Estropipate (oral)
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Rabin Bista, M.B.B.S. [2]
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Black Box Warning
|
WARNINGS:
See full prescribing information for complete Boxed Warning.
ESTROGENS INCREASE THE RISK OF ENDOMETRIAL CANCER:
Close clinical surveillance of all women taking estrogens is important. Adequate diagnostic measures, including endometrial sampling when indicated, should be undertaken to rule out malignancy in all cases of undiagnosed persistent or recurring abnormal vaginal bleeding. There is no evidence that the use of “natural” estrogens result in a different endometrial risk profile than “synthetic” estrogens at equivalent estrogen doses CARDIOVASCULAR AND OTHER RISKS: Estrogens with and without progestins should not be used for the prevention of cardiovascular disease. (See WARNINGS, CARDIOVASCULAR DISORDERS.) The Women’s Health Initiative (WHI) study reported increased risks of myocardial infarction, stroke, invasive breast cancer, pulmonary emboli, and deep vein thrombosis in postmenopausal women (50 to 79 years of age) during 5 years of treatment with oral conjugated estrogens (CE 0.625 mg) combined with medroxyprogesterone acetate (MPA 2.5 mg) relative to placebo. The Women’s Health Initiative Memory Study (WHIMS), a substudy of WHI, reported increased risk of developing probable dementia in postmenopausal women 65 years of age or older during 4 years of treatment with oral conjugated estrogens plus medroxyprogesterone acetate relative to placebo. It is unknown whether this finding applies to younger postmenopausal women or to women taking estrogen alone therapy. |
Overview
Estropipate (oral) is a Endocrine-Metabolic Agent that is FDA approved for the treatment of vasomotor symptoms associated with the menopause, vulval and vaginal atrophy, hypoestrogenism due to hypogonadism, Prevention of postmenopausal osteoporosis. There is a Black Box Warning for this drug as shown here. Common adverse reactions include Edema, Chloasma, Hirsutism, Bloating, Nausea, Stomach cramps, Vomiting, Headache, Migraine, Depression, Breast tenderness, Disorder of menstruation.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Indications
- Estropipate tablets are indicated in the:
- Treatment of moderate to severe symptoms of vulval and vaginal atrophy associated with the menopause. When prescribing solely for the treatment of symptoms of vulvar and vaginal atrophy, topical vaginal products should be considered.
- Treatment of hypoestrogenism due to hypogonadism, castration or primary ovarian failure.
- Prevention of postmenopausal osteoporosis. When prescribing solely for the prevention of postmenopausal osteoporosis, therapy should only be considered for women at significant risk of osteoporosis and for whom non-estrogen medications are not considered to be appropriate.
- The mainstays for decreasing the risk of postmenopausal osteoporosis are weight-bearing exercise, adequate calcium and vitamin D intake, and when indicated, pharmacologic therapy. Postmenopausal women require an average of 1500 mg/day of elemental calcium. Therefore, when not contraindicated, calcium supplementation may be helpful for women with suboptimal dietary intake. Vitamin D supplementation of 400-800 IU/day may also be required to ensure adequate daily intake in postmenopausal women.
Dosage
- When estrogen is prescribed for a woman with a uterus, progestin should also be initiated to reduce the risk of endometrial cancer. A woman without a uterus does not need progestin. Use of estrogen, alone or in combination with a progestin, should be with the lowest effective dose and for the shortest duration consistent with treatment goals and risks for the individual woman. Patients should be reevaluated periodically as clinically appropriate (e.g., 3-month to 6-month intervals) to determine if treatment is still necessary For women who have a uterus, adequate diagnostic measures, such as endometrial sampling, when indicated, should be undertaken to rule out malignancy in cases of undiagnosed persistent or recurring abnormal vaginal bleeding.
- For treatment of moderate to severe vasomotor symptoms, vulval and vaginal atrophy associated with the menopause, the lowest dose and regimen that will control symptoms should be chosen and medication should be discontinued as promptly as possible. Attempts to discontinue or taper medication should be made at 3month to 6-month intervals. Usual dosage ranges:
- Vasomotor symptoms—One estropipate 0.75 mg tablet to two estropipate 3 mg tablets per day. The lowest dose that will control symptoms should be chosen. If the patient has not menstruated within the last two months or more, cyclic administration is started arbitrarily. If the patient is menstruating, cyclic administration is started on day 5 of bleeding.
- vulval and vaginal atrophy—One estropipate 0.75 mg tablet to two estropipate 3 mg tablets daily, depending upon the tissue response of the individual patient. The lowest dose that will control symptoms should be chosen. Administer cyclically.
