Pulmonary contusion natural history: Difference between revisions
Kashish Goel (talk | contribs) (Created page with "{{Pulmonary contusion}} {{CMG}} ==Complications== Pulmonary contusion can result in respiratory failure—about half of such cases occur within a few hours of the initial trauma....") |
No edit summary |
||
| (6 intermediate revisions by 2 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | |||
{{Pulmonary contusion}} | {{Pulmonary contusion}} | ||
{{CMG}} | {{CMG}} | ||
==Overview== | |||
==Natural History== | |||
The severity ranges from mild to deadly—small contusions may have little or no impact on the patient's health—yet pulmonary contusion is the most common type of potentially lethal chest trauma. It occurs in 30–75% of severe chest injuries. With an estimated mortality rate of 14–40%, pulmonary contusion plays a key role in determining whether an individual will die or suffer serious ill effects as the result of trauma. Pulmonary contusion is usually accompanied by other injuries. Although associated injuries are often the cause of death, pulmonary contusion is thought to cause death directly in a quarter to half of cases. Children are at especially high risk for the injury because the relative flexibility of their bones prevents the chest wall from absorbing force from an impact, causing it to be transmitted instead to the lung. Pulmonary contusion is associated with complications including [[pneumonia]] and [[acute respiratory distress syndrome]], and it can cause long-term respiratory disability. | |||
==Complications== | ==Complications== | ||
Pulmonary contusion can result in respiratory failure—about half of such cases occur within a few hours of the initial trauma.<ref name="pmid18420127">{{cite journal| author=Johnson SB| title=Tracheobronchial injury. | journal=Semin Thorac Cardiovasc Surg | year= 2008 | volume= 20 | issue= 1 | pages= 52-7 | pmid=18420127 | doi=10.1053/j.semtcvs.2007.09.001 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18420127 }} </ref> Other severe complications, including infections and [[acute respiratory distress syndrome]] ([[ARDS]]) occur in up to half of cases.<ref name="pmid9853720">{{cite journal| author=Allen GS, Cox CS| title=Pulmonary contusion in children: diagnosis and management. | journal=South Med J | year= 1998 | volume= 91 | issue= 12 | pages= 1099-106 | pmid=9853720 | doi= | pmc= | url= }} </ref> Elderly people and those who have heart, lung, or kidney disease prior to the injury are more likely to stay longer in hospital and have complications from the injury. Complications occur in 55% of people with heart or lung disease and 13% of those without.<ref name="pmid17019186">{{cite journal| author=Klein Y, Cohn SM, Proctor KG| title=Lung contusion: pathophysiology and management. | journal=Curr Opin Anaesthesiol | year= 2002 | volume= 15 | issue= 1 | pages= 65-8 | pmid=17019186 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17019186 }} </ref> Of people with pulmonary contusion alone, 17% develop ARDS, while 78% of people with at least two additional injuries develop the condition.<ref name="pmid17650697">{{cite journal| author=Miller DL, Mansour KA| title=Blunt traumatic lung injuries. | journal=Thorac Surg Clin | year= 2007 | volume= 17 | issue= 1 | pages= 57-61, vi | pmid=17650697 | doi=10.1016/j.thorsurg.2007.03.017 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17650697 }} </ref> A larger contusion is associated with an increased risk. In one study, 82% of people with 20% or more of the lung volume affected developed ARDS, while only 22% of people with less than 20% did so.<ref name="pmid14979330">{{cite journal| author=Wanek S, Mayberry JC| title=Blunt thoracic trauma: flail chest, pulmonary contusion, and blast injury. | journal=Crit Care Clin | year= 2004 | volume= 20 | issue= 1 | pages= 71-81 | pmid=14979330 | doi= | pmc= | url= }} </ref> | Pulmonary contusion can result in respiratory failure—about half of such cases occur within a few hours of the initial trauma.<ref name="pmid18420127">{{cite journal| author=Johnson SB| title=Tracheobronchial injury. | journal=Semin Thorac Cardiovasc Surg | year= 2008 | volume= 20 | issue= 1 | pages= 52-7 | pmid=18420127 | doi=10.1053/j.semtcvs.2007.09.001 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18420127 }} </ref> Other severe complications, including infections and [[acute respiratory distress syndrome]] ([[ARDS]]) occur in up to half of cases.<ref name="pmid9853720">{{cite journal| author=Allen GS, Cox CS| title=Pulmonary contusion in children: diagnosis and management. | journal=South Med J | year= 1998 | volume= 91 | issue= 12 | pages= 1099-106 | pmid=9853720 | doi= | pmc= | url= }} </ref> Elderly people and those who have heart, lung, or kidney disease prior to the injury are more likely to stay longer in hospital and have complications from the injury. Complications occur in 55% of people with heart or lung disease and 13% of those without.<ref name="pmid17019186">{{cite journal| author=Klein Y, Cohn SM, Proctor KG| title=Lung contusion: pathophysiology and management. | journal=Curr Opin Anaesthesiol | year= 2002 | volume= 15 | issue= 1 | pages= 65-8 | pmid=17019186 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17019186 }} </ref> Of people with pulmonary contusion alone, 17% develop ARDS, while 78% of people with at least two additional injuries develop the condition.