Fetus
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]

A fetus (or foetus, or fœtus) is a developing mammal or other viviparous vertebrate, after the embryonic stage and before birth. The plural is fetuses (foetuses, fœtuses) or, very rarely, foeti.
In humans, the fetal stage of prenatal development begins about eight weeks after fertilization, when the major structures and organ systems have formed, until birth.[1]
Etymology and spelling variations
The word "fetus" is from the Latin fetus, meaning "offspring", "bringing forth", or "hatching of young".[2] It has Indo-European roots related to sucking or suckling.[3]
Foetus is an English variation on this, rather than a Latin or Greek word, but has been in use since at least 1594 according to the Oxford English Dictionary, which describes "fetus" as the etymologically preferable spelling. The word "fetus" is not derived from the Latin verb foetare, and therefore the superior etymological spelling does not include the letter "o".[4] The variant foetus or fœtus may have originated with an error by Saint Isidore of Seville, in AD 620.[5] The preferred spelling in the United States is fetus, but the variant foetus or fœtus persists in other English-speaking countries, and in some medical contexts, as well as in some other languages (e.g. French).
Human fetus
The fetal stage begins eight weeks after fertilization. The fetus is not as sensitive to damage from environmental exposures as the embryo was, though toxic exposures can often cause physiological abnormalities or minor congenital malformation. Fetal growth can be terminated by various factors, including miscarriage, feticide committed by a third party, or induced abortion.
Development
The following timeline describes some of the specific changes in fetal anatomy and physiology by fertilization age (i.e. the time elapsed since fertilization). However, it should be noted that obstetricians often use "gestational age" which, by convention, is measured from 2 weeks earlier than fertilization. For purposes of this article, age is measured from fertilization, except as noted.
- 8 weeks (condition at start of fetal stage)
- The risk of miscarriage decreases sharply at the beginning of the fetal stage.[6] At this point, all major structures, including hands, feet, head, brain, and other organs are present, but they continue to grow, develop, and become more functional.[7] When the fetal stage commences, a fetus is typically about 30 mm (1.2 inches) in length, and the heart is beating.[8] The fetus bends the head, and also makes general movements and startles that involve the whole body.[9] Brain stem activity has been detected as early as 54 days after conception.[10] Some fingerprint formation can be seen from the beginning of the fetal stage.[11]

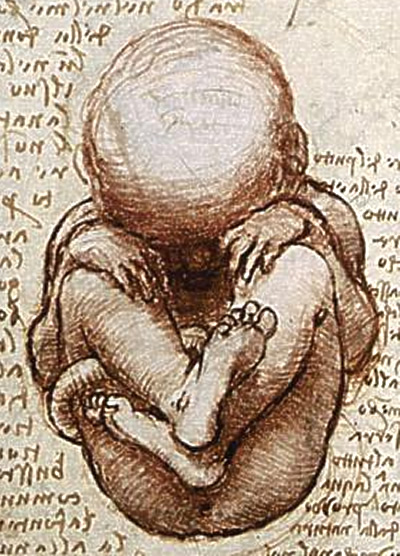
Fetus at 8 weeks after fertilization.[12] - 8 to 15 weeks
- The fetus continues to move in distinct motor patterns, picking up new patterns such as localized movement of the arms and legs, hiccups, breathing-like movements, and stretches and yawns .[9][13] The breathing-like movement of the fetus is necessary for stimulation of lung development, rather than for obtaining oxygen.[14] At nine weeks, the fetus is able to bend fingers around an object; in response to a touch on the foot, the fetus will bend the legs or curl the toes to move away from the object.[15] The face is well-formed and develops a more human appearance. Eyelids close and remain closed for several months. The different appearance of the genitals in males and females becomes pronounced. Tooth buds appear, the limbs are long and thin, and red blood cells are produced in the liver. A fine hair called lanugo develops on the head. The gastrointestinal tract, still forming, starts to collect sloughed skin and lanugo, as well as hepatic products, forming meconium (stool). Fetal skin is almost transparent. More muscle tissue and bones have developed, and the bones become harder. The first measurable signs of EEG activity occur in the 12th week.[10][16] By the end of this stage, the fetus has reached about 15 cm (6 inches).