- For treatment of female hypoestrogenism due to hypogonadism, castration, or primary ovarian failure. Usual dosage ranges:
- Female hypogonadism—A daily dose of one estropipate 1.5 mg tablet to three estropipate 3 mg tablets may be given for the first three weeks of a theoretical cycle, followed by a rest period of eight to ten days. The lowest dose that will control symptoms should be chosen. If bleeding does not occur by the end of this period, the same dosage schedule is repeated. The number of courses of estrogen therapy necessary to produce bleeding may vary depending on the responsiveness of the endometrium. If satisfactory withdrawal bleeding does not occur, an oral progestogen may be given in addition to estrogen during the third week of the cycle.
- Female castration or primary ovarian failure—A daily dose of one estropipate 1.5 mg tablet to three estropipate 3 mg tablets may be given for the first three weeks of a theoretical cycle, followed by a rest period of eight to ten days. Adjust dosage upward or downward according to severity of symptoms and response of the patient. For maintenance, adjust dosage to lowest level that will provide effective control.
- Treated patients with an intact uterus should be monitored closely for signs of endometrial cancer and appropriate diagnostic measures should be taken to rule out malignancy in the event of persistent or recurring abnormal vaginal bleeding.
- For prevention of osteoporosis. A daily dose of one estropipate 0.75 mg tablet for 25 days of a 31-day cycle per month.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Estropipate (oral) in adult patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Estropipate (oral) in adult patients.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
There is limited information regarding FDA-Labeled Use of Estropipate (oral) in pediatric patients.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Estropipate (oral) in pediatric patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Estropipate (oral) in pediatric patients.
Contraindications
- Estropipate tablets should not be used in women with any of the following conditions:
- Undiagnosed abnormal genital bleeding.
- Known, suspected, or history of cancer of the breast.
- Known or suspected estrogen-dependent neoplasia.
- Active deep vein thrombosis, pulmonary embolism or history of these conditions.
- Active or recent (e.g., within the past year) arterial thromboembolic disease (e.g., stroke, myocardial infarction).
- Liver dysfunction or disease.
- Estropipate tablets should not be used in patients with known hypersensitivity to its ingredients.
- Known or suspected pregnancy. There is no indication for estropipate tablets in pregnancy.
- There appears to be little or no increased risk of birth defects in children born to women who have used estrogens and progestins from oral contraceptives inadvertently during early pregnancy.
Warnings
|
WARNINGS:
See full prescribing information for complete Boxed Warning.
ESTROGENS INCREASE THE RISK OF ENDOMETRIAL CANCER:
Close clinical surveillance of all women taking estrogens is important. Adequate diagnostic measures, including endometrial sampling when indicated, should be undertaken to rule out malignancy in all cases of undiagnosed persistent or recurring abnormal vaginal bleeding. There is no evidence that the use of “natural” estrogens result in a different endometrial risk profile than “synthetic” estrogens at equivalent estrogen doses CARDIOVASCULAR AND OTHER RISKS: Estrogens with and without progestins should not be used for the prevention of cardiovascular disease. (See WARNINGS, CARDIOVASCULAR DISORDERS.) The Women’s Health Initiative (WHI) study reported increased risks of myocardial infarction, stroke, invasive breast cancer, pulmonary emboli, and deep vein thrombosis in postmenopausal women (50 to 79 years of age) during 5 years of treatment with oral conjugated estrogens (CE 0.625 mg) combined with medroxyprogesterone acetate (MPA 2.5 mg) relative to placebo. The Women’s Health Initiative Memory Study (WHIMS), a substudy of WHI, reported increased risk of developing probable dementia in postmenopausal women 65 years of age or older during 4 years of treatment with oral conjugated estrogens plus medroxyprogesterone acetate relative to placebo. It is unknown whether this finding applies to younger postmenopausal women or to women taking estrogen alone therapy. |
Cardiovascular disorders
- Estrogen and estrogen/progestin therapy have been associated with an increased risk of cardiovascular events such as myocardial infarction and stroke, as well as venous thrombosis and pulmonary embolism (venous thromboembolism or VTE). Should any of these occur or be suspected, estrogens should be discontinued immediately.
- Risk factors for arterial vascular disease (e.g., hypertension, diabetes mellitus, tobacco use, hypercholesterolemia, and obesity) and/or venous thromboembolism (e.g., personal history or family history of VTE, obesity, and systemic lupus erythematosus) should be managed appropriately.