<ref name="pmid17650697">{{cite journal| author=Miller DL, Mansour KA| title=Blunt traumatic lung injuries. | journal=Thorac Surg Clin | year= 2007 | volume= 17 | issue= 1 | pages= 57-61, vi | pmid=17650697 | doi=10.1016/j.thorsurg.2007.03.017 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17650697 }} </ref> A larger contusion is associated with an increased risk. In one study, 82% of people with 20% or more of the lung volume affected developed ARDS, while only 22% of people with less than 20% did so.<ref name="pmid14979330">{{cite journal| author=Wanek S, Mayberry JC| title=Blunt thoracic trauma: flail chest, pulmonary contusion, and blast injury. | journal=Crit Care Clin | year= 2004 | volume= 20 | issue= 1 | pages= 71-81 | pmid=14979330 | doi= | pmc= | url= }} </ref> | ||
[[Image:AARDS X-ray cropped.jpg|thumb|left|A chest X-ray showing acute respiratory distress syndrome]] | [[Image:AARDS X-ray cropped.jpg|thumb|left|A chest X-ray showing acute respiratory distress syndrome]] | ||
Pneumonia, another potential complication, develops in as many as 20% of people with pulmonary contusion.<ref name=" | Pneumonia, another potential complication, develops in as many as 20% of people with pulmonary contusion.<ref name="pmid18158142">{{cite journal| author=Tovar JA| title=The lung and pediatric trauma. | journal=Semin Pediatr Surg | year= 2008 | volume= 17 | issue= 1 | pages= 53-9 | pmid=18158142 | doi=10.1053/j.sempedsurg.2007.10.008 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18158142 }} </ref> Contused lungs are less able to remove bacteria than uninjured lungs, predisposing them to infection.<ref name="Fry07">{{cite book | author=Fry DE | chapter=Surgical infection |editor=O'Leary JP, Tabuenca A, Capote LR | title=The Physiologic Basis of Surgery | publisher=Lippincott Williams & Wilkins | location=Hagerstown, MD |year=2007 |pages=241 |isbn=0-7817-7138-2 }}</ref> Intubation and mechanical ventilation further increase the risk of developing pneumonia; the tube is passed through the nose or mouth into the airways, potentially tracking bacteria from the mouth or sinuses into them. Also, intubation prevents coughing, which would clear bacteria-laden secretions from the airways, and secretions pool near the tube's cuff and allow bacteria to grow.<ref name="pmid17650693">{{cite journal| author=Sutyak JP, Wohltmann CD, Larson J| title=Pulmonary contusions and critical care management in thoracic trauma. | journal=Thorac Surg Clin | year= 2007 | volume= 17 | issue= 1 | pages= 11-23, v | pmid=17650693 | doi=10.1016/j.thorsurg.2007.02.001 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17650693 }} </ref> The sooner the [[endotracheal tube]] is removed, the lower the risk of pneumonia, but if it is removed too early and has to be put back in, the risk of pneumonia rises. People who are at risk for [[pulmonary aspiration]] (e.g. those with lowered level of consciousness due to head injuries) are especially likely to get pneumonia.<ref name="pmid17650693">{{cite journal| author=Sutyak JP, Wohltmann CD, Larson J| title=Pulmonary contusions and critical care management in thoracic trauma. | journal=Thorac Surg Clin | year= 2007 | volume= 17 | issue= 1 | pages= 11-23, v | pmid=17650693 | doi=10.1016/j.thorsurg.2007.02.001 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17650693 }} </ref> As with ARDS, the chances of developing pneumonia increase with the size of the contusion. Children and adults have been found to have similar rates of complication with pneumonia and ARDS.<ref name="pmid9853720">{{cite journal| author=Allen GS, Cox CS| title=Pulmonary contusion in children: diagnosis and management. | journal=South Med J | year= 1998 | volume= 91 | issue= 12 | pages= 1099-106 | pmid=9853720 | doi= | pmc= | url= }} </ref> | ||
===Bleeding and edema=== | ===Bleeding and edema=== | ||
In contusions, torn [[capillary|capillaries]] leak fluid into the tissues around them.<ref name="Fleisher06">{{cite book |chapter=Thoracic trauma|editor=Fleisher GR, Ludwig S, Henretig FM, Ruddy RM, Silverman BK |title=Textbook of Pediatric Emergency Medicine |publisher=Lippincott Williams & Wilkins|location=Hagerstown, MD |year=2006 |pages=1434–1441 |isbn=0-7817-5074-1}}</ref> The membrane between alveoli and capillaries is torn; damage to this[[Alveolar-capillary barrier|capillary–alveolar membrane]] and small blood vessels causes blood and fluids to leak into the alveoli and the [[interstitial space]] (the space surrounding cells) of the lung.<ref name=" | In contusions, torn [[capillary|capillaries]] leak fluid into the tissues around them.<ref name="Fleisher06">{{cite book |chapter=Thoracic trauma|editor=Fleisher GR, Ludwig S, Henretig FM, Ruddy RM, Silverman BK |title=Textbook of Pediatric Emergency Medicine |publisher=Lippincott Williams & Wilkins|location=Hagerstown, MD |year=2006 |pages=1434–1441 |isbn=0-7817-5074-1}}</ref> The membrane between alveoli and capillaries is torn; damage to this[[Alveolar-capillary barrier|capillary–alveolar membrane]] and small blood vessels causes blood and fluids to leak into the alveoli and the [[interstitial space]] (the space surrounding cells) of the lung.