Fetus at 18 weeks after fertilization.[17]
- 16 to 25 weeks
- The lanugo covers the entire body. Eyebrows, eyelashes, fingernails, and toenails appear. The fetus has increased muscle development. Alveoli (air sacs) are forming in lungs. The nervous system develops enough to control some body functions. The cochlea are now developed, though the myelin sheaths in the neural portion of the auditory system will continue to develop until 18 months after birth. The respiratory system has developed to the point where gas exchange is possible. The quickening, the first maternally discernable fetal movements, are often felt during this period. A woman pregnant for the first time (i.e. a primiparous woman) typically feels fetal movements at about 18-19 weeks, whereas a woman who has already given birth at least two times (i.e. a multiparous woman) will typically feel movements around 16 weeks.[18] By the end of the fifth month, the fetus is about 20 cm (8 inches).

Fetus at 38 weeks after fertilization.[19]
- 26 to 38 weeks
- The amount of body fat rapidly increases. Lungs are not fully mature. Thalamic brain connections, which mediate sensory input, form. Bones are fully developed, but are still soft and pliable. Iron, calcium, and phosphorus become more abundant. Continuous EEG readings have been observed by the 30th week.[10] Fingernails reach the end of the fingertips. The lanugo begins to disappear, until it is gone except on the upper arms and shoulders. Small breast buds are present on both sexes. Head hair becomes coarse and thicker. Birth is imminent and occurs around the 38th week. The fetus is considered full-term between weeks 35 and 40,[20] which means that the baby is considered sufficiently developed for life outside the womb.[21] It may be 48 to 53 cm (19 to 21 inches) in length, when born.
Variation in growth
Template:Seealso There is much variation in the growth of the fetus. When fetal size is less than expected, that condition is known as intrauterine growth restriction (IUGR) also called fetal growth restriction (FGR); factors affecting fetal growth can be maternal, placental, or fetal.[22]
Maternal factors include maternal weight, body mass index, nutritional state, emotional stress, toxin exposure (including tobacco, alcohol, heroin, and other drugs which can also harm the fetus in other ways), and uterine blood flow. A woman's primiparity also may affect fetal weight (firstborns tend to weigh less).
Placental factors include size, microstructure (densities and architecture), umbilical blood flow, transporters and binding proteins, nutrient utilization and nutrient production.
Fetal factors include the fetus genome, nutrient production, and hormone output. Also, female fetuses tend to weigh less than males, at full term.[22]
Fetal growth is often classified as follows: small for gestational age (SGA), appropriate for gestational age (AGA), and large for gestational age (LGA).[23] SGA can result in low birth weight, although premature birth can also result in low birth weight. Low birth weight increases risk for perinatal mortality (death shortly after birth), asphyxia, hypothermia, polycythemia, hypocalcemia, immune dysfunction, neurologic abnormalities, and other long-term health problems. SGA may be associated with growth delay, or it may instead be associated with absolute stunting of growth.
Viability
Five months is currently the lower limit of viability, and viability usually occurs later.[24] According to The Developing Human:
Viability is defined as the ability of fetuses to survive in the extrauterine environment... There is no sharp limit of development, age, or weight at which a fetus automatically becomes viable or beyond which survival is assured, but experience has shown that it is rare for a baby to survive whose weight is less than 500 gm or whose fertilization age is less than 22 weeks. Even fetuses born between 26 and 28 weeks have difficulty surviving, mainly because the respiratory system and the central nervous system are not completely differentiated... If given expert postnatal care, some fetuses weighing less than 500 gm may survive; they are referred to as extremely low birth weight or immature infants.... Prematurity is one of the most common causes of morbidity and prenatal death.[25]
During the past several decades, expert postnatal care has improved with advances in medical science, and therefore the point of viability has moved earlier.[26] As of 2006, the youngest child to survive a premature birth was a girl born at the Baptist Hospital of Miami at 21 weeks and 6 days' gestational age.[27]
Fetal pain
The subject of fetal pain and suffering is controversial. The ability of a fetus to feel pain is often part of the abortion debate. However, according to Arthur Caplan, "there is no consensus among the medical and scientific experts about precisely when a fetus becomes pain-capable."[28] Different sources have estimated that the earliest point for pain sensation may be during the first 12 weeks or after 20, 24, or 26 weeks gestation, or months after birth.