Coronary heart disease and stroke
- In the Women’s Health Initiative (WHI) study, an increase in the number of myocardial infarctions and strokes has been observed in women receiving CE compared to placebo. These observations are preliminary, and the study is continuing.
- In the CE/MPA substudy of WHI, an increased risk of coronary heart disease (CHD) events (defined as nonfatal myocardial infarction and CHD death) was observed in women receiving CE/MPA compared to women receiving placebo (37 vs. 30 per 10,000 women-years). The increase in risk was observed in year one and persisted.
- In the same substudy of WHI, an increased risk of stroke was observed in women receiving CE/MPA compared to women receiving placebo (29 vs. 21 per 10,000 women-years). The increase in risk was observed after the first year and persisted.
- In postmenopausal women with documented heart disease (n = 2,763, average age 66.7 years) a controlled clinical trial of secondary prevention of cardiovascular disease (Heart and Estrogen/Progestin Replacement Study; HERS) treatment with CE/MPA (0.625 mg/2.5 mg per day) demonstrated no cardiovascular benefit. During an average follow-up of 4.1 years, treatment with CE/MPA did not reduce the overall rate of CHD events in postmenopausal women with established coronary heart disease. There were more CHD events in the CE/MPA-treated group than in the placebo group in year 1, but not during the subsequent years. Two thousand three hundred and twenty one women from the original HERS trial agreed to participate in an open label extension of HERS, HERS II. Average follow-up in HERS II was an additional 2.7 years, for a total of 6.8 years overall. Rates of CHD events were comparable among women in the CE/MPA group and the placebo group in HERS, HERS II, and overall.
- Large doses of estrogen (5 mg conjugated estrogens per day), comparable to those used to treat cancer of the prostate and breast, have been shown in a large prospective clinical trial in men to increase the risks of nonfatal myocardial infarction, pulmonary embolism, and thrombophlebitis.
Venous thromboembolism (VTE)
- In the Women’s Health study (WHI) an increase in VTE has been observed in women receiving CE compared to placebo. These observations are preliminary, and the study is continuing.
- In the CE/MPA treatment substudy of WHI, a 2-fold greater rate of VTE, including deep venous thrombosis and pulmonary embolism, was observed in women receiving treatment with CE/MPA compared to women receiving placebo. The rate of VTE was 34 per 10,000 woman-years in the CE/MPA group compared to 16 per 10,000 woman-years in the placebo group. The increase in VTE risk was observed during the first year and persisted.
- If feasible, estrogens should be discontinued at least 4 to 6 weeks before surgery of the type associated with an increased risk of thromboembolism, or during periods of prolonged immobilization.
Malignant neoplasms
Endometrial cancer
- The use of unopposed estrogens in women with intact uteri has been associated with an increased risk of endometrial cancer. The reported endometrial cancer risk among unopposed estrogen users is about 2–to-12 fold greater than in nonusers, and appears dependent on duration of treatment and on estrogen dose. Most studies show no significant increased risk associated with use of estrogens for less than one year. The greatest risk appears associated with prolonged use, with increased risks of 15–to-24 fold for five to ten years or more and this risk has been shown to persist for at least 8 to 15 years after estrogen therapy is discontinued.
- Clinical surveillance of all women taking estrogen/progestin combinations is important. Adequate diagnostic measures, including endometrial sampling when indicated, should be undertaken to rule out malignancy in all cases of undiagnosed persistent or recurring abnormal vaginal bleeding. There is no evidence that the use of natural estrogens results in a different endometrial risk profile than synthetic estrogens of equivalent estrogen dose. Adding a progestin to estrogen therapy has been shown to reduce the risk of endometrial hyperplasia, which may be a precursor to endometrial cancer.
Breast cancer
- The use of estrogens and progestins by postmenopausal women has been reported to increase the risk of breast cancer. The most important randomized clinical trial providing information about this issue is the Women’s Health Initiative (WHI) substudy of CE/MPA. The results from observational studies are generally consistent with those of the WHI clinical trial and report no significant variation in the risk of breast cancer among different estrogens or progestins, doses, or routes of administration.
- The CE/MPA substudy of WHI reported an increased risk of breast cancer in women who took CE/MPA for a mean follow-up of 5.6 years. Observational studies have also reported an increased risk for estrogen/progestin combination therapy, and a smaller increased risk for estrogen alone therapy, after several years of use. In the WHI trial and from observational studies, the excess risk increased with duration of use. From observational studies, the risk appeared to return to baseline in about five years after stopping treatment. In addition, observational studies suggest that the risk of breast cancer was greater, and became apparent earlier, with estrogen/progestin combination therapy as compared to estrogen alone therapy.