<ref name="pmid12042932">{{cite journal| author=Gavelli G, Canini R, Bertaccini P, Battista G, Bnà C, Fattori R| title=Traumatic injuries: imaging of thoracic injuries. | journal=Eur Radiol | year= 2002 | volume= 12 | issue= 6 | pages= 1273-94 | pmid=12042932 | doi=10.1007/s00330-002-1439-6 | pmc= | url= }} </ref> With more severe trauma, there is a greater amount of edema, bleeding, and tearing of the alveoli.<ref name="pmid12793615">{{cite journal| author=Ullman EA, Donley LP, Brady WJ| title=Pulmonary trauma emergency department evaluation and management. | journal=Emerg Med Clin North Am | year= 2003 | volume= 21 | issue= 2 | pages= 291-313 | pmid=12793615 | doi= | pmc= | url= }} </ref> Pulmonary contusion is characterized by [[hemorrhage|microhemorrhage]]s (tiny bleeds) that occur when the[[alveoli]] are traumatically separated from airway structures and blood vessels. Blood initially collects in the interstitial space, and then edema occurs by an hour or two after injury. An area of in the contused lung is commonly surrounded by an area of edema. In normal [[gas exchange]], [[carbon dioxide]] [[diffusion|diffuses]] across the [[endothelium]] of the capillaries, the interstitial space, and across the alveolar epithelium; oxygen diffuses in the other direction. Fluid accumulation interferes with gas exchange,<ref name="Bailey06">{{cite book | author=Bailey BJ, Johnson JT, Newlands SD, Calhoun KS, Deskin RW | title=Head and Neck Surgery—Otolaryngology |publisher=Lippincott Williams & Wilkins | location=Hagerstown, MD | year=2006 | page=929 | isbn=0-7817-5561-1 }}</ref> and can cause the alveoli to fill with proteins and collapse due to edema and bleeding. The larger the area of the injury, the more severe respiratory compromise will be. | ||
===Consolidation and collapse=== | ===Consolidation and collapse=== | ||
Pulmonary contusion can cause parts of the lung to [[consolidation (medicine)|consolidate]], alveoli to collapse, and [[atelectasis]] (partial or total lung collapse) to occur.<ref name="Keough01">{{cite journal |author=Keough V, Pudelek B |title=Blunt chest trauma: Review of selected pulmonary injuries focusing on pulmonary contusion |journal=AACN Clinical Issues |volume=12 |issue=2 |pages=270–281 |year=2001 |pmid=11759554}}</ref> Consolidation occurs when the parts of the lung that are normally filled with air fill with material from the pathological condition, such as blood.<ref name="Pryor98">{{cite book|author=Collins CD, Hansell DM |chapter=Thoracic imaging |editor=Pryor JA, Webber BR| title=Physiotherapy for Respiratory and Cardiac Problems|publisher=Churchill Livingstone |location=Edinburgh |year=1998 |pages= 35 |isbn=0-443-05841-5}}</ref> Over a period of hours after the injury, the alveoli in the injured area thicken and may become consolidated. | Pulmonary contusion can cause parts of the lung to [[consolidation (medicine)|consolidate]], alveoli to collapse, and [[atelectasis]] (partial or total lung collapse) to occur.<ref name="Keough01">{{cite journal |author=Keough V, Pudelek B |title=Blunt chest trauma: Review of selected pulmonary injuries focusing on pulmonary contusion |journal=AACN Clinical Issues |volume=12 |issue=2 |pages=270–281 |year=2001 |pmid=11759554}}</ref> Consolidation occurs when the parts of the lung that are normally filled with air fill with material from the pathological condition, such as blood.<ref name="Pryor98">{{cite book|author=Collins CD, Hansell DM |chapter=Thoracic imaging |editor=Pryor JA, Webber BR| title=Physiotherapy for Respiratory and Cardiac Problems|publisher=Churchill Livingstone |location=Edinburgh |year=1998 |pages= 35 |isbn=0-443-05841-5}}</ref> Over a period of hours after the injury, the alveoli in the injured area thicken and may become consolidated. A decrease in the amount of [[surfactant]] produced also contributes to the collapse and consolidation of alveoli; inactivation of surfactant increases their [[surface tension]]. Reduced production of surfactant can also occur in surrounding tissue that was not originally injured. | ||
[[Inflammation]] of the lungs, which can result when components of blood enter the tissue due to contusion, can also cause parts of the lung to collapse. [[Macrophage]]s, [[neutrophils]], and other [[White blood cell|inflammatory cell]]s and blood components can enter the lung tissue and release factors that lead to inflammation, increasing the likelihood of respiratory failure.<ref name=" | [[Inflammation]] of the lungs, which can result when components of blood enter the tissue due to contusion, can also cause parts of the lung to collapse. [[Macrophage]]s, [[neutrophils]], and other [[White blood cell|inflammatory cell]]s and blood components can enter the lung tissue and release factors that lead to inflammation, increasing the likelihood of respiratory failure.<ref name="pmid17019186">{{cite journal| author=Klein Y, Cohn SM, Proctor KG| title=Lung contusion: pathophysiology and management. | journal=Curr Opin Anaesthesiol | year= 2002 | volume= 15 | issue= 1 | pages= 65-8 | pmid=17019186 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17019186 }} </ref> In response to inflammation, excess [[mucus]] is produced, potentially plugging parts of the lung and leading to their collapse. Even when only one side of the chest is injured, inflammation may also affect the other lung.<ref name="pmid17019186">{{cite journal| author=Klein Y, Cohn SM, Proctor KG| title=Lung contusion: pathophysiology and management. | journal=Curr Opin Anaesthesiol | year= 2002 | volume= 15 | issue= 1 | pages= 65-8 | pmid=17019186 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17019186 }} </ref> Uninjured lung tissue may develop edema, thickening of the septa of the alveoli, and other changes. If this inflammation is severe enough, it can lead to dysfunction of the lungs like that seen in acute respiratory distress syndrome. | ||
