Mitral regurgitation resident survival guide: Difference between revisions
No edit summary |
No edit summary |
||
| Line 84: | Line 84: | ||
:❑ [[Crackles]] or [[rales]] <br> | :❑ [[Crackles]] or [[rales]] <br> | ||
❑ [[Cardiogenic shock physical examination|Signs and symptoms of cardiogenic shock]]: <BR> | ❑ [[Cardiogenic shock physical examination|Signs and symptoms of cardiogenic shock]]: <BR> | ||
:❑ [[Tachycardia]] <br> | |||
:❑ [[Hypotension]]<br> | |||
:❑ [[Altered mental status]]<br> | :❑ [[Altered mental status]]<br> | ||
:❑ [[Oliguria]]<br> | :❑ [[Oliguria]]<br> | ||
:❑ [[Diaphoresis]] | :❑ [[Diaphoresis]] | ||
:❑ [[ | :❑ [[Cold extremities]] | ||
:❑ [[ | :❑ [[Peripheral cyanosis]] | ||
:❑ [[Mottling]] | |||
</div>}} | </div>}} | ||
{{familytree | | | | | | | |,|-|^|-|.| | | | |}} | {{familytree | | | | | | | |,|-|^|-|.| | | | |}} | ||
| Line 96: | Line 98: | ||
{{familytree | | | | | | | |!| | | A02 | | | | | | A02= [[Mitral regurgitation resident survival guide#Complete Diagnostic Approach|'''Continue with complete diagnostic approach below''']]}} | {{familytree | | | | | | | |!| | | A02 | | | | | | A02= [[Mitral regurgitation resident survival guide#Complete Diagnostic Approach|'''Continue with complete diagnostic approach below''']]}} | ||
{{familytree |boxstyle=background: #FA8072; color: #F8F8FF;| | | | | | A01 | | | | | | A01=<div style="float: left; text-align: left; width: 25em; padding:1em;"> '''Initiate resuscitative measures:'''<br> | {{familytree |boxstyle=background: #FA8072; color: #F8F8FF;| | | | | | A01 | | | | | | A01=<div style="float: left; text-align: left; width: 25em; padding:1em;"> '''Initiate resuscitative measures:'''<br> | ||
❑ Secure airway <br> | ❑ Secure airway <br> | ||
❑ O2 <br> | ❑ Administer O2 <br> | ||
❑ 2 wide bore IV access <br> | ❑ Establish 2 wide bore IV access <br> | ||
❑ | ❑ Establish an arterial line<br> | ||
❑ ECG monitor<br> | ❑ Connect to ECG monitor<br> | ||
❑ Monitor vitals continuously<br> | ❑ Monitor vitals continuously<br> | ||
❑ ICU admission<br> | ❑ Consider ICU admission<br> | ||
❑ Consider [[mechanical ventilation|<span style="color:white;">mechanical ventilation</span>]]<br> | ❑ Consider [[mechanical ventilation|<span style="color:white;">mechanical ventilation</span>]]<br> | ||
❑ Consider [[pulmonary artery catheterization|<span style="color:white;">pulmonary artery catheterization</span>]] | ❑ Consider [[pulmonary artery catheterization|<span style="color:white;">pulmonary artery catheterization</span>]] | ||
---- | ---- | ||
'''Order imaging and blood tests (urgent):'''<br> | '''Order imaging and blood tests (urgent):'''<br> | ||
❑ [[Transthoracic echocardiography|<span style="color:white;">Transthoracic echocardiography</span>]] ([[TTE|<span style="color:white;">TTE</span>]])<br> | ❑ [[Transthoracic echocardiography|<span style="color:white;">Transthoracic echocardiography</span>]] ([[TTE|<span style="color:white;">TTE</span>]])<br> | ||
❑ [[Chest X-ray|<span style="color:white;">Chest X-ray</span>]]<br> | ❑ [[Chest X-ray|<span style="color:white;">Chest X-ray</span>]]<br> | ||
❑ [[CBC|<span style="color:white;">CBC</span>]] <br> | ❑ [[CBC|<span style="color:white;">CBC</span>]] <br> | ||
❑ [[Serum electrolytes|<span style="color:white;">Serum electrolytes</span>]]<br> | ❑ [[Serum electrolytes|<span style="color:white;">Serum electrolytes</span>]]<br> | ||
❑ [[Blood cultures|<span style="color:white;">Blood cultures</span>]] (in case of fever) <br> | |||