Circulatory system

The circulatory system of a human fetus works differently from that of born humans, mainly because the lungs are not in use: the fetus obtains oxygen and nutrients from the woman through the placenta and the umbilical cord.[29]
Blood from the placenta is carried to the fetus by the umbilical vein. About half of this enters the fetal ductus venosus and is carried to the inferior vena cava, while the other half enters the liver proper from the inferior border of the liver. The branch of the umbilical vein that supplies the right lobe of the liver first joins with the portal vein. The blood then moves to the right atrium of the heart. In the fetus, there is an opening between the right and left atrium (the foramen ovale), and most of the blood flows from the right into the left atrium, thus bypassing pulmonary circulation. The majority of blood flow is into the left ventricle from where it is pumped through the aorta into the body. Some of the blood moves from the aorta through the internal iliac arteries to the umbilical arteries, and re-enters the placenta, where carbon dioxide and other waste products from the fetus are taken up and enter the woman's circulation.[29]
Some of the blood from the right atrium does not enter the left atrium, but enters the right ventricle and is pumped into the pulmonary artery. In the fetus, there is a special connection between the pulmonary artery and the aorta, called the ductus arteriosus, which directs most of this blood away from the lungs (which aren't being used for respiration at this point as the fetus is suspended in amniotic fluid).[29]
Postnatal development
With the first breath after birth, the system changes suddenly. The pulmonary resistance is dramatically reduced ("pulmo" is from the Latin for "lung"). More blood moves from the right atrium to the right ventricle and into the pulmonary arteries, and less flows through the foramen ovale to the left atrium. The blood from the lungs travels through the pulmonary veins to the left atrium, increasing the pressure there. The decreased right atrial pressure and the increased left atrial pressure pushes the septum primum against the septum secundum, closing the foramen ovale, which now becomes the fossa ovalis. This completes the separation of the circulatory system into two halves, the left and the right.
The ductus arteriosus normally closes off within one or two days of birth, leaving behind the ligamentum arteriosum. The umbilical vein and the ductus venosus closes off within two to five days after birth, leaving behind the ligamentum teres and the ligamentum venosus of the liver respectively.
Differences from the adult circulatory system
Remnants of the fetal circulation can be found in adults:[30][31]
| Fetal | Adult |
|---|---|
| foramen ovale | fossa ovalis |
| ductus arteriosus | ligamentum arteriosum |
| extra-hepatic portion of the fetal left umbilical vein | ligamentum teres hepatis (the "round ligament of the liver"). |
| intra-hepatic portion of the fetal left umbilical vein (the ductus venosus) | ligamentum venosum |
| proximal portions of the fetal left and right umbilical arteries | umbilical branches of the internal iliac arteries |
| distal portions of the fetal left and right umbilical arteries | medial umbilical ligaments (urachus) |
In addition to differences in circulation, the developing fetus also employs a different type of oxygen transport molecule than adults (adults use adult hemoglobin). Fetal hemoglobin enhances the fetus' ability to draw oxygen from the placenta. Its association curve to oxygen is shifted to the left, meaning that it will take up oxygen at a lower concentration than adult hemoglobin will. This enables fetal hemoglobin to absorb oxygen from adult hemoglobin in the placenta, which has a lower pressure of oxygen than at the lungs.
Developmental problems
Congenital anomalies are anomalies that are acquired before birth. Infants with certain congenital anomalies of the heart can survive only as long as the ductus remains open: in such cases the closure of the ductus can be delayed by the administration of prostaglandins to permit sufficient time for the surgical correction of the anomalies. Conversely, in cases of patent ductus arteriosus, where the ductus does not properly close, drugs that inhibit prostaglandin synthesis can be used to encourage its closure, so that surgery can be avoided.
