolved. The risk of myopathy is increased by concomitant therapy with certain drugs, some of which were excluded by the EXCEL study design.
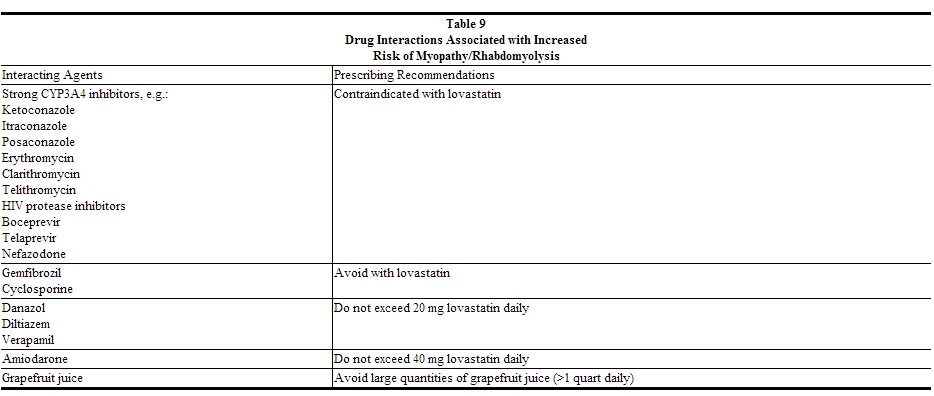
The risk of myopathy/rhabdomyolysis is increased by concomitant use of lovastatin with the following:
Strong inhibitors of CYP3A4: The risk of myopathy appears to be increased by high levels of HMG-CoA reductase inhibitory activity in plasma. Lovastatin is metabolized by the cytochrome P450 isoform 3A4. Certain drugs which share this metabolic pathway can raise the plasma levels of lovastatin and may increase the risk of myopathy. These include itraconazole, ketoconazole, and posaconazole, the macrolide antibiotics erythromycin and clarithromycin, and the ketolide antibiotic telithromycin, HIV protease inhibitors, boceprevir, telaprevir, the antidepressant nefazodone, or large quantities of grapefruit juice (>1 quart daily). Combination of these drugs with lovastatin is contraindicated. If treatment with itraconazole, ketoconazole, erythromycin, clarithromycin or telithromycin is unavoidable, therapy with lovastatin should be suspended during the course of treatment.
Although not studied clinically, voriconazole has been shown to inhibit lovastatin metabolism in vitro (human liver microsomes). Therefore, voriconazole is likely to increase the plasma concentration of lovastatin. It is recommended that dose adjustment of lovastatin be considered during coadministration. Increased lovastatin concentration in plasma has been associated with an increased risk of myopathy/rhabdomyolysis.
Gemfibrozil: The combined use of lovastatin with gemfibrozil should be avoided.
Other fibrates: Caution should be used when prescribing other fibrates with lovastatin, as these agents can cause myopathy when given alone. The benefit of further alterations in lipid levels by the combined use of lovastatin with other fibrates should be carefully weighed against the potential risks of this combination.
Cyclosporine: The use of lovastatin with cyclosporine should be avoided.
Danazol, diltiazem or verapamil with higher doses of lovastatin: In patients taking concomitant danazol, diltiazem or verapamil, the dose of lovastatin should not exceed 20 mg (see DOSAGE AND ADMINISTRATION), as the risk of myopathy increases at higher doses. The benefits of the use of lovastatin in patients receiving danazol, diltiazem, or verapamil should be carefully weighed against the risks of these combinations.
Amiodarone: In patients taking concomitant amiodarone, the dose of lovastatin should not exceed 40 mg (see DOSAGE AND ADMINISTRATION), as the risk of myopathy increases at higher doses.
Colchicine: Cases of myopathy, including rhabdomyolysis, have been reported with lovastatin coadministered with colchicine, and caution should be exercised when prescribing lovastatin with colchicine.
Ranolazine: The risk of myopathy, including rhabdomyolysis, may be increased by concomitant administration of ranolazine. Dose adjustment of lovastatin may be considered during co-administration with ranolazine.