- In the CE/MPA substudy, 26% of the women reported prior use of estrogen alone and/or estrogen/progestin combination hormone therapy. After a mean follow-up of 5.6 years during the clinical trial, the overall relative risk of invasive breast cancer was 1.24 (95% confidence interval 1.01-1.54), and the overall absolute risk was 41 vs. 33 cases per 10,000 women-years, for CE/MPA compared with placebo. Among women who reported prior use of hormone therapy, the relative risk of invasive breast cancer was 1.86, and the absolute risk was 46 vs. 25 cases per 10,000 women-years, for CE/MPA compared with placebo. Among women who reported no prior use of hormone therapy, the relative risk of invasive breast cancer was 1.09, and the absolute risk was 40 vs. 36 cases per 10,000 women-years for CE/MPA compared with placebo. In the same substudy, invasive breast cancers were larger and diagnosed at a more advanced stage in the CE/MPA group compared with the placebo group. Metastatic disease was rare with no apparent difference between the two groups. Other prognostic factors such as histologic subtype, grade and hormone receptor status did not differ between groups.
- The use of estrogen plus progestin has been reported to result in an increase in abnormal mammograms requiring further evaluation. All women should receive yearly breast examinations by a health care provider and perform monthly breast self-examinations. In addition, mammography examinations should be scheduled based on patient age, risk factors, and prior mammogram results.
Dementia
- In the Women’s Health Initiative Memory Study (WHIMS), 4,532 generally healthy postmenopausal women 65 years of age and older were studied, of whom 35% were 70 to 74 years of age and 18% were 75 or older. After an average follow-up of 4 years, 40 women being treated with CE/MPA (1.8%, n= 2,229) and 21 women in the placebo group (0.9%, n= 2,303) received diagnoses of probable dementia. The relative risk for CE/MPA versus placebo was 2.05 (95% confidence interval 1.21 – 3.48), and was similar for women with and without histories of menopausal hormone use before WHIMS. The absolute risk of probable dementia for CE/MPA versus placebo was 45 versus 22 cases per 10,000 women-years. It is unknown whether these findings apply to younger postmenopausal women.
Gallbladder disease
- A 2- to 4-fold increase in the risk of gallbladder disease requiring surgery in postmenopausal women receiving estrogens has been reported.
Hypercalcemia
- Estrogen administration may lead to severe hypercalcemia in patients with breast cancer and bone metastases. If hypercalcemia occurs, use of the drug should be stopped and appropriate measures taken to reduce the serum calcium level.
Visual abnormalities
- Retinal vascular thrombosis has been reported in patients receiving estrogens. Discontinue medication pending examination if there is sudden partial or complete loss of vision, or a sudden onset of proptosis, diplopia, or migraine. If examination reveals papilledema or retinal vascular lesions, estrogens should be permanently discontinued.
Precautions
GENERAL
1. Addition of a progestin when a woman has not had a hysterectomy
- Studies of the addition of a progestin for 10 or more days of a cycle of estrogen administration, or daily with estrogen in a continuous regimen, have reported a lowered incidence of endometrial hyperplasia than would be induced by estrogen treatment alone. Endometrial hyperplasia may be a precursor to endometrial cancer.
- There are, however, possible risks that may be associated with the use of progestins with estrogens compared to estrogen-alone regimens. These include a possible increased risk of breast cancer, adverse effects on lipoprotein metabolism (e.g., lowering HDL, raising LDL) and impairment of glucose tolerance.
2. Elevated blood pressure
- In a small number of case reports, substantial increases in blood pressure have been attributed to idiosyncratic reactions to estrogens. In a large, randomized, placebo-controlled clinical trial, a generalized effect of estrogens on blood pressure was not seen. Blood pressure should be monitored at regular intervals with estrogen use.
3. Hypertriglyceridemia
- In patients with pre-existing hypertriglyceridemia, estrogen therapy may be associated with elevations of plasma triglycerides leading to pancreatitis and other complications.
4. Impaired liver function and past history of cholestatic jaundice
- Estrogens may be poorly metabolized in patients with impaired liver function. For patients with a history of cholestatic jaundice associated with past estrogen use or with pregnancy, caution should be exercised and in the case of recurrence, medication should be discontinued.
- Estrogen administration leads to increased thyroid-binding globulin (TBG) levels. Patients with normal thyroid function can compensate for the increased TBG by making more thyroid hormone, thus maintaining free T4 and T3 serum concentrations in the normal range. Patients dependent on thyroid hormone replacement therapy who are also receiving estrogens may require increased doses of their thyroid replacement therapy. These patients should have their thyroid function monitored in order to maintain their free thyroid hormone levels in an acceptable range.
6. Fluid retention
- Because estrogens may cause some degree of fluid retention, patients with conditions that might be influenced by this factor, such as a cardiac or renal dysfunction, warrant careful observation when estrogens are prescribed.
7. Hypocalcemia
- Estrogens should be used with caution in individuals with severe hypocalcemia.
8. Ovarian cancer
- The CE/MPA substudy of WHI reported that estrogen plus progestin increased the risk of ovarian cancer. After an average follow-up of 5.6 years, the relative risk for ovarian cancer for CE/MPA versus placebo was 1.58 (95% confidence interval 0.77 – 3.24) but was not statistically significant. The absolute risk for CE/MPA versus placebo was 4.2 versus 2.7 cases per 10,000 women-years. In some epidemiologic studies, the use of estrogen alone, in particular for ten or more years, has been associated with an increased risk of ovarian cancer. Other epidemiologic studies have not found these associations.
9. Exacerbation of endometriosis
- Endometriosis may be exacerbated with administration of estrogens. A few cases of malignant transformation of residual endometrial implants have been reported in women treated post-hysterectomy with estrogen alone therapy. For patients known to have residual endometriosis post-hysterectomy, the addition of progestin should be considered.
10. Exacerbation of other conditions
- Estrogens may cause an exacerbation of asthma, diabetes mellitus, epilepsy, migraine or porphyria, systemic lupus erythematosus, and hepatic hemangiomas and should be used with caution in women with these conditions.
B. PATIENT INFORMATION
- Physicians are advised to discuss the PATIENT INFORMATION leaflet with patients for whom they prescribe estropipate tablets.
C. LABORATORY TESTS
- Estrogen administration should be initiated at the lowest dose approved for the indication and then guided by clinical response rather than by serum hormone levels (e.g., estradiol, FSH).
Adverse Reactions
Clinical Trials Experience
- The following additional adverse reactions have been reported with estrogens and/or progestin therapy.
Genitourinary system
- Changes in vaginal bleeding pattern and abnormal withdrawal bleeding or flow; breakthrough bleeding; spotting; dysmenorrhea; increase in size of uterine leiomyomata; vaginitis; including vaginal candidiasis; change in amount of cervical secretion; changes in cervical ectropion; ovarian cancer; endometrial hyperplasia; endometrial cancer.
Breasts
- Tenderness, enlargement, pain, nipple discharge, galactorrhea; fibrocystic breast changes; breast cancer.
Cardiovascular
- Deep and superficial venous thrombosis; pulmonary embolism; thrombophlebitis; myocardial infarction; stroke; increase in blood pressure.
Gastrointestinal
- Nausea, vomiting; abdominal cramps, bloating; cholestatic jaundice; increased incidence of gallbladder disease; pancreatitis; enlargement of hepatic hemangiomas.
Skin
- Chloasma or melasma that may persist when drug is discontinued; erythema multiforme; erythema nodosum; hemorrhagic eruption; loss of scalp hair; hirsutism; pruritus, rash.
Eyes
- Retinal vascular thrombosis; steepening of corneal curvature; intolerance to contact lenses.
Central nervous system
- Headache, migraine, dizziness; mental depression; chorea; nervousness; mood disturbances; irritability; exacerbation of epilepsy; dementia.
Miscellaneous
- Increase or decrease in weight; reduced carbohydrate tolerance; aggravation of porphyria; edema; arthralgias; leg cramps; urticaria; angioedema; anaphylactoid/anaphylactic reactions; hypocalcemia; exacerbation of asthma; changes in libido; triglycerides.
Postmarketing Experience
There is limited information regarding Postmarketing Experience of Estropipate (oral) in the drug label.
Drug Interactions
- Accelerated prothrombin time, partial thromboplastin time, and platelet aggregation time; increased platelet count; increased factors II, VII antigen, VIII antigen, VIII coagulant activity, IX, X, XII, VII— X complex, II—VII—X complex, and beta-thromboglobulin; decreased levels of anti-factor Xa and antithrombin III, decreased antithrombin III activity; increased levels of fibrinogen and fibrinogen activity; increased plasminogen antigen and activity.
- Increased thyroid-binding globulin (TBG) levels leading to increased circulating total thyroid hormone, levels as measured by protein-bound iodine (PBI), T4 levels (by column or by radioimmunoassay) or T3 levels by radioimmunoassay. T3 resin uptake is decreased, reflecting the elevated TBG. Free T4 and free T3 concentrations are unaltered. Patients on thyroid replacement therapy may require higher doses of thyroid hormone.