===Ventilation/perfusion mismatch=== | ===Ventilation/perfusion mismatch=== | ||
Normally, the [[Ventilation/perfusion ratio|ratio of ventilation to perfusion]] is about one-to-one; the volume of air entering the alveoli ([[ventilation (physiology)|ventilation]]) is about equal to that of blood in the capillaries around them ([[perfusion]]). | Normally, the [[Ventilation/perfusion ratio|ratio of ventilation to perfusion]] is about one-to-one; the volume of air entering the alveoli ([[ventilation (physiology)|ventilation]]) is about equal to that of blood in the capillaries around them ([[perfusion]]). | ||
{{ | {{ | ||
cite journal |author=Prentice D, Ahrens T |title=Pulmonary complications of trauma |journal=Critical Care Nursing Quarterly |volume=17 |issue=2 |pages=24–33|year=1994 |month=August |pmid=8055358 | cite journal |author=Prentice D, Ahrens T |title=Pulmonary complications of trauma |journal=Critical Care Nursing Quarterly |volume=17 |issue=2 |pages=24–33|year=1994 |month=August |pmid=8055358 | ||
}} | }} | ||
</ref> This ratio is reduced in pulmonary contusion; fluid-filled alveoli cannot fill with air, oxygen does not fully saturate the [[hemoglobin]], and the blood leaves the lung without being fully oxygenated. | </ref> This ratio is reduced in pulmonary contusion; fluid-filled alveoli cannot fill with air, oxygen does not fully saturate the [[hemoglobin]], and the blood leaves the lung without being fully oxygenated. | ||
{{ | {{ | ||
cite book |author=Kishen R, Lomas G |chapter=Thoracic trauma |editor=Gwinnutt CL, Driscoll P |title=Trauma Resuscitation: The Team Approach|publisher=Informa Healthcare |year=2003 |isbn=1-85996-009-X |pages=55–64 | cite book |author=Kishen R, Lomas G |chapter=Thoracic trauma |editor=Gwinnutt CL, Driscoll P |title=Trauma Resuscitation: The Team Approach|publisher=Informa Healthcare |year=2003 |isbn=1-85996-009-X |pages=55–64 | ||
}} | }} | ||
</ref> Insufficient inflation of the lungs, which can result from inadequate mechanical ventilation or an associated injury such as flail chest, can also contribute to the ventilation/perfusion mismatch. | </ref> Insufficient inflation of the lungs, which can result from inadequate mechanical ventilation or an associated injury such as flail chest, can also contribute to the ventilation/perfusion mismatch. As the mismatch between ventilation and perfusion grows, blood oxygen saturation is reduced. Pulmonary hypoxic vasoconstriction, in which blood vessels near the hypoxic alveoli [[vasoconstriction|constrict]](narrow their diameter) in response to the lowered oxygen levels, can occur in pulmonary contusion. The [[vascular resistance]]increases in the contused part of the lung, leading to a decrease in the amount of blood that flows into it, directing blood to better-ventilated areas. Although reducing blood flow to the unventilated alveoli is a way to compensate for the fact that blood passing unventilated alveoli is not oxygenated, the oxygenation of the blood remains lower than normal. If it is severe enough, the hypoxemia resulting from fluid in the alveoli cannot be corrected just by giving supplemental oxygen; this problem is the cause of a large portion of the fatalities that result from trauma. | ||
===Associated injuries=== | ===Associated injuries=== | ||
[[Image:Pneumothorax hemothorax pneumomediastinum contusion.JPG|right|thumb|Severe pulmonary contusion with pneumothorax and hemothorax following severe chest trauma<ref name="Konijn08">{{cite journal |author=Konijn AJ, Egbers PH, Kuiper MA |title=Pneumopericardium should be considered with electrocardiogram changes after blunt chest trauma: a case report |journal=J Med Case Reports |volume=2 |issue= |pages=100 |year=2008 |pmid=18394149 |pmc=2323010|doi=10.1186/1752-1947-2-100 |url=http://www.jmedicalcasereports.com/content/2/1/100}}</ref>]] | [[Image:Pneumothorax hemothorax pneumomediastinum contusion.JPG|right|thumb|Severe pulmonary contusion with pneumothorax and hemothorax following severe chest trauma<ref name="Konijn08">{{cite journal |author=Konijn AJ, Egbers PH, Kuiper MA |title=Pneumopericardium should be considered with electrocardiogram changes after blunt chest trauma: a case report |journal=J Med Case Reports |volume=2 |issue= |pages=100 |year=2008 |pmid=18394149 |pmc=2323010|doi=10.1186/1752-1947-2-100 |url=http://www.jmedicalcasereports.com/content/2/1/100}}</ref>]] | ||
A large amount of force is required to cause pulmonary contusion; a person injured with such force is likely to have other types of injuries as well, | A large amount of force is required to cause pulmonary contusion; a person injured with such force is likely to have other types of injuries as well, and pulmonary contusion can be used to gauge the severity of trauma.<ref name="White99"> | ||
{{ | {{ | ||
