Primary ciliary dyskinesia
| Primary ciliary dyskinesia | |
 | |
|---|---|
| ICD-10 | Q89.3 |
| ICD-9 | 759.3 |
| OMIM | 244400 242650 |
| DiseasesDB | 7111 Template:DiseasesDB2 |
| eMedicine | med/1220 ped/1166 |
| MeSH | D002925 |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Primary ciliary dyskinesia (PCD), also known as immotile ciliary syndrome or Kartagener Syndrome (KS), is a rare autosomal recessive genetic disorder caused by a defect in the action of the tiny hairs (cilia) lining the respiratory tract. Specifically, it is a defect in a gene coding for left-right dynein (lrd), a key structural protein in cilia.[1]
Classification
When accompanied by the triad of situs inversus (reversal of the internal organs), chronic sinusitis, and bronchiectasis, it is known as Kartagener syndrome. Use of immotile ciliary syndrome is no longer favoured, as sperm in affected men often have some motility - the term was coined in the mistaken belief that they had none.
Signs and symptoms
The main consequence of impaired ciliary function is reduced or absent mucus clearance in the lungs, and susceptibility to chronic, recurrent respiratory infections, including sinusitis, bronchitis, pneumonia, and otitis media. Susceptibility to these infections can be drastically reduced by an early diagnosis, as treatment with various chest physiotherapy techniques during childhood helps prevent the lungs being damaged or colonised by infection during this vulnerable period. Many patients experience hearing loss and show symptoms of glue ear which demonstrate variable responsiveness to the insertion of myringotomy tubes or grommets. A poor sense of smell accompanies high mucus production in the sinuses. Infertility is common, but IVF techniques have been successful for some parents with PCD. Clinical progression of the disease is variable with lung