Scoliosis: Difference between revisions
Varun Kumar (talk | contribs) No edit summary |
m (Robot: Automated text replacement (-{{SIB}} +, -{{EH}} +, -{{EJ}} +, -{{Editor Help}} +, -{{Editor Join}} +)) |
||
| Line 171: | Line 171: | ||
*[[Spina Bifida]] | *[[Spina Bifida]] | ||
{{Diseases of the musculoskeletal system and connective tissue}} | {{Diseases of the musculoskeletal system and connective tissue}} | ||
{{Congenital malformations and deformations of musculoskeletal system}} | {{Congenital malformations and deformations of musculoskeletal system}} | ||
Revision as of 15:55, 20 August 2012
Template:DiseaseDisorder infobox
|
WikiDoc Resources for Scoliosis |
|
Articles |
|---|
|
Most recent articles on Scoliosis |
|
Media |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Scoliosis at Clinical Trials.gov Clinical Trials on Scoliosis at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Scoliosis
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Scoliosis Discussion groups on Scoliosis Directions to Hospitals Treating Scoliosis Risk calculators and risk factors for Scoliosis
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Scoliosis |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Overview
Scoliosis is a medical condition in which a person's spine is curved from side to side or front to back, and may also be rotated. On an x-ray, the spine of an individual with a typical scoliosis may look more like an "S" or a "C" than a straight line. It is typically classified as congenital (caused by vertebral anomalies present at birth), idiopathic (sub-classified as infantile, juvenile, adolescent, or adult according to when onset occurred) or as having developed as a secondary symptom of another condition, such as cerebral palsy or spinal muscular atrophy.
Terminology
Dextroscoliosis is a scoliosis with the convexity on the right side.[1][2][3]
Levoscoliosis is a scoliosis with the convexity on the left side.[1][2][3]
Cause
The cause of scoliosis is poorly understood. In the case of the most common form of scoliosis, Adolescent Idiopathic Scoliosis, there is a clear Mendelian inheritance but with incomplete penetrance. Various causes have been implicated, but none has consensus among scientists as the cause of scoliosis. Scoliosis is more common in females and is often seen in patients with cerebral palsy or spina bifida, although this form of scoliosis is different from that seen in children without these conditions. In some cases, scoliosis exists at birth due to a congenital vertebral anomaly. Occasionally development of scoliosis during adolescence is due to an underlying anomaly such as a tethered spinal cord, but most often the cause is unknown or idiopathic. Contrary to common belief, scoliosis does not come from slouching, sitting in awkward positions, or sleeping on an old mattress. Scoliosis often presents itself, or worsens, during the adolescence growth spurt. [4]
In April 2007, researchers at Texas Scottish Rite Hospital for Children identified the first gene associated with idiopathic scoliosis, CHD7. The medical breakthrough was the result of a 10-year study and is outlined in the May 2007 issue of the American Journal of Human Genetics.[5]
Complete Differential Diagnosis for Scoliosis
Nonstructural scoliosis
- Appendicitis
- Local inflammation
- Leg length discrepancy
- Muscle spasms
Structural scoliosis
- Amyoplasia congenita
- Arthrogryposis
- Bechterew's Disease
- Benign tumors
- Brucella infection of the spine
- Cerebral Palsy
- Chondrodysplasia
- Dislocation
- Dwarfism
- Ehlers-Danlos syndrome
- Fredrick's Ataxia
- Hemivertebra
- Homocystinuria
- Irradiation
- Malignant tumors
- Marfan's Syndrome
- Morquio's Disease
- Muscular Dystrophy
- Osteogenesis imperfecta
- Osteomalacia
- Osteoporosis
- Polyomyelitis
- Postoperative
- Rheumatic disease of the spine
- Rheumatoid Arthritis
- Rickets
- Salmonella infection of the spine
- Scheuermann's disease
- Spinal cord trauma
- Spinal muscular atrophy
- Still's Disease
- Syringomyelia
- Tuberculosis of the spine
- Unilateral bar
- VonRecklinghausen's Disease
Prevalence
Scoliotic curves greater than 10° affect 2-3% of the population of the United States.[6] The prevalence of curves less than 20° is about equal in males and females. Curves greater than 20° affect about 1 in 2500 people. Curves convex to the right are more common than those to the left, and single or 'C' curves are slightly more common than double or 'S' curve patterns. Males are more likely to have infantile or juvenile scoliosis, but there is a high female predominance of adolescent scoliosis. Young males are seven times more likely than young females to develop a significant, progressive curvature. Females are nine times more likely to require treatment than males as they tend to have larger, more progressive curves.