cite book |author=Stern EJ, White C |title=Chest Radiology Companion |publisher=Lippincott Williams & Wilkins |location=Hagerstown, MD |year=1999 |pages=80|isbn=0-397-51732-7 | cite book |author=Stern EJ, White C |title=Chest Radiology Companion |publisher=Lippincott Williams & Wilkins |location=Hagerstown, MD |year=1999 |pages=80|isbn=0-397-51732-7 | ||
| Line 39: | Line 44: | ||
{{ | {{ | ||
cite journal |author=Klein Y, Cohn SM, Proctor KG |title=Lung contusion: Pathophysiology and management |journal=Current Opinion in Anaesthesiology|volume=15 |issue=1 |pages=65–68 |year=2002 |month=February |pmid=17019186|url=http://www.co-anesthesiology.com/pt/re/coanes/pdfhandler.00001503-200202000-00010.pdf|format=PDF }} | cite journal |author=Klein Y, Cohn SM, Proctor KG |title=Lung contusion: Pathophysiology and management |journal=Current Opinion in Anaesthesiology|volume=15 |issue=1 |pages=65–68 |year=2002 |month=February |pmid=17019186|url=http://www.co-anesthesiology.com/pt/re/coanes/pdfhandler.00001503-200202000-00010.pdf|format=PDF }} | ||
</ref> Flail chest is usually associated with pulmonary contusion, | </ref> Flail chest is usually associated with pulmonary contusion,<ref name="Johnson08"/> and the contusion, rather than the chest wall injury, is often the main cause of respiratory failure in people with these injuries.<ref name="Dohert05"> | ||
{{ | {{ | ||
cite book |author= Hemmila MR, Wahl WL |chapter= Management of the injured patient |editor=Doherty GM |title=Current Surgical Diagnosis and Treatment|publisher=McGraw-Hill Medical |year=2005 |pages= 214 |isbn=0-07-142315-X | cite book |author= Hemmila MR, Wahl WL |chapter= Management of the injured patient |editor=Doherty GM |title=Current Surgical Diagnosis and Treatment|publisher=McGraw-Hill Medical |year=2005 |pages= 214 |isbn=0-07-142315-X | ||
}} | }} | ||
</ref> Other indications of [[Thorax|thoracic]] trauma may be associated, including [[sternal fracture|fracture of the sternum]] and bruising of the chest wall. | </ref> Other indications of [[Thorax|thoracic]] trauma may be associated, including [[sternal fracture|fracture of the sternum]] and bruising of the chest wall. Over half of fractures of the [[scapula]] are associated with pulmonary contusion. The contusion is frequently found underlying fracture sites. When accompanied by a fracture, it is usually concentrated into a specific location—the contusion is more diffuse when there is no fracture.<ref name="Johnson08">{{cite journal |author=Johnson SB |title=Tracheobronchial injury |journal= Seminars in Thoracic and Cardiovascular Surgery |volume=20 |issue=1 |pages=52–57 |year= 2008 |pmid=18420127 |doi=10.1053/j.semtcvs.2007.09.001 |url=}}</ref> [[Pulmonary laceration]]s may result from the same blunt or penetrating forces that cause pulmonary contusion. Lacerations can result in pulmonary hematomas; these are reported to develop in 4–11% of pulmonary contusions. | ||
==Prognosis== | ==Prognosis== | ||
Pulmonary contusion usually resolves itself | Pulmonary contusion usually resolves itself without causing permanent complications;<ref name="Collins07">{{cite book |author=Collins J, Stern EJ | title=Chest Radiology: The Essentials | isbn=0781763142 | publisher=Lippincott Williams & Wilkins | year=2007 | pages=120}}</ref> however it may also have long-term ill effects on respiratory function.<ref name="CohnZieg96">{{cite journal | author=Cohn SM, Zieg PM |title=Experimental pulmonary contusion: Review of the literature and description of a new porcine model | journal=Journal of Trauma |volume=41 | issue=3 |pages=565–571 | year=1996 | month=September | pmid=8810987 }}</ref> Most contusions resolve in five to seven days after the injury. Signs detectable by radiography are usually gone within 10 days after the injury—when they are not, other conditions, such as pneumonia, are the likely cause. Chronic lung disease correlates with the size of the contusion and can interfere with an individual's ability to return to work. [[Fibrosis]] of the lungs can occur, resulting in [[dyspnea]] (shortness of breath), low blood oxygenation, and reduced [[functional residual capacity]] for as long as six years after the injury. As late as four years post-injury, decreased functional residual capacity has been found in most pulmonary contusion patients studied.<ref name="pmid18420127">{{cite journal| author=Johnson SB| title=Tracheobronchial injury. | journal=Semin Thorac Cardiovasc Surg | year= 2008 | volume= 20 | issue= 1 | pages= 52-7 | pmid=18420127 | doi=10.1053/j.semtcvs.2007.09.001 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18420127 }} </ref> During the six months after pulmonary contusion, up to 90% of people suffer difficulty breathing.<ref name="pmid18420127">{{cite journal| author=Johnson SB| title=Tracheobronchial injury. | journal=Semin Thorac Cardiovasc Surg | year= 2008 | volume= 20 | issue= 1 | pages= 52-7 | pmid=18420127 | doi=10.1053/j.semtcvs.2007.09.001 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18420127 }} </ref> In some cases, dyspnea persists for an indefinite period. Contusion can also permanently reduce the compliance of the lungs.<ref name="O'Leary07">{{cite book| author=Heck HA, Levitzky MG | chapter=The respiratory system | editor=O'Leary JP, Tabuenca A, Capote LR | title=The The Physiologic Basis of Surgery |publisher=Lippincott Williams & Wilkins | location=Hagerstown, MD | year=2007 | pages=463 | isbn=0-7817-7138-2 }}</ref> | ||
==References== | ==References== | ||