- Other binding proteins may be elevated in serum, (i.e., corticosteroid binding globulin (CBG), sex hormone-binding globulin (SHBG), leading to increased circulating corticosteroids and sex steroids, respectively. Free or biologically active hormone concentrations are unchanged. Other plasma proteins may be increased (angiotensinogen/renin substrate, alpha-1-antitrypsin, ceruloplasmin).
- Increased plasma HDL and HDL2 subfraction concentrations, reduced LDL cholesterol concentration, increased triglycerides levels.
- Impaired glucose tolerance.
- Reduced response to metyrapone test.
- Reduced serum folate concentration.
Use in Specific Populations
Pregnancy
- Estropipate tablets should not be used during pregnancy.
- Australian Drug Evaluation Committee (ADEC) Pregnancy Category
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Estropipate (oral) in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Estropipate (oral) during labor and delivery.
Nursing Mothers
- Estrogen administration to nursing mothers has been shown to decrease the quantity and quality of the milk. Detectable amounts of estrogens have been identified in the milk of mothers receiving this drug. Caution should be exercised when estropipate is administered to a nursing woman.
Pediatric Use
There is no FDA guidance on the use of Estropipate (oral) with respect to pediatric patients.
Geriatic Use
- In the Women’s Health Initiative Memory Study, including 4,532 women 65 years of age and older, followed for an average of 4 years, 82% (n= 3,729) were 65 to 74 while 18% (n= 803) were 75 and over. Most women (80%) had no prior hormone therapy use. Women treated with conjugated estrogens plus medroxyprogesterone acetate were reported to have a two-fold increase in the risk of developing probable dementia. Alzheimer’s disease was the most common classification of probable dementia in both the conjugated estrogens plus medroxyprogesterone acetate group and the placebo group. Ninety percent of the cases of probable dementia occurred in the 54% of women that were older than 70.
Gender
There is no FDA guidance on the use of Estropipate (oral) with respect to specific gender populations.
Race
There is no FDA guidance on the use of Estropipate (oral) with respect to specific racial populations.
Renal Impairment
There is no FDA guidance on the use of Estropipate (oral) in patients with renal impairment.
Hepatic Impairment
There is no FDA guidance on the use of Estropipate (oral) in patients with hepatic impairment.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Estropipate (oral) in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Estropipate (oral) in patients who are immunocompromised.
Administration and Monitoring
Administration
Monitoring
- Treated patients with an intact uterus should be monitored closely for signs of endometrial cancer and appropriate diagnostic measures should be taken to rule out malignancy in the event of persistent or recurring abnormal vaginal bleeding.
- Blood pressure should be monitored at regular intervals with estrogen use.
- Estrogen administration leads to increased thyroid-binding globulin (TBG) levels. Patients dependent on thyroid hormone replacement therapy who are also receiving estrogens may require increased doses of their thyroid replacement therapy. These patients should have their thyroid function monitored in order to maintain their free thyroid hormone levels in an acceptable range.
IV Compatibility
There is limited information regarding IV Compatibility of Estropipate (oral) in the drug label.
Overdosage
- Serious ill effects have not been reported following acute ingestion of large doses of estrogen-containing oral contraceptives by young children. Overdosage of estrogen may cause nausea and vomiting, and withdrawal bleeding may occur in females.
Pharmacology
| |
Estropipate (oral)
| |
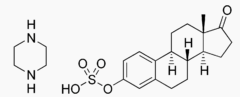
| Systematic (IUPAC) name | |
| [(8R,9S,13S,14S)-13-Methyl-17-oxo-7,8,9,11,12,14,15,16-octahydro-6H-cyclopenta[a]phenanthren-3-yl] hydrogen sulfate; piperazine | |
| Identifiers | |
| CAS number | |
| ATC code | none |
| PubChem | |
| DrugBank | |
| Chemical data | |
| Formula | Template:OrganicBox atomTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox |
| Mol. mass | 436.56 g/mol |
| SMILES | & |
| Pharmacokinetic data | |
| Bioavailability | ? |
| Metabolism | ? |
| Half life | ? |
| Excretion | ? |
| Therapeutic considerations | |
| Pregnancy cat. |
? |
| Legal status | |
| Routes | ? |
Mechanism of Action
- Endogenous estrogens are largely responsible for the development and maintenance of the female reproductive system and secondary sexual characteristics. Although circulating estrogens exist in a dynamic equilibrium of metabolic interconversions, estradiol is the principal intracellular human estrogen and is substantially more potent than its metabolites, estrone and estriol at the receptor level.