Prescribing recommendations for interacting agents are summarized in Table 9.
 |
ADVICOR
myopathy and/or rhabdomyolysis have been reported when lovastatin is used in combination with lipid-altering doses (≥1g/day) of niacin. Physicians contemplating the use of ADVICOR, a combination of lovastatin and niacin, should weigh the potential benefits and risks, and should carefully monitor patients for any signs and symptoms of muscle pain, tenderness, or weakness, particularly during the initial month of treatment or during any period of upward dosage titration of either drug. Periodic CK determinations may be considered in such situations, but there is no assurance that such monitoring will prevent myopathy.
In clinical studies, no cases of rhabdomyolysis and one suspected case of myopathy have been reported in 1079 patients who were treated with ADVICOR at doses up to 2000 mg/40 mg for periods up to 2 years.
There have been rare reports of immune-mediated necrotizing myopathy (IMNM), an autoimmune myopathy, associated with statin use. IMNM is characterized by: proximal muscle weakness and elevated serum creatine kinase, which persist despite discontinuation of statin treatment; muscle biopsy showing necotizing myopathy without significant inflammation; improvement with immunosuppressive agents.
All patients starting therapy with ADVICOR, or whose dose of ADVICOR is being increased, should be advised of the risk of myopathy, and told to report promptly unexplained muscle pain, tenderness, or weakness particularly if accompanied by malaise or fever or if muscle signs and symptoms persist after discontinuing ADVICOR. A CK level above 10 times ULN in a patient with unexplained muscle symptoms indicates myopathy. ADVICOR therapy should be discontinued immediately if myopathy is diagnosed or suspected.
In patients with complicated medical histories predisposing to rhabdomyolysis, such as preexisting renal insufficiency, dose escalation requires caution. ADVICOR therapy should be discontinued if markedly elevated CPK levels occur or myopathy is diagnosed or suspected. ADVICOR therapy should also be temporarily withheld in any patient experiencing an acute or serious condition predisposing to the development of renal failure secondary to rhabdomyolysis, e.g., sepsis; hypotension; major surgery; trauma; severe metabolic, endocrine, or electrolyte disorders; or uncontrolled epilepsy.
PRECAUTIONS
General
Before instituting therapy with a lipid-altering medication, an attempt should be made to control dyslipidemia with appropriate diet, exercise, and weight reduction in obese patients, and to treat other underlying medical problems (see INDICATIONS AND USAGE).
Patients with a past history of jaundice, hepatobiliary disease, or peptic ulcer should be observed closely during ADVICOR therapy. Frequent monitoring of liver function tests and blood glucose should be performed to ascertain that the drug is producing no adverse effects on these organ systems.
Diabetic patients may experience a dose-related rise in fasting blood sugar (FBS). In three clinical studies, which included 1028 patients exposed to ADVICOR (6 to 22% of whom had diabetes type II at baseline), increases in FBS above normal occurred in 46 to 65% of patients at any time during study treatment with ADVICOR. Fourteen patients (1.4%) were discontinued from study treatment: 3 patients for worsening diabetes, 10 patients for hyperglycemia and 1 patient for a new diagnosis of diabetes. In the studies in which lovastatin and NIASPAN were used as active controls, 24 to 41% of patients receiving lovastatin and 43 to 58% of patients receiving NIASPAN also had increases in FBS above normal. One patient (1.1%) receiving lovastatin was discontinued for hyperglycemia. Diabetic or potentially diabetic patients should be observed closely during treatment with ADVICOR, and adjustment of diet and/or hypoglycemic therapy may be necessary.
In one long-term study of 106 patients treated with ADVICOR, elevations in prothrombin time (PT) >3 times ULN occurred in 2 patients (2%) during study drug treatment. In a long-term study of 814 patients treated with ADVICOR, 7 patients were noted to have platelet counts <100,000 during study drug treatment. Four of these patients were discontinued, and one patient with a platelet count <100,000 had prolonged bleeding after a tooth extraction. Prior studies have shown that NIASPAN can be associated with dose-related reductions in platelet count (mean of -11% with 2000 mg) and increases of PT (mean of approximately +4%). Accordingly, patients undergoing surgery should be carefully evaluated. In controlled studies, ADVICOR has been associated with small but statistically significant dose-related reductions in phosphorus levels (mean of -10% with 2000 mg/40 mg). Phosphorus levels should be monitored periodically in patients at risk for hypophosphatemia. In clinical studies with ADVICOR, hypophosphatemia was more common in males than in females. The clinical relevance of hypophosphatemia in this population is not known.