Symptoms
Pain is common in adulthood, especially if left untreated. One of the major complaints from parents and patients is cosmetic deformity.
The symptoms of scoliosis can include:
- Uneven musculature on one side of the spine
- A rib "hump" and/or a prominent shoulder blade, caused by rotation of the ribcage in thoracic scoliosis
- Uneven hip and shoulder levels
- Asymmetric size or location of breast in females
- Unequal distance between arms and body
- Clothes that do not "hang right", i.e. with uneven hemlines
- Slow nerve action (in some cases)
Associated conditions
Scoliosis is sometimes associated with other conditions such as cerebral palsy, spinal muscular atrophy, familial dysautonomia, CHARGE syndrome, Friedreich's ataxia, Spina bifidas, Marfan's syndrome, neurofibromatosis, connective tissue disorders, and craniospinal axis disorders (e.g., syringomyelia, Arnold-Chiari malformation).
However, the majority of people with adolescent scoliosis have no pain or other abnormalities.
Investigation

Patients who initially present with scoliosis are examined to determine if there is an underlying cause of the deformity. During a physical examination, the following is assessed:
- Skin for café au lait spots indicative of neurofibromatosis
- The feet for cavovarus deformity
- Abdominal reflexes
- Muscle tone for spasticity
During the exam, the patient is asked to bend forward (Adam's Bend Test). If a hump is noted, then scoliosis is a possibility and the patient should be sent for an x-ray to confirm the diagnosis.
The patient's gait is assessed, and there is an exam for signs of other abnormalities (e.g., Spina bifida as evidenced by a dimple, hairy patch, lipoma, or hemangioma).
A thorough neurological examination is also performed.
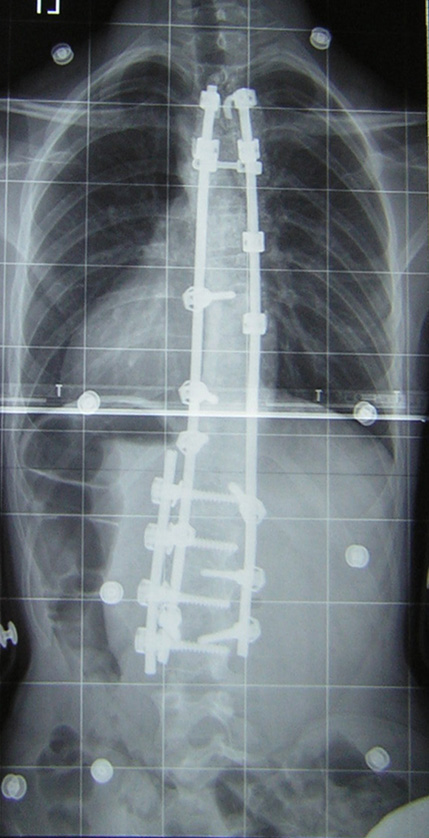
Many doctors when suspecting scoliosis will exclaim "scolie and AP-Lateral", which are two types of X-ray. The scolie is pictured above, a scolie is an X-ray taken from the rear. An AP-Lateral is taken from the side but the xray machine is programmed only to show the spine with high definition.
Full-length standing spine X rays are the standard method for evaluating the severity and progression of the scoliosis, and whether it is congenital or idiopathic in nature. In growing individuals, serial radiographs are obtained at 3-12 month intervals to follow curve progression. In some instances, MRI investigation is warranted.