The primary source of estrogen in normally cycling adult women is the ovarian follicle, which secretes 70 to 500 mcg of estradiol daily, depending on the phase of the menstrual cycle. After menopause, most endogenous estrogen is produced by conversion of androstenedione, secreted by the adrenal cortex, to estrone by peripheral tissues. Thus, estrone and the sulfate conjugated form, estrone sulfate, are the most abundant circulating estrogens in postmenopausal women.
Estrogens act through binding to nuclear receptors in estrogen-responsive tissues. To date, two estrogen receptors have been identified. These vary in proportion from tissue to tissue.
Circulating estrogens modulate the pituitary secretion of the gonadotropins, luteinizing hormone (LH) and follicle stimulating hormone (FSH), through a negative feedback mechanism. Estrogens act to reduce the elevated levels of these hormones seen in postmenopausal women.
Structure
- Estropipate (formerly piperazine estrone sulfate), is a natural estrogenic substance prepared from purified crystalline estrone, solubilized as the sulfate and stabilized with piperazine. It is appreciably soluble in water and has almost no odor or taste — properties which are ideally suited for oral administration. The amount of piperazine in estropipate is not sufficient to exert a pharmacological action. Its addition ensures solubility, stability, and uniform potency of the estrone sulfate. Chemically estropipate, molecular weight: 436.56, is represented by estra-1,3,5(10)-trien-17-one,3-(sulfooxy)-, compound with piperazine (1:1). The structural formula may be represented as follows:
- Estropipate is available as tablets for oral administration containing either 0.75 mg, 1.5 mg, 3 mg, or 6 mg estropipate (calculated as sodium estrone sulfate 0.625 mg, 1.25 mg, 2.5 mg and 5 mg, respectively).
Inactive Ingredients
- Each tablet contains: lactose NF, magnesium stearate NF, piperazine USP, pregelatinized starch NF, talc USP, and coloring agents: 0.75 mg—D&C Yellow #10; 1.5 mg—FD&C Yellow #6; 3 mg—FD&C Blue #2; 6 mg—FD&C Blue #2 and D&C Yellow #10.
Pharmacodynamics
There is limited information regarding Pharmacodynamics of Estropipate (oral) in the drug label.
Pharmacokinetics
Absorption
- Estrogens are well absorbed through the skin and gastrointestinal tract. When applied for a local action, absorption is usually sufficient to cause systemic effects.
Distribution
- The distribution of exogenous estrogens is similar to that of endogenous estrogens. Estrogens are widely distributed in the body and are generally found in higher concentrations in the sex hormone target organs. Estrogens circulate in the blood largely bound to sex hormone binding globulin (SHBG) and albumin.
Metabolism
- Exogenous estrogens are metabolized in the same manner as endogenous estrogens. Circulating estrogens exist in a dynamic equilibrium of metabolic interconversions. These transformations take place mainly in the liver. Estradiol is converted reversibly to estrone, and both can be converted to estriol, which is the major urinary metabolite. Estrogens also undergo enterohepatic recirculation via sulfate and glucuronide conjugation in the liver, biliary secretion of conjugates into the intestine, and hydrolysis in the gut followed by reabsorption. In postmenopausal women, a significant proportion of the circulating estrogens exist as sulfate conjugates, especially estrone sulfate, which serves as a circulating reservoir for the formation of more active estrogens.
Excretion
- Estradiol, estrone, and estriol are excreted in the urine along with glucuronide and sulfate conjugates.
Drug Interactions
- In vitro and in vivo studies have shown that estrogens are metabolized partially by cytochrome P450 3A4 (CYP3A4). Therefore, inducers or inhibitors of CYP3A4 may affect estrogen drug metabolism. Inducers of CYP3A4 such as St. John’s Wort preparations (Hypericum perforatum), phenobarbital, carbamazepine, and rifampin may reduce plasma concentrations of estrogens, possibly resulting in a decrease in therapeutic effects and/or changes in the uterine bleeding profile. Inhibitors of CYP3A4 such as erythromycin, clarithromycin, ketoconazole, itraconazole, ritonavir and grapefruit juice may increase plasma concentrations of estrogens and may result in side effects.
Nonclinical Toxicology
CARCINOGENESIS, MUTAGENESIS, IMPAIRMENT OF FERTILITY
- Long-term continuous administration of estrogen, with and without progestin, in women with and without a uterus, has shown an increased risk of endometrial cancer, breast cancer, and ovarian cancer.
- Long-term continuous administration of natural and synthetic estrogens in certain animal species increases the frequency of carcinomas of the breast, uterus, cervix, vagina, testis, and liver.