{{reflist|2}} | {{reflist|2}} | ||
Latest revision as of 14:34, 25 September 2012
|
Pulmonary contusion Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Pulmonary contusion natural history On the Web |
|
American Roentgen Ray Society Images of Pulmonary contusion natural history |
|
Risk calculators and risk factors for Pulmonary contusion natural history |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Natural History
The severity ranges from mild to deadly—small contusions may have little or no impact on the patient's health—yet pulmonary contusion is the most common type of potentially lethal chest trauma. It occurs in 30–75% of severe chest injuries. With an estimated mortality rate of 14–40%, pulmonary contusion plays a key role in determining whether an individual will die or suffer serious ill effects as the result of trauma. Pulmonary contusion is usually accompanied by other injuries. Although associated injuries are often the cause of death, pulmonary contusion is thought to cause death directly in a quarter to half of cases. Children are at especially high risk for the injury because the relative flexibility of their bones prevents the chest wall from absorbing force from an impact, causing it to be transmitted instead to the lung. Pulmonary contusion is associated with complications including pneumonia and acute respiratory distress syndrome, and it can cause long-term respiratory disability.
Complications
Pulmonary contusion can result in respiratory failure—about half of such cases occur within a few hours of the initial trauma.[1] Other severe complications, including infections and acute respiratory distress syndrome (ARDS) occur in up to half of cases.[2] Elderly people and those who have heart, lung, or kidney disease prior to the injury are more likely to stay longer in hospital and have complications from the injury. Complications occur in 55% of people with heart or lung disease and 13% of those without.[3] Of people with pulmonary contusion alone, 17% develop ARDS, while 78% of people with at least two additional injuries develop the condition.[4] A larger contusion is associated with an increased risk. In one study, 82% of people with 20% or more of the lung volume affected developed ARDS, while only 22% of people with less than 20% did so.[5]

Pneumonia, another potential complication, develops in as many as 20% of people with pulmonary contusion.[6] Contused lungs are less able to remove bacteria than uninjured lungs, predisposing them to infection.[7] Intubation and mechanical ventilation further increase the risk of developing pneumonia; the tube is passed through the nose or mouth into the airways, potentially tracking bacteria from the mouth or sinuses into them. Also, intubation prevents coughing, which would clear bacteria-laden secretions from the airways, and secretions pool near the tube's cuff and allow bacteria to grow.[8] The sooner the endotracheal tube is removed, the lower the risk of pneumonia, but if it is removed too early and has to be put back in, the risk of pneumonia rises. People who are at risk for pulmonary aspiration (e.g. those with lowered level of consciousness due to head injuries) are especially likely to get pneumonia.[8] As with ARDS, the chances of developing pneumonia increase with the size of the contusion. Children and adults have been found to have similar rates of complication with pneumonia and ARDS.[2]
Bleeding and edema
In contusions, torn capillaries leak fluid into the tissues around them.[9] The membrane between alveoli and capillaries is torn; damage to thiscapillary–alveolar membrane and small blood vessels causes blood and fluids to leak into the alveoli and the interstitial space (the space surrounding cells) of the lung.[10] With more severe trauma, there is a greater amount of edema, bleeding, and tearing of the alveoli.[11] Pulmonary contusion is characterized by microhemorrhages (tiny bleeds) that occur when thealveoli are traumatically separated from airway structures and blood vessels. Blood initially collects in the interstitial space, and then edema occurs by an hour or two after injury. An area of in the contused lung is commonly surrounded by an area of edema. In normal gas exchange, carbon dioxide diffuses across the endothelium of the capillaries, the interstitial space, and across the alveolar epithelium; oxygen diffuses in the other direction. Fluid accumulation interferes with gas exchange,[12] and can cause the alveoli to fill with proteins and collapse due to edema and bleeding. The larger the area of the injury, the more severe respiratory compromise will be.
Consolidation and collapse
Pulmonary contusion can cause parts of the lung to consolidate, alveoli to collapse, and atelectasis (partial or total lung collapse) to occur.[13] Consolidation occurs when the parts of the lung that are normally filled with air fill with material from the pathological condition, such as blood.[14] Over a period of hours after the injury, the alveoli in the injured area thicken and may become consolidated. A decrease in the amount of surfactant produced also contributes to the collapse and consolidation of alveoli; inactivation of surfactant increases their surface tension. Reduced production of surfactant can also occur in surrounding tissue that was not originally injured.
Inflammation of the lungs, which can result when components of blood enter the tissue due to contusion, can also cause parts of the lung to collapse. Macrophages, neutrophils, and other inflammatory cells and blood components can enter the lung tissue and release factors that lead to inflammation, increasing the likelihood of respiratory failure.[3] In response to inflammation, excess mucus is produced, potentially plugging parts of the lung and leading to their collapse. Even when only one side of the chest is injured, inflammation may also affect the other lung.[3] Uninjured lung tissue may develop edema, thickening of the septa of the alveoli, and other changes. If this inflammation is severe enough, it can lead to dysfunction of the lungs like that seen in acute respiratory distress syndrome.
Ventilation/perfusion mismatch
Normally, the ratio of ventilation to perfusion is about one-to-one; the volume of air entering the alveoli (ventilation) is about equal to that of blood in the capillaries around them (perfusion).
Prentice D, Ahrens T (1994). "Pulmonary complications of trauma". Critical Care Nursing Quarterly. 17 (2): 24–33. PMID 8055358. Unknown parameter |month= ignored (help)
</ref> This ratio is reduced in pulmonary contusion; fluid-filled alveoli cannot fill with air, oxygen does not fully saturate the hemoglobin, and the blood leaves the lung without being fully oxygenated.
Kishen R, Lomas G (2003). "Thoracic trauma". In Gwinnutt CL, Driscoll P. Trauma Resuscitation: The Team Approach. Informa Healthcare. pp. 55–64. ISBN 1-85996-009-X.
</ref> Insufficient inflation of the lungs, which can result from inadequate mechanical ventilation or an associated injury such as flail chest, can also contribute to the ventilation/perfusion mismatch. As the mismatch between ventilation and perfusion grows, blood oxygen saturation is reduced. Pulmonary hypoxic vasoconstriction, in which blood vessels near the hypoxic alveoli constrict(narrow their diameter) in response to the lowered oxygen levels, can occur in pulmonary contusion. The vascular resistanceincreases in the contused part of the lung, leading to a decrease in the amount of blood that flows into it, directing blood to better-ventilated areas. Although reducing blood flow to the unventilated alveoli is a way to compensate for the fact that blood passing unventilated alveoli is not oxygenated, the oxygenation of the blood remains lower than normal. If it is severe enough, the hypoxemia resulting from fluid in the alveoli cannot be corrected just by giving supplemental oxygen; this problem is the cause of a large portion of the fatalities that result from trauma.
Associated injuries
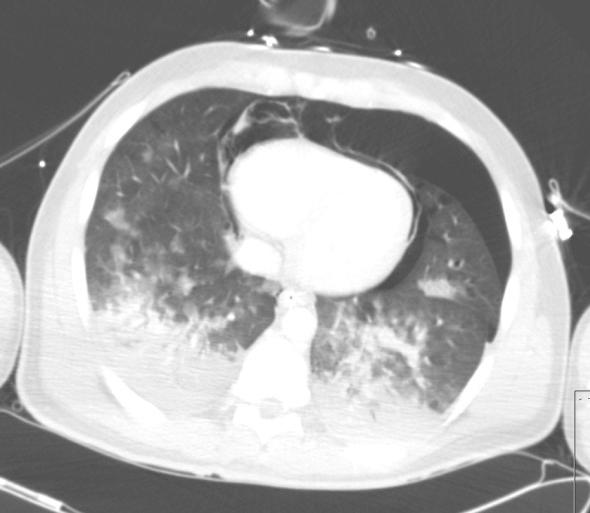
A large amount of force is required to cause pulmonary contusion; a person injured with such force is likely to have other types of injuries as well, and pulmonary contusion can be used to gauge the severity of trauma.[16] Up to three quarters of cases are accompanied by other chest injuries,[17] the most common of these being hemothorax and pneumothorax.[18] Flail chest is usually associated with pulmonary contusion,[19] and the contusion, rather than the chest wall injury, is often the main cause of respiratory failure in people with these injuries.[20] Other indications of thoracic trauma may be associated, including fracture of the sternum and bruising of the chest wall. Over half of fractures of the scapula are associated with pulmonary contusion. The contusion is frequently found underlying fracture sites. When accompanied by a fracture, it is usually concentrated into a specific location—the contusion is more diffuse when there is no fracture.[19] Pulmonary lacerations may result from the same blunt or penetrating forces that cause pulmonary contusion. Lacerations can result in pulmonary hematomas; these are reported to develop in 4–11% of pulmonary contusions.
Prognosis
Pulmonary contusion usually resolves itself without causing permanent complications;[21] however it may also have long-term ill effects on respiratory function.[22] Most contusions resolve in five to seven days after the injury. Signs detectable by radiography are usually gone within 10 days after the injury—when they are not, other conditions, such as pneumonia, are the likely cause. Chronic lung disease correlates with the size of the contusion and can interfere with an individual's ability to return to work. Fibrosis of the lungs can occur, resulting in dyspnea (shortness of breath), low blood oxygenation, and reduced functional residual capacity for as long as six years after the injury. As late as four years post-injury, decreased functional residual capacity has been found in most pulmonary contusion patients studied.[1] During the six months after pulmonary contusion, up to 90% of people suffer difficulty breathing.[1] In some cases, dyspnea persists for an indefinite period. Contusion can also permanently reduce the compliance of the lungs.[23]
References
- ↑ 1.0 1.1 1.2 Johnson SB (2008). "Tracheobronchial injury". Semin Thorac Cardiovasc Surg. 20 (1): 52–7. doi:10.1053/j.semtcvs.2007.09.001. PMID 18420127.
- ↑ 2.0 2.1 Allen GS, Cox CS (1998). "Pulmonary contusion in children: diagnosis and management". South Med J. 91 (12): 1099–106. PMID 9853720.
- ↑ 3.0 3.1 3.2 Klein Y, Cohn SM, Proctor KG (2002). "Lung contusion: pathophysiology and management". Curr Opin Anaesthesiol. 15 (1): 65–8. PMID 17019186.
- ↑ Miller DL, Mansour KA (2007). "Blunt traumatic lung injuries". Thorac Surg Clin. 17 (1): 57–61, vi. doi:10.1016/j.thorsurg.2007.03.017. PMID 17650697.
- ↑ Wanek S, Mayberry JC (2004). "Blunt thoracic trauma: flail chest, pulmonary contusion, and blast injury". Crit Care Clin. 20 (1): 71–81. PMID 14979330.
- ↑ Tovar JA (2008). "The lung and pediatric trauma". Semin Pediatr Surg. 17 (1): 53–9. doi:10.1053/j.sempedsurg.2007.10.008. PMID 18158142.
- ↑ Fry DE (2007). "Surgical infection". In O'Leary JP, Tabuenca A, Capote LR. The Physiologic Basis of Surgery. Hagerstown, MD: Lippincott Williams & Wilkins. p. 241. ISBN 0-7817-7138-2.
- ↑ 8.0 8.1 Sutyak JP, Wohltmann CD, Larson J (2007). "Pulmonary contusions and critical care management in thoracic trauma". Thorac Surg Clin. 17 (1): 11–23, v. doi:10.1016/j.thorsurg.2007.02.001. PMID 17650693.
- ↑ Fleisher GR, Ludwig S, Henretig FM, Ruddy RM, Silverman BK, ed. (2006). "Thoracic trauma". Textbook of Pediatric Emergency Medicine. Hagerstown, MD: Lippincott Williams & Wilkins. pp. 1434–1441. ISBN 0-7817-5074-1.
- ↑ Gavelli G, Canini R, Bertaccini P, Battista G, Bnà C, Fattori R (2002). "Traumatic injuries: imaging of thoracic injuries". Eur Radiol. 12 (6): 1273–94. doi:10.1007/s00330-002-1439-6. PMID 12042932.
- ↑ Ullman EA, Donley LP, Brady WJ (2003). "Pulmonary trauma emergency department evaluation and management". Emerg Med Clin North Am. 21 (2): 291–313. PMID 12793615.
- ↑ Bailey BJ, Johnson JT, Newlands SD, Calhoun KS, Deskin RW (2006). Head and Neck Surgery—Otolaryngology. Hagerstown, MD: Lippincott Williams & Wilkins. p. 929. ISBN 0-7817-5561-1.
- ↑ Keough V, Pudelek B (2001). "Blunt chest trauma: Review of selected pulmonary injuries focusing on pulmonary contusion". AACN Clinical Issues. 12 (2): 270–281. PMID 11759554.
- ↑ Collins CD, Hansell DM (1998). "Thoracic imaging". In Pryor JA, Webber BR. Physiotherapy for Respiratory and Cardiac Problems. Edinburgh: Churchill Livingstone. p. 35. ISBN 0-443-05841-5.
- ↑ Konijn AJ, Egbers PH, Kuiper MA (2008). "Pneumopericardium should be considered with electrocardiogram changes after blunt chest trauma: a case report". J Med Case Reports. 2: 100. doi:10.1186/1752-1947-2-100. PMC 2323010. PMID 18394149.
- ↑ Stern EJ, White C (1999). Chest Radiology Companion. Hagerstown, MD: Lippincott Williams & Wilkins. p. 80. ISBN 0-397-51732-7.
- ↑ Sutyak JP, Wohltmann CD, Larson J (2007). "Pulmonary contusions and critical care management in thoracic trauma". Thoracic Surgical Clinics. 17 (1): 11–23. doi:10.1016/j.thorsurg.2007.02.001. PMID 17650693.
- ↑
Klein Y, Cohn SM, Proctor KG (2002). "Lung contusion: Pathophysiology and management" (PDF). Current Opinion in Anaesthesiology. 15 (1): 65–68. PMID 17019186. Unknown parameter
|month=ignored (help) - ↑ 19.0 19.1 Johnson SB (2008). "Tracheobronchial injury". Seminars in Thoracic and Cardiovascular Surgery. 20 (1): 52&ndash, 57. doi:10.1053/j.semtcvs.2007.09.001. PMID 18420127.
- ↑ Hemmila MR, Wahl WL (2005). "Management of the injured patient". In Doherty GM. Current Surgical Diagnosis and Treatment. McGraw-Hill Medical. p. 214. ISBN 0-07-142315-X.
- ↑ Collins J, Stern EJ (2007). Chest Radiology: The Essentials. Lippincott Williams & Wilkins. p. 120. ISBN 0781763142.
- ↑ Cohn SM, Zieg PM (1996). "Experimental pulmonary contusion: Review of the literature and description of a new porcine model". Journal of Trauma. 41 (3): 565–571. PMID 8810987. Unknown parameter
|month=ignored (help) - ↑ Heck HA, Levitzky MG (2007). "The respiratory system". In O'Leary JP, Tabuenca A, Capote LR. The The Physiologic Basis of Surgery. Hagerstown, MD: Lippincott Williams & Wilkins. p. 463. ISBN 0-7817-7138-2.