❑ Serum cardiac [[troponin|<span style="color:white;">troponin</span>]] I and T <br> | ❑ Serum cardiac [[troponin|<span style="color:white;">troponin</span>]] I and T <br> | ||
❑ [[Creatine kinase|<span style="color:white;">Creatine kinase</span>]] (CK-MB) <br> | ❑ [[Creatine kinase|<span style="color:white;">Creatine kinase</span>]] (CK-MB) <br> | ||
| Line 118: | Line 119: | ||
</div>}} | </div>}} | ||
{{familytree | | | | | | | |!| | | | | | }} | {{familytree | | | | | | | |!| | | | | | }} | ||
{{familytree |boxstyle=background: #FA8072; color: #F8F8FF;| | | | | | A01 | | | | | A01= | {{familytree |boxstyle=background: #FA8072; color: #F8F8FF;| | | | | | A01 | | | | | A01='''Does the patient has any evidence of MR in TTE?'''}} | ||
{{familytree | | | | | |,|-|^|-|.| | | | }} | {{familytree | | | | | |,|-|^|-|.| | | | }} | ||
{{familytree |boxstyle=background: #FA8072; color: #F8F8FF;| | | | A01 | | A02 | | | A01=Yes| A02=No}} | {{familytree |boxstyle=background: #FA8072; color: #F8F8FF;| | | | A01 | | A02 | | | A01=Yes| A02=No}} | ||
{{familytree | | | | | |!| | | |!| | | | }} | {{familytree | | | | | |!| | | |!| | | | }} | ||
{{familytree |boxstyle=background: #FA8072; color: #F8F8FF;| | | | A01 | | A02 | | | A01= <div style="text-align: left; width: 18em; padding: 1em;"> | {{familytree |boxstyle=background: #FA8072; color: #F8F8FF;| | | | A01 | | A02 | | | A01= <div style="text-align: left; width: 18em; padding: 1em;"> | ||
'''Initiate medical | '''Stabilize the patient:'''<br> | ||
❑ Initiate medical stabilization: | |||
:❑ [[Vasodilator|<span style="color:white;">Vasodilator</span>]] (IV [[nitroprusside|<span style="color:white;">nitroprusside</span>]]) '''PLUS''' inotropic agents (IV [[dobutamine|<span style="color:white;">dobutamine</span>]]) <br> | |||
❑ Establish [[intra-aortic balloon pump|<span style="color:white;">intra-aortic balloon pump</span>]]:<br> | |||
:❑ If medical therapy is not effective to maintain hemodynamic stability<br> | |||
---- | ---- | ||
'''Initiate treatment for specific etiologies:'''<br> | |||
❑ [[Aspirin|<span style="color:white;">Aspirin</span>]] in case of myocardial infarction<br> | ❑ [[Aspirin|<span style="color:white;">Aspirin</span>]] in case of myocardial infarction<br> | ||
❑ Antibiotics in case of [[Infective endocarditis resident survival guide|<span style="color:white;">infective endocarditis</span>]] | ❑ Antibiotics in case of [[Infective endocarditis resident survival guide|<span style="color:white;">infective endocarditis</span>]] | ||
</div>| A02= <div style="text-align: left; width: 18em; padding: 1em;">'''Consider other possible diagnosis:'''<br> | |||
❑ [[Acute respiratory distress syndrome|<span style="color:white;">Acute respiratory distress syndrome</span>]] | ❑ [[Acute respiratory distress syndrome|<span style="color:white;">Acute respiratory distress syndrome</span>]] | ||
❑ [[Sepsis|<span style="color:white;">Sepsis</span>]]<br> | ❑ [[Sepsis|<span style="color:white;">Sepsis</span>]]<br> | ||
</div>}} | </div>}} | ||
{{familytree | | | | | |!| | | | | | }} | {{familytree | | | | | |!| | | | | | }} | ||
{{familytree |boxstyle=background: #FA8072; color: #F8F8FF;| | | | A01 | | | | | | A01= <div style="text-align: left; width: 18em; padding: 1em;">'''Does the patient have any findings on TTE that require mitral valve surgery | {{familytree |boxstyle=background: #FA8072; color: #F8F8FF;| | | | A01 | | | | | | A01= <div style="text-align: left; width: 18em; padding: 1em;">'''Does the patient have any findings on TTE that require mitral valve surgery?'''<br> | ||