The standard method for assessing the curvature quantitatively is measurement of the Cobb angle, which is the angle between two lines, drawn perpendicular to the upper endplate of the uppermost vertebrae involved and the lower endplate of the lowest vertebrae involved. For patients who have two curves, Cobb angles are followed for both curves. In some patients, lateral bending xrays are obtained to assess the flexibility of the curves or the primary and compensatory curves.
Prognosis
The prognosis of scoliosis depends on the likelihood of progression. The general rules of progression are that larger curves carry a higher risk of progression than smaller curves, and that thoracic and double primary curves carry a higher risk of progression than single lumbar or thoracolumbar curves. In addition, patients who have not yet reached skeletal maturity have a higher likelihood of progression.
Management
The traditional medical management of scoliosis is complex and is determined by the severity of the curvature, skeletal maturity, which together help predict the likelihood of progression.
The conventional options are, in order:
- Observation
- Bracing - for example the Milwaukee brace
- Surgery
Bracing is only done when the patient has bone growth remaining, and is generally implemented in order to hold the curve and prevent it from progressing to the point where surgery is necessary. Bracing involves fitting the patient with a device that covers the torso and in some cases it extends to the neck. The most commonly used brace is a TLSO, a corset-like appliance that fits from armpits to hips and is custom-made from plastic. It is usually worn 23 hours a day and applies pressure on the curves in the spine. Bracing is only mildly effective as compliance is typically low, although some of the newer braces (such as the Charleston back brace) are touting better compliance rates and outcomes. Typically braces are only used for idiopathic curves that are not grave enough to warrant surgery, but they may also be used to prevent the progression of more severe curves in young children, in order to buy the child time to grow before performing surgery which would prevent further growth in the part of the spine affected.
In infantile, and sometimes juvenile scoliosis, a body cast or plaster jacket may be used instead of a brace. It has been proven possible to permanently correct some cases of infantile idiopathic scoliosis by using a series of plaster body casts applied under corrective traction, which help to "mould" the infant's soft bones and work with their infantile growth spurts. This method was pioneered by UK scoliosis specialist Min Mehta.
Chiropractic and physical therapy have some degree of anecdotal success in treating scoliosis that is primarily neuromuscular in nature, however non-surgical approaches will not address severe bone deformities associated with many cases of scoliosis. Chiropractors utilize joint mobilization techniques and therapeutic exercise to increase a scoliosis patient's flexibility and strength, theorizing that this better enables the brace to influence the curvature of the spine. Electronic Muscle Stimulation (EMS) is another therapeutic modality commonly utilized by chiropractors and physical therapists to reduce muscle spasms and strengthen atrophied muscles.
There is limited published scientific research to evaluate the efficiency of treatment programs that include a combination of bracing along with physical therapy. While much debate remains in the scientific community about whether or not chiropractic and physical therapy can influence scoliotic curvature, there may well be palliative benefit from them in scoliosis patients who experience back pain either directly as a result of their deformity or indirectly from wearing an uncomfortable brace for the vast majority of the day.
A non-invasive treatment for idiopathic scoliosis used successfully in Europe since the 1920s was established in the English-speaking world in the first years of the 21st century. Originally developed in Germany by scoliosis sufferer Katharina Schroth, this method is now taught to scoliosis patients in clinics specifically devoted to Schroth therapy in Germany, Spain, England, and, most recently, the United States. Physical therapists who do not specialize exclusively in Schroth therapy but who have received Schroth certification through the clinics in Spain and Germany offer Schroth therapy throughout Europe, parts of the Middle East, and the United States.
The Schroth method of physical therapy, combined with the Rigo-Cheneau bracing system (developed by Dr. Manuel Rigo of Spain and Dr. Jacques Cheneau of France), addresses scoliosis from a three-dimensional approach both to prevent progression of scoliotic curvature (in children) and reduce resulting pain as well as promote anatomical symmetry (in children and adults). Because each individual's curve is unique, and because scoliosis involves the rotation (twisting) of vertebrae--in different directions in different areas of the spine--as well as the side-to-side, S-shaped or C-shaped curvature, this three-dimensional approach seeks both to "untwist" (or de-rotate) and to straighten the spine by employing specialized equipment and exercises that elongate shortened muscles and strengthen overstretched, overtaxed muscles. The exercises are augmented by a technique called "rotational breathing," which expands collapsed portions of the rib cage, thus also helping to pull the spine out of its twisting and curving.
In children with immature skeletons and remaining growth potential, Schroth-method physical therapy is used in combination with the Rigo System-Cheneau brace not only to prevent progression of (and sometimes reduce) the condition but also to train and strengthen patients in holding their bodies in as corrected a position as possible after completion of the bracing treatment (i.e., when the skeleton has reached maturity). A patient's consistent practicing of an individualized Schroth program for one-half hour per day, after an initial intensive training period of two to six weeks, has been clinically shown to inhibit the mechanical forces, exacerbated by poor postural habits and gravity, that otherwise perpetuate the progression of the curvature over time (the so-called "vicious cycle"), even after the cessation of physical growth.
Bracing
Bracing is commonly prescribed to prevent progression of the spinal curvature in adolescents. There are several types of braces depending on the individual's condition and type of curve. These include the Boston Brace, also known as the Thoraco-Lumbo-Sacral-Orthosis, that fits around the patient's body like a jacket, pressing against the rib cage to prevent the spine curving inwards. Another type of brace is the Milwaukee brace, or the Cervico-Lumbo-Sacral-Orthosis. The features that separate it from a Boston Brace are large metal bars that extend around the shoulders to help against spine curvature. The third type of brace, the Charleston Bending Brace, is molded to work when the patient is lying on their side. It is used only at night.
There is also a new type of brace called Spincor which attempts to improve quality of wearer's life by allowing freedom of movement and improved cosmesis. Large scale clinical trial has been completed and results are very promising. Spinecorcan be worn by adults as a postural support as well as a treatment for Adolescent Idiopathic Scoliosis.
The amount of time an adolescent has to wear a brace each day can range from sixteen hours a day to twenty-three hours a day, depending on the patient. A recent study shows that there is no significant difference between these two time ranges.
Adolescent patients can be required to wear the brace for as long as five years, and generally lasts until his or her growth spurt has completed. Braces are not always effective, however, and patients may require surgery even after being braced.
Surgery
Surgery is usually indicated for curves that have a high likelihood of progression, curves that cause a significant amount of pain with some regularity, curves that would be cosmetically unacceptable as an adult, curves in patients with spina bifida and cerebral palsy that interfere with sitting and care, and curves that affect physiological functions such as breathing.
Surgery for scoliosis is usually done by an orthopaedic surgeon who specializes in spine surgery. For various reasons it is usually impossible to completely straighten a scoliotic spine, but in most cases very good corrections are achieved.
Spinal fusion with instrumentation
Spinal fusion is the most widely performed surgery for scoliosis. In this procedure, bone (either harvested from elsewhere in the body (autograft), or donor bone (allograft) is grafted to the vertebrae so that when it heals, they will form one solid bone mass and the vertebral column becomes rigid. This prevents worsening of the curve at the expense of spinal movement. This can be performed from the anterior (front) aspect of the spine by entering the thoracic or abdominal cavity, or performed from the back (posterior). A combination of both is used in more severe cases.
Originally, spinal fusions were done without metal implants. A cast was applied after the surgery, usually under traction to pull the curve as straight as possible and then hold it there while fusion took place. Unfortunately, there was a relatively high risk of pseudarthrosis (fusion failure) at one or more levels and significant correction could not always be achieved. In 1962, Paul Harrington introduced a metal spinal system of instrumentation which assisted with straightening the spine, as well as holding it rigid while fusion took place. The original, now obsolete Harrington rod operated on a ratchet system, attached by hooks to the spine at the top and bottom of the curvature that when cranked would distract, or straighten, the curve. A major shortcoming of the Harrington method was that it failed to produce a posture where the skull would be in proper alignment with the pelvis and it didn't address rotational deformity. As a result, unfused parts of the spine would try to compensate for this in the effort to "stand up straight". As the person aged, there would be increased "wear and tear", early onset arthritis, disc degeneration, muscular stiffness and pain with eventual reliance on painkillers, further surgery, inability to work full-time and disability. "Flatback" became the medical name for a related complication, especially for those who had lumbar scoliosis. Modern spinal systems are attempting to address sagittal imbalance and rotational defects unresolved by the Harrington rod system. They involve a combination of rods, screws, hooks and wires fixing the spine and can apply stronger, safer forces to the spine than the Harrington rod. Spinal fusion is rarely performed without this instrumentation.