A developing fetus is highly susceptible to anomalies in its growth and metabolism, increasing the risk of birth defects. One area of concern is the mother's lifestyle choices made during pregnancy [32] Diet is especially important in the early stages of development. Studies show that supplementation of the mother's diet with folic acid reduces the risk of spina bifida and other neural tube defects. Another dietary concern is the consumption of breakfast by the mother. This one factor could lead to extended periods of lower than normal nutrients in the mother's blood, leading to a higher risk of prematurity, or other birth defects in the fetus. During this time alcohol consumption may increase the risk of the development of Fetal alcohol syndrome, a condition leading to mental retardation in some infants.[33] Smoking during pregnancy may also lead to reduced birth weight. Low birth weight is defined as 2500 grams (5.5 lb). Low birth weight is a concern for medical providers due to the tendency of these infants, described as premature by weight, to have a higher risk of secondary medical problems.
Legal issues
Especially since the 1970s, there has been continuing debate over the "personhood" of the human fetus. Although abortion of a fetus before viability is generally legal in the United States following the case of Roe v. Wade, the third-party-killing of a fetus can be punishable as feticide or homicide throughout the pregnancy, depending on jurisdiction.
Non-human fetuses
The fetus of most mammals develops similarly to the Homo sapiens fetus. After the first stages of development, the human embryo reaches a stage very similar to all other vertebrates.[34] The anatomy of the area surrounding a fetus is different in litter-bearing animals compared to humans: each fetus is surrounded by placental tissue and is lodged along one of two long uteri instead of the single uterus found in a human female. Development at birth is similar, with animals also having a poorly developed sense of vision and other senses.
See also
References
- ↑ Some authorities suggest that the embryonic stage may last only seven weeks. See Encyclopedia Britannica: "In humans, the organism is called an embryo for the first seven or eight weeks after conception, after which it is called a fetus." Also see People v. Taylor, California Supreme Court: "beyond the embryonic stage of seven to eight weeks."
- ↑ Harper, Douglas. (2001). Online Etymology Dictionary. Retrieved 2007-01-20.
- ↑ The American Heritage Dictionary of the English Language, Fourth Edition. Retrieved 2007-01-22.
- ↑ Peters, P. (1998). The Cambridge Australian English Style Guide, Cambridge: Cambridge University Press. ISBN 0-521-57634-2
- ↑ Aronson, Jeff (July 1997). "When I use a word...:Oe no!". British Medical Journal. BMJ Publishing Group Ltd. 315 (1). Retrieved 2006-06-29.
- ↑ -Q&A: Miscarriage. (August 6 , 2002). BBC News. Retrieved 2007-01-10.
- ↑ The Columbia Encyclopedia (Sixth Edition). Retrieved 2007-03-05.
- ↑ Greenfield, Marjorie. “Dr. Spock.com". Retrieved 2007-01-20.
- ↑ 9.0 9.1 Prechtl, Heinz. "Prenatal and Early Postnatal Development of Human Motor Behavior" in Handbook of brain and behaviour in human development, Kalverboer and Gramsbergen eds., pp. 415-418 (2001 Kluwer Academic Publishers). Retrieved 2007-03-04.
- ↑ 10.0 10.1 10.2 Singer, Peter. Rethinking life & death: the collapse of our traditional ethics, page 104 (St. Martins Press 1996). Retrieved 2007-03-04.
- ↑ Zabinski, Mark. Forensic Series Seminar, Pastore Chemical Laboratory, University of Rhode Island (February 2003) (news report retrieved 2007-01-20).
- ↑ 3D Pregnancy (large image of fetus at 8 weeks after fertilization). Retrieved 2007-08-28. A rotatable 3D version of this photo is available here, and a sketch is available here.
- ↑ Butterworth, George and Harris, Margaret. Principles of developmental psychology (Psychology Press 1994).
