Thymoma
For patient information click here.
| Thymoma | |
 | |
|---|---|
| Thymoma: A bottle-shaped tumor is encapsulated and shows a bulging, rather homogeneous, faintly lobulated ivory-colored cut surface. Image courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology | |
| ICD-10 | C37.9, D60 |
| ICD-9 | 164.0, 212.6 |
| ICD-O: | 8580 |
| DiseasesDB | 13067 |
| MedlinePlus | 001086 |
| eMedicine | med/2752 med/3448 ped/2246 |
| MeSH | D013945 |
|
WikiDoc Resources for Thymoma |
|
Articles |
|---|
|
Most recent articles on Thymoma |
|
Media |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Thymoma at Clinical Trials.gov Clinical Trials on Thymoma at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Thymoma
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Directions to Hospitals Treating Thymoma Risk calculators and risk factors for Thymoma
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Thymoma |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Please Join in Editing This Page and Apply to be an Editor-In-Chief for this topic:
There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [2] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Overview
In medicine (oncology), thymoma is a tumor originating from the thymus. It consists of any type of thymic epithelial cell as well as lymphocytes that are usually abundant and probably not neoplastic. Thymoma usually is benign, and frequently encapsulated; when occasionally malignant, then it is invasive: metastasis is extremely rare. Malignant lymphomas that involve the thymus, e.g., lymphosarcoma, Hodgkin's disease (termed "granulomatous thymoma" in the past), should not be regarded as thymoma. Thymoma is a rare disease, best known for its enigmatic association with the neuromuscular disorder myasthenia gravis.[1]
Signs and symptoms
A third of all people with a thymoma have symptoms due to compression of the surrounding organs by an expansive mass. This may take the form of vena cava superior syndrome (compression of the upper caval vein), dysphagia (difficulty swallowing), cough or chest pain.[1]
A third have a thymoma detected because they have an associated autoimmune disorder. The most common condition in this group is myasthenia gravis (of which 25-50% are associated with a thymoma); patients with myasthenia are routinely screened for thymoma. Other associated autoimmune conditions are pure red cell aplasia and Good's syndrome (thymoma with combined immunodeficiency and hypoimmunoglobulinemia G). Rare associations that have been reported are: acute pericarditis, Addison's disease, agranulocytosis, alopecia areata, ulcerative colitis, Cushing's disease, hemolytic anemia, limbic encephalopathy, myocarditis, nephrotic syndrome, panhypopituitarism, pernicious anemia, polymyositis, rheumatoid arthritis, sarcoidosis, scleroderma, sensorimotor radiculopathy, stiff person syndrome, systemic lupus erythematosus and thyroiditis.[1]
A third to half of all people with a thymoma have no symptoms at all, and the mass is identified on a chest X-ray performed for an unrelated problem.[1]
Diagnosis
When a thymic mass is identified, the made is achieved with histology (obtaining a tissue sample of the mass). When a thymoma is suspected, a CT/CAT scan is generally performed to estimate the size of the tumor, and can be biopsied with a CT-guided needle. There is a small risk of pneumomediastinum, mediastinitis and the risk of damaging the heart or large blood vessels. The final diagnosis is made by removing the thymus. Pathological investigation of the specimen will reveal if the tumor was benign or malignant, although the initial biopsy is usually indicative.[1]
The tumor is generally located inside the thymus, and can be calcified. Increased vascular enhancement can be indicative of malignancy, as can be pleural deposits.[1]
If the suspicion is high, some blood tests are often performed to look for associated problems or possible spread. These include: full blood count, protein electrophoresis, antibodies to the acetylcholine receptor (indicative of myasthenia), electrolytes, liver enzymes and renal function.[1]
-
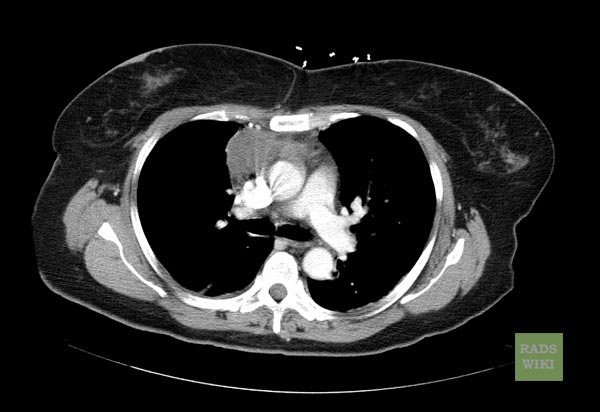
CT shows Thymoma (Image courtesy of RadsWiki and copylefted)
Pathophysiology
Thymoma originates from the epithelial cell population in the thymus. Many subtypes are recognized, some of which have a better- or worse-than-general prognosis.[1]
Treatment
Surgery is the mainstay of treatment. If the tumor was benign and was removed completely, no further therapy is necessary. Removal of the thymus in adults does not appear to induce a severe immune deficiency. In children, however, added care and scrupulous vaccination are necessary to protect from infections. Malignant tumors may need additional treatment with radiotherapy, or sometimes with chemotherapy (cyclophosphamide, doxorubicin and cisplatin).[1]
Prognosis
Thymomas associated with autoimmune disorders usually are benign. Malignant thymomas can metastasize, generally to pleura, kidney, bone, liver or brain.[1]
Epidemiology
Men and women are equally affected. The typical age at diagnosis is 30-40, although cases have been described in every age group.[1]