Modern spinal fusions generally have good outcomes with high degrees of correction and low rates of failure and infection. Patients with fused spines and permanent implants tend to have normal lives with unrestricted activities when they are younger, it remains to be seen whether those that have been treated with the newer surgical techniques will develop problems as they age. They are able to participate in recreational athletics, have natural childbirth and are generally satisfied with their treatment. The most notable limitation of spinal fusions is that patients who have undergone surgery for scoliosis are ineligible for military service in the United States.
In cases where scoliosis has caused a significant deformity resulting in a rib hump, it is often possible to perform a surgery called a "costoplasty" (also called "thorocoplasty") in order to achieve a more pleasing cosmetic result. This procedure may be performed at any time after a fusion surgery, whether as part of the same operation or several years afterwards. As stated before, it is usually impossible to completely straighten and untwist a scoliotic spine, and it should be noted that the level of cosmetic success will depend on the extent to which the fused spine still rotates out into the ribcage. A rib hump is evidence that there is still some rotational deformity to the spine. Specific weight training techniques can be used to influence this rotational deformity in the unfused parts of the spine. This leads to a marked decrease in pain and to some improvement in organ function depending on the person's particular case and is to be recommended over any cosmetic surgical procedure.
Alternatives
Recently, new implants have been developed that aim to delay spinal fusion and to allow more spinal growth in young children. These include rods that are extendible and allow growth while still applying corrective forces and vertebral stapling which is a method of retarding normal growth on the convex side of a curve, allowing the concave side to 'catch up.' For the youngest patients, whose thoracic insufficiency compromises their ability to breathe and applies significant cardiac pressure, ribcage implants that push the ribs apart on the concave side of the curve may be especially useful. These Vertical Expandable Prosthetic Titanium Ribs (VEPTR) provide the benefit of expanding the thoracic cavity and straightening the spine in all three dimensions while allowing the spine to grow. Although these methods are novel and promising, these treatments are only suitable for growing patients. Spinal fusion remains the 'gold-standard' of surgical treatment for scoliosis. There are now non-surgical ways to help treat scoliosis, as mentioned above in the management section.
References
- ↑ 1.0 1.1 Richardson ML. Approaches to differential diagnosis in musculoskeletal imaging. Univ. of Washington School of Medicine. URL: http://www.rad.washington.edu/mskbook/scoliosis.html. Accessed on: January 8, 2006.
- ↑ 2.0 2.1 Morningstar M, Joy T. "Scoliosis treatment using spinal manipulation and the Pettibon Weighting Systemtrade mark: a summary of 3 atypical presentations". Chiropr Osteopat. 14: 1. PMID 16409627. Free Full Text.
- ↑ 3.0 3.1 Chief Pediatric Resident. Scoliosis. Univ. of Chicago. URL: http://pediatrics.uchicago.edu/chiefs/documents/Scoliosis-Gina.pdf. Accessed on: January 8, 2006.
- ↑ http://www.ucihealth.com/news/uci%20health/win01scoliosis.htm Scoliosis
- ↑ Texas Scottish Rite Hospital for Children Research: Scoliosis Research
- ↑ http://www.scoliosis.org/info.php
Additional references
- Canale: Campbell's Operative Orthopaedics, 10th ed., Copyright © 2003 Mosby, Inc.
See also
Template:Diseases of the musculoskeletal system and connective tissue
ar:جنف(سکولیوز( bg:Сколиоза ca:Escoliosi cs:Skolióza da:Skoliose de:Skoliose fa:اسکولیوز fi:Skolioosi he:עקמת it:Scoliosi ms:Skoliosis nl:Scoliose sk:Skolióza sv:Skolios