- ↑ Institute of Medicine of the National Academies, Preterm Birth: Causes, Consequences, and Prevention (2006). Retrieved 2007-03-04.
- ↑ Valman, H. and Pearson, J. "What the Fetus Feels", British Medical Journal, (January 26, 1980). Retrieved 2007-03-04.
- ↑ Vogel, Friedrich. Genetics and the Electroencephalogram (Springer 2000): "Slow EEG activity (0.5 – 2 c/s) can be demonstrated in the fetus even at the conceptual age of three months." Retrieved 2007-03-05.
- ↑ 3D Pregnancy (large image of fetus at 18 weeks after fertilization). Retrieved 2007-08-28. A rotatable 3D version of this photo is available here, and a sketch is available here.
- ↑ Levene, Malcolm et al. Essentials of Neonatal Medicine (Blackwell 2000), page 8. Retrieved 2007-03-04.
- ↑ 3D Pregnancy (large image of fetus at 38 weeks aftre fertilization). Retrieved 2007-08-28. A rotatable 3D version of this photo is available here, and a sketch is available here.
- ↑ Your Pregnancy: 36 Weeks BabyCenter.com Retrieved June 1, 2007.
- ↑ Word Web Online, retrieved 2007-01-26.
- ↑ 22.0 22.1 Holden, Chris and MacDonald, Anita. Nutrition and Child Health (Elsevier 2000). Retrieved 2007-03-04.
- ↑ Queenan, John. Management of High-Risk Pregnancy (Blackwell 1999). Retrieved 2007-03-04.
- ↑ Halamek, Louis. "Prenatal Consultation at the Limits of Viability", NeoReviews, Vol.4 No.6 (2003): "most neonatologists would agree that survival of infants younger than approximately 22 to 23 weeks’ estimated gestational age [i.e. 20 to 21 weeks' estimated fertilization age] is universally dismal and that resuscitative efforts should not be undertaken when a neonate is born at this point in pregnancy."
- ↑ Moore, Keith and Persaud, T. (2003). The Developing Human: Clinically Oriented Embryology'. Philadelphia: Saunders. pp. p. 103. ISBN 0-7216-9412-8.
- ↑ Roe v. Wade, 410 U.S. 113 (1973) ("viability is usually placed at about seven months (28 weeks) but may occur earlier, even at 24 weeks.") Retrieved 2007-03-04.
- ↑ Baptist Hospital of Miami, Fact Sheet (2006).
- ↑ Caplan, Arthur. Testimony to U.S. Congress, Subcommittee on the Constitution, Civil Rights, and Civil Liberties. "Oversight Hearing on Pain of the Unborn." (2005-11-01). Retrieved 2007-03-10.
- ↑ 29.0 29.1 29.2 Whitaker, Kent. Comprehensive Perinatal and Pediatric Respiratory Care (Delmar 2001). Retrieved 2007-03-04.
- ↑ Dudek, Ronald and Fix, James. Board Review Series Embryology (Lippincott 2004). Retrieved 2007-03-04.
- ↑ University of Michigan Medical School, Fetal Circulation and Changes at Birth. Retrieved 2007-03-04.
- ↑ Dalby, JT. (1978).Environmental effects on prenatal development Journal of Pediatric Psychology, 3, 105-109.
- ↑ Streissguth, A. (1997). Fetal Alcohol Syndrome: A Guide for Families and Communities. Baltimore: Brookes Publishing. ISBN 1-55766-283-5.
- ↑ ZFIN, Pharyngula Period (24-48 h). Modified from: Kimmel et al., 1995. Developmental Dynamics 203:253-310. Downloaded 5 March 2007.
External links
Template:Start box Template:Succession box Template:End box Template:Embryology
ar:جنين حي zh-min-nan:The-jî cs:Fétus da:Foster de:Fetus eo:Feto hi:भ्रूण id:Janin it:Feto he:עובר lt:Žmogaus vaisius nl:Foetus no:Foster nn:Foster qu:Sullu simple:Fetus sl:Plod (medicina) sr:Фетус su:Fétus fi:Sikiö sv:Foster