transplantation required in severe cases. For most patients, aggressive measures to enhance clearance of mucus, prevent respiratory infections, and treat bacterial super infections are recommended. Although the true incidence of the disease is unknown, it is estimated to be 1 in 32.000[2], although the actual incidence may be as high as 1 in 150.000.
Causes
This disease in genetically inherited. Both inner and/or outer dynein arms are dysfunction and thus the axoneme structure lacks the ability to move. Axonemes are the elongated structures that make up cilia and flagella. The dysfunction of the cilia begins during the embryologic phase of development. Since the cilia aid in the movement of growth factors resulting in the normal rotation of the internal organs during early embryological development, 50% of these individuals will develop situs inversus, as the laterality of the internal organs is determined by chance.
History
The classical triad was first described by A. K. Zivert in 1904 while Kartagener published his first report in 1933.
Diagnosis
Multi Sliced CT
-
CT image showing dilated and thickened medium sized airways (bronchiectasis)in a patient with Kartagener syndrome
-
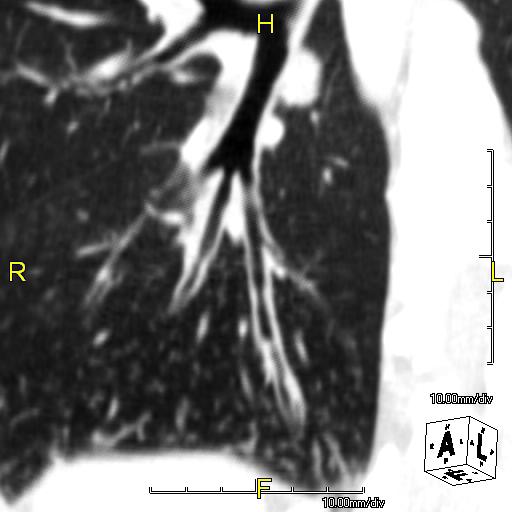
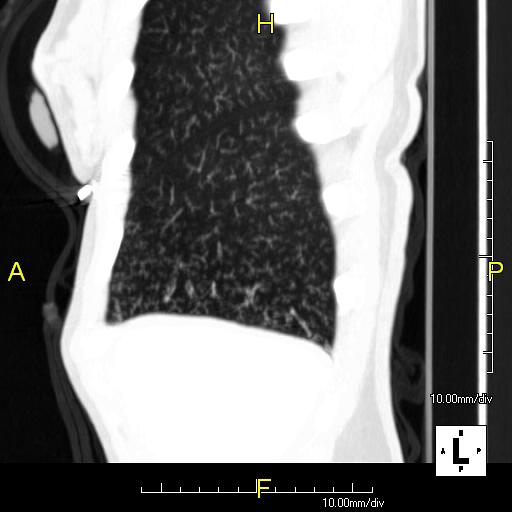
Oblique sagittal CT image showing lower lobe cylinidrical bronchiectasis in the same patient
-
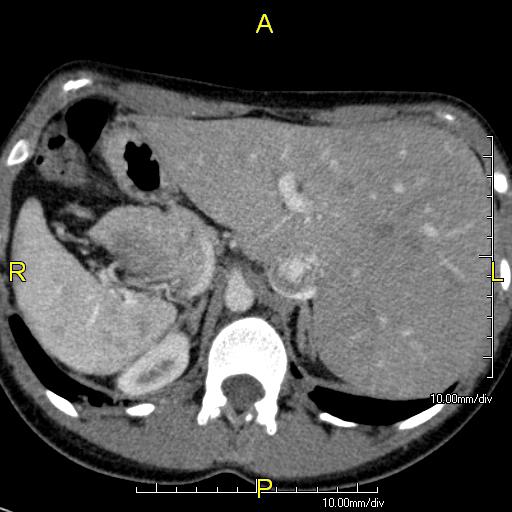
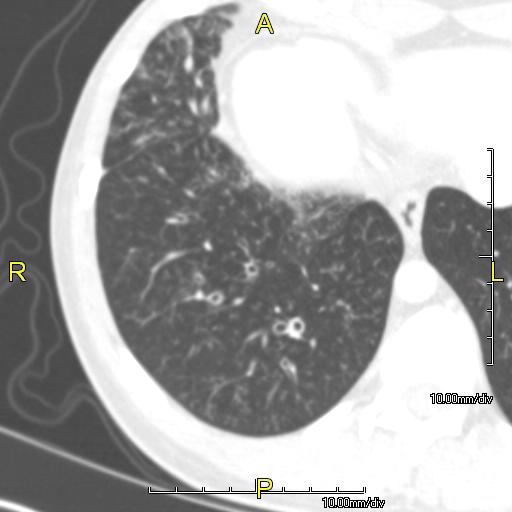
Axial CT image showing situs inversus with the liver and IVC on the left and the spleen and aorta on the right
-
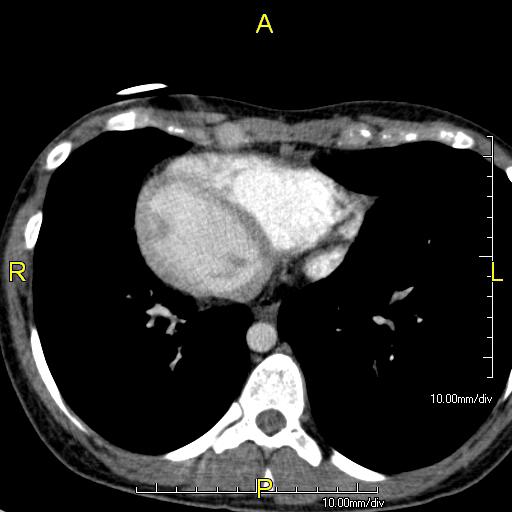
Axial CT image showing dextrocardia with the IVC and morphologic right ventricle on the left and the left ventricle on the right
-
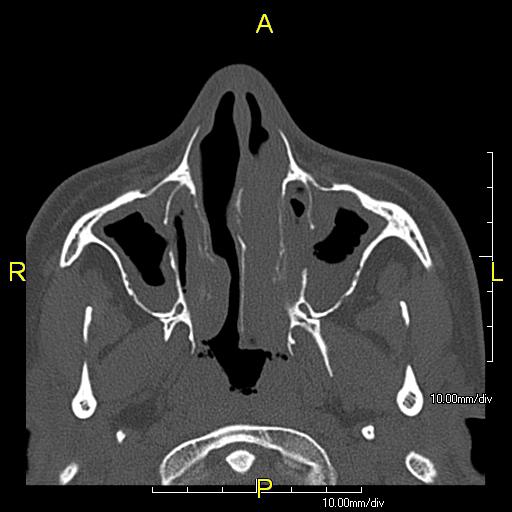
Axial CT image showing chronic sinusitis in a patient with Kartagener syndrome.