Clinical Studies
Women's Health Initiative Studies
- The Women's Health Initiative (WHI) enrolled a total of 27,000 predominantly healthy postmenopausal women to assess the risks and benefits of either the use of 0.625 mg conjugated estrogens (CE) per day alone or the use of oral 0.625 mg conjugated estrogens plus 2.5 mg medroxyprogesterone acetate (MPA) per day compared to placebo in the prevention of certain chronic diseases. The primary endpoint was the incidence of coronary heart disease (CHD) (nonfatal myocardial infarction and CHD death), with invasive breast cancer as the primary adverse outcome studied. A "global index" included the earliest occurrence of CHD, invasive breast cancer, stroke, pulmonary embolism (PE), endometrial cancer, colorectal cancer, hip fracture, or death due to other cause. The study did not evaluate the effects of CE or CE/MPA on menopausal symptoms.
- The CE/MPA substudy was stopped early because, according to the predefined stopping rule, the increased risk of breast cancer and cardiovascular events exceeded the specified benefits included in the "global index." Results of the CE/MPA substudy, which included 16,608 women (average age of 63 years, range 50 to 79; 83.9% White, 6.5% Black, 5.5% Hispanic), after an average follow-up of 5.2 years are presented in Table 1 below:
- For those outcomes included in the "global index," the absolute excess risks per 10,000 person-years in the group treated with CE/MPA were 7 more CHD events, 8 more strokes, 8 more PEs, and 8 more invasive breast cancers, while absolute risk reductions per 10,000 person-years were 6 fewer colorectal cancers and 5 fewer hip fractures. The absolute excess risk of events included in the "global index" was 19 per 10,000 women-years. There was no difference between the groups in terms of all-cause mortality.
Women’s Health Initiative Memory Study
- The Women’s Health Initiative Memory Study (WHIMS), a substudy of WHI, enrolled 4,532 predominantly healthy postmenopausal women 65 years of age and older (47% were age 65 to 69 years, 35% were 70 to 74 years, and 18% were 75 years of age and older) to evaluate the effects of CE/MPA (0.625mg conjugated estrogens plus 2.5 mg medroxyprogesterone acetate) on the incidence of probable dementia (primary outcome) compared with placebo.
- After an average follow-up of 4 years, 40 women in the estrogen/progestin group (45 per 10,000 women-years) and 21 in the placebo group (22 per 10,000 women-years) were diagnosed with probable dementia. The relative risk of probable dementia in the hormone therapy group was 2.05 (95% CI, 1.21 to 3.48) compared to placebo. Differences between groups became apparent in the first year of treatment. It is unknown whether these findings apply to younger postmenopausal women.
Osteoporosis
- The results of a double-blind, placebo-controlled two-year study have shown that treatment with one tablet of estropipate 0.625 daily for 25 days (of a 31-day cycle per month) prevents vertebral bone mass loss in postmenopausal women. When estrogen therapy is discontinued, bone mass declines at a rate comparable to that of the immediate postmenopausal period. There is no evidence that estrogen replacement therapy restores to premenopausal levels.
How Supplied
- Estropipate tablets USP are supplied as follows:
- 0.75 mg Estropipate (calculated as sodium estrone sulfate 0.625 mg) as round, scored, yellow tablets, in bottles of 30, 100 and 500 tablets.
- 1.5 mg Estropipate (calculated as sodium estrone sulfate 1.25 mg) as round, scored, peach tablets, in bottles of 30, 100 and 500 tablets.
- 3 mg Estropipate (calculated as sodium estrone sulfate 2.5 mg) as round, scored, blue tablets, in bottles of 30, 100 and 500 tablets
- 6 mg Estropipate (calculated as sodium estrone sulfate 5 mg) as round, scored, green tablets, in bottles of 30, 100 and 500 tablets
Storage
- Store at 20° to 25°C (68° to 77°F).
Images
Drug Images
{{#ask: Page Name::Estropipate (oral) |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
PRINCIPAL DISPLAY PANEL

This image is provided by the National Library of Medicine. 
This image is provided by the National Library of Medicine. 
This image is provided by the National Library of Medicine.
Ingredients and Appearance
{{#ask: Label Page::Estropipate (oral) |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
Precautions with Alcohol
- Alcohol-Estropipate (oral) interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
- ESTROPIPATE®[1]
Look-Alike Drug Names
There is limited information regarding Estropipate (oral) Look-Alike Drug Names in the drug label.
Price
References
The contents of this FDA label are provided by the National Library of Medicine.