❑ Flail mitral leaflet (papillary muscle or chordal rupture)<br> | ❑ Flail mitral leaflet (papillary muscle or chordal rupture)<br> | ||
❑ Any signs of [[endocarditis|<span style="color:white;">endocarditis</span>]] <br> | ❑ Any signs of [[endocarditis|<span style="color:white;">endocarditis</span>]] <br> | ||
| Line 148: | Line 147: | ||
{{familytree |boxstyle=background: #FA8072; color: #F8F8FF;| | A01 | | A02 | | | | A01=Yes| A02=No}} | {{familytree |boxstyle=background: #FA8072; color: #F8F8FF;| | A01 | | A02 | | | | A01=Yes| A02=No}} | ||
{{familytree | | | |!| | | |!| | | | | }} | {{familytree | | | |!| | | |!| | | | | }} | ||
{{familytree |boxstyle=background: #FA8072; color: #F8F8FF;| | A01 | | A02 | | | | A01=<div style="text-align: left; width: 18em; padding: 1em;">''' | {{familytree |boxstyle=background: #FA8072; color: #F8F8FF;| | A01 | | A02 | | | | A01=<div style="text-align: left; width: 18em; padding: 1em;">'''Perform mitral valve surgery:'''<br> | ||
❑ [[Mitral valve repair|<span style="color:white;">Mitral valve repair</span>]]: <br> | ❑ [[Mitral valve repair|<span style="color:white;">Mitral valve repair</span>]]: <br> | ||
:❑ Most preferred | :❑ Most preferred | ||
:❑ Done in absence of [[papillary muscle|<span style="color:white;">papillary muscle</span>]] necrosis | :❑ Done in absence of [[papillary muscle|<span style="color:white;">papillary muscle</span>]] necrosis | ||
❑ [[Mitral valve replacement|<span style="color:white;">Mitral valve replacement</span>]]: | ❑ [[Mitral valve replacement|<span style="color:white;">Mitral valve replacement</span>]]: | ||
:❑ | :❑ Performed in cases of complex MR with extensive tissue destruction | ||
:❑ | :❑ Performed in cases of MR with lateral LV wall motion abnormality | ||
</div>| A02=<div style="text-align: left; width: 18em; padding: 1em;">''' | </div>| A02=<div style="text-align: left; width: 18em; padding: 1em;">'''Perform reperfusion or revascularization:'''<br> | ||
---- | ---- | ||
❑ In patients with acute coronary syndrome, [[CABG|<span style="color:white;">CABG</span>]] or [[coronary angioplasty|<span style="color:white;">coronary angioplasty</span>]] should be performed<br> | |||
❑ Early reperfusion for [[myocardial infarction|<span style="color:white;">myocardial infarction</span>]] can reduce localized [[LV|<span style="color:white;">LV</span>]] remodeling and hence [[MR|<span style="color:white;">MR</span>]] | ❑ Early reperfusion for [[myocardial infarction|<span style="color:white;">myocardial infarction</span>]] can reduce localized [[LV|<span style="color:white;">LV</span>]] remodeling and hence [[MR|<span style="color:white;">MR</span>]] | ||
</div>}} | </div>}} | ||
{{familytree | | | |!| | | | | | | | }} | {{familytree | | | |!| | | | | | | | }} | ||
{{familytree |boxstyle=background: #FA8072; color: #F8F8FF;| | A01 | | | | | | A01=<div style="text-align: left; width: 18em; padding: 1em;">''' | {{familytree |boxstyle=background: #FA8072; color: #F8F8FF;| | A01 | | | | | | A01=<div style="text-align: left; width: 18em; padding: 1em;">'''Perform reperfusion or revascularization:'''<br> | ||
❑ Perform [[CABG|<span style="color:white;">CABG</span>]] or [[coronary angioplasty|<span style="color:white;">coronary angioplasty</span>]] at the time of mitral valve surgery in patients with myocardial infarction<br> | |||
❑ [[CABG|<span style="color:white;">CABG</span>]] or [[coronary angioplasty|<span style="color:white;">coronary angioplasty</span>]] | |||