Niacin
Caution should also be used when ADVICOR is used in patients with unstable angina or in the acute phase of MI, particularly when such patients are also receiving vasoactive drugs such as nitrates, calcium channel blockers, or adrenergic blocking agents.
Elevated uric acid levels have occurred with niacin therapy; therefore, in patients predisposed to gout, niacin therapy should be used with caution. Niacin is rapidly metabolized by the liver, and excreted through the kidneys. ADVICOR is contraindicated in patients with significant or unexplained hepatic dysfunction (seeCONTRAINDICATIONS and WARNINGS) and should be used with caution in patients with renal dysfunction.
Lovastatin
Lovastatin may elevate creatine phosphokinase and transaminase levels (see WARNINGS and ADVERSE REACTIONS). This should be considered in the differential diagnosis of chest pain in a patient on therapy with lovastatin.
Endocrine function - Increases in HbA1c and fasting serum glucose levels have been reported with HMG-CoA reductase inhibitors, including lovastatin.
HMG-CoA reductase inhibitors interfere with cholesterol synthesis and as such might theoretically blunt adrenal and/or gonadal steroid production. Results of clinical studies with drugs in this class have been inconsistent with regard to drug effects on basal and reserve steroid levels. However, clinical studies have shown that lovastatin does not reduce basal plasma cortisol concentration or impair adrenal reserve, and does not reduce basal plasma testosterone concentration. Another HMG-CoA reductase inhibitor has been shown to reduce the plasma testosterone response to human chorionic gonadotropin (HCG). In the same study, the mean testosterone response to HCG was slightly but not significantly reduced after treatment with lovastatin 40 mg daily for 16 weeks in 21 men. The effects of HMG-CoA reductase inhibitors on male fertility have not been studied in adequate numbers of male patients. The effects, if any, on the pituitary-gonadal axis in premenopausal women are unknown. Patients treated with lovastatin who develop clinical evidence of endocrine dysfunction should be evaluated appropriately. Caution should also be exercised if an HMG-CoA reductase inhibitor or other agent used to lower cholesterol levels is administered to patients also receiving other drugs (e.g., spironolactone, cimetidine) that may decrease the levels or activity of endogenous steroid hormones.
CNS toxicity - Lovastatin produced optic nerve degeneration (Wallerian degeneration of retinogeniculate fibers) in clinically normal dogs in a dose-dependent fashion starting at 60 mg/kg/day, a dose that produced mean plasma drug levels about 30 times higher than the mean drug level in humans taking the highest recommended dose (as measured by total enzyme inhibitory activity). Vestibulocochlear Wallerian-like degeneration and retinal ganglion cell chromatolysis were also seen in dogs treated for 14 weeks at 180 mg/kg/day, a dose which resulted in a mean plasma drug level (Cmax) similar to that seen with the 60 mg/kg/day dose.
CNS vascular lesions, characterized by perivascular hemorrhage and edema, mononuclear cell infiltration of perivascular spaces, perivascular fibrin deposits and necrosis of small vessels, were seen in dogs treated with lovastatin at a dose of 180 mg/kg/day, a dose which produced plasma drug levels (Cmax) which were about 30 times higher than the mean values in humans taking 80 mg/day.
Similar optic nerve and CNS vascular lesions have been observed with other drugs of this class.
Cataracts were seen in dogs treated with lovastatin for 11 and 28 weeks at 180 mg/kg/day and 1 year at 60mg/kg/day.[1]
References
- ↑ "ADVICOR (NIACIN AND LOVASTATIN) TABLET, EXTENDED RELEASE [ABBVIE INC.]". Retrieved 18 February 2014.