-
Sagittal CT image showing "tree in bud" appearance of mucous impaction in distal small airways related to primary ciliary dyskinesia
-
Situs inversus in a patient with Kartagener syndrome (Image courtesy of RadsWiki and copylefted)
Cardiac MRI
Images shown below are courtesy of RadsWiki and copylefted
-
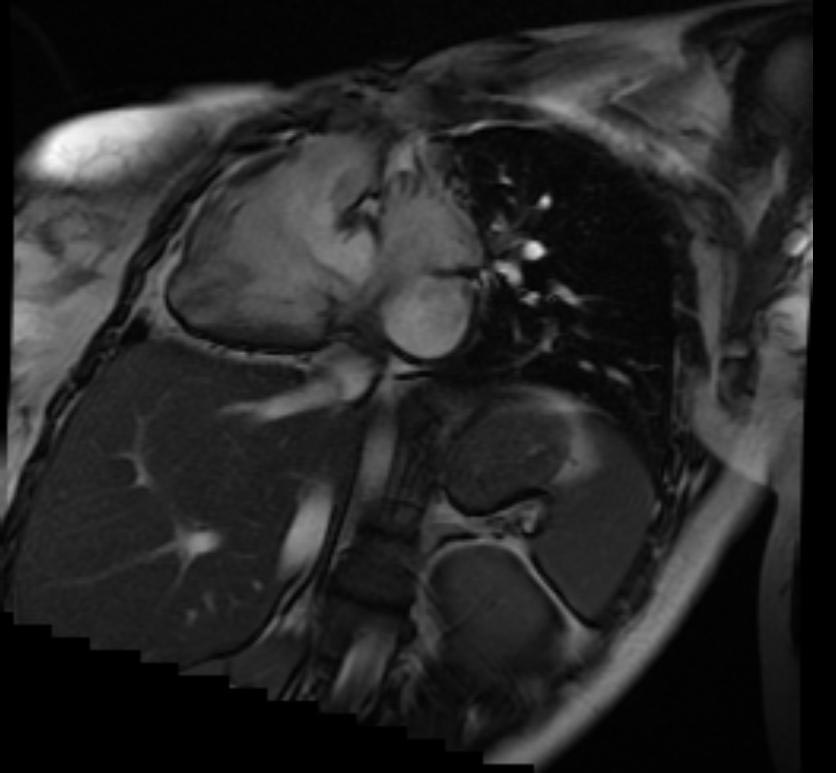
Dextrocardia in Kartagener syndrome
-
Dextrocardia in Kartagener syndrome
-
Dextrocardia in Kartagener syndrome
Footnotes
- ↑ Chodhari R, Mitchison HM, Meeks M. Cilia, primary ciliary dyskinesia and molecular genetics. Paediatr Respir Rev. 2004 Mar;5(1):69-76.
- ↑ Ceccaldi PF, Carre-Pigeon F, Youinou Y, Delepine B, Bryckaert PE, Harika G, Quereux C, Gaillard D. Kartagener's syndrome and infertility: observation, diagnosis and treatment J Gynecol Obstet Biol Reprod (Paris). 2004 May;33 (3):192-4.
References
- Zivert, A.K. Über einen Fall von Bronchiectasie bei einem Patienten mit situs inversus viscerum. Berliner klinische Wochenschrift, 1904, 41: 139-141.
- Kartagener, M. Zur Pathogenese der Bronchiektasien: Bronchiektasien bei Situs viscerum inversus. Beiträge zur Klinik der Tuberkulose, 1933, 83: 489-501.
- Afzelius, B., 1976. A human syndrome caused by immotile cilia. Science 193, 317–319.
- Coren ME, Meeks M, Morrison I, Buchdahl RM, Bush A. Primary ciliary dyskinesia: age at diagnosis and symptom history. Acta Paediatr. 2002; 91 (6):667-9.
- Ann S. Fulcher, and Mary Ann Turner. Abdominal Manifestations of Situs Anomalies in Adults. RadioGraphics 2002 22: 1439-1456.
Videos
- {{#ev:youtube|EKW9kVqorN0}}
External links
- http://www.pcdfoundation.org
- http://www.pcdsupport.org.uk
- http://www.med.unc.edu/cystfib/PCD.htm
- http://www.cheo.on.ca/english/9301c.shtml
- http://health.groups.yahoo.com/group/kartagener_syndrome/
- http://www.pcdforum.com/
- Kartagener's syndrome on Who Named It
This article contains some text from the public domain source "National Heart, Lung, and Blood Institute Rare Diseases Report FY 2001" available at http://www.nhlbi.nih.gov/resources/docs/raredisrpt01.htm Please adapt as necessary.