---- | ---- | ||
'''Consider cardiac transplantation:'''<br> | |||
❑ On some occasions with no contraindication for surgery<br> | ❑ On some occasions with no contraindication for surgery<br> | ||
❑ | ❑ For patients with severe LV dysfunction | ||
</div>}} | </div>}} | ||
{{Family tree/end}} | {{Family tree/end}} | ||
==Complete Diagnostic Approach to Mitral Regurgitation== | ==Complete Diagnostic Approach to Mitral Regurgitation== | ||
A complete diagnostic approach should be carried out after a focused initial rapid evaluation is conducted and following initiation of any urgent intervention | A complete diagnostic approach should be carried out after a focused initial rapid evaluation is conducted and following initiation of any urgent intervention.<ref name="pmid24589852">{{cite journal| author=Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP, Guyton RA et al.| title=2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. | journal=Circulation | year= 2014 | volume= | issue= | pages= | pmid=24589852 | doi=10.1161/CIR.0000000000000029 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24589852 }} </ref>.<br> | ||
<span style="font-size:85%">'''Abbreviations:''' '''AF''': Atrial fibrillation; '''MR''': Mitral regurgitation; '''EKG''': Electrocardiogram; '''EF''': Ejection fraction; '''S1''': First heart sound; '''S2''': Second heart sound; '''S3''': Third heart sound; '''LV''': Left ventricle; '''MVP''': Mitral valve prolapse</span> <br> | <span style="font-size:85%">'''Abbreviations:''' '''AF''': Atrial fibrillation; '''MR''': Mitral regurgitation; '''EKG''': Electrocardiogram; '''EF''': Ejection fraction; '''S1''': First heart sound; '''S2''': Second heart sound; '''S3''': Third heart sound; '''LV''': Left ventricle; '''MVP''': Mitral valve prolapse</span> <br> | ||
{{family tree/start}} | {{family tree/start}} | ||
{{family tree| | | | | | | A01 | | | | | A01= <div style="float: left; text-align: left; width:25em; padding:1em;">'''Characterize the symptoms:'''<br> | {{family tree| | | | | | | A01 | | | | | A01= <div style="float: left; text-align: left; width:25em; padding:1em;">'''Characterize the symptoms:'''<br> | ||
'''Acute mitral regurgitation:''' | '''Acute mitral regurgitation:''' | ||
❑ '''Symptoms of [[shock]] and [[pulmonary edema]]:'''<br> | ❑ '''Symptoms of [[shock]] and [[pulmonary edema]]:'''<br> | ||
:❑ [[Shortness of breath]]<br> | :❑ [[Shortness of breath]]<br> | ||
| Line 201: | Line 195: | ||
---- | ---- | ||
'''Chronic mitral regurgitation:''' | '''Chronic mitral regurgitation:''' | ||
❑ [[Asymptomatic]] | ❑ [[Asymptomatic]] | ||
:❑ Typical in isolated mild to moderate [[MR]] | :❑ Typical in isolated mild to moderate [[MR]] | ||
:❑ Severe MR until there is [[left ventricular failure]], [[pulmonary hypertension]] or [[atrial fibrillation]] | :❑ Severe MR until there is [[left ventricular failure]], [[pulmonary hypertension]] or [[atrial fibrillation]] | ||
❑ '''Symptoms associated with decreased forward flow and increased backflow across mitral valve:'''<br> | ❑ '''Symptoms associated with decreased forward flow and increased backflow across mitral valve (left ventricular failure):'''<br> | ||
:❑ [[Exertional dyspnea]]<br> | :❑ [[Exertional dyspnea]]<br> | ||
:❑ [[Orthopnea]]<br> | :❑ [[Orthopnea]]<br> | ||
| Line 227: | Line 220: | ||
::❑ [[edema|Pedel edema]] | ::❑ [[edema|Pedel edema]] | ||
::❑ [[Abdominal pain]] ([[hepatomegaly]]) | ::❑ [[Abdominal pain]] ([[hepatomegaly]]) | ||
</div>}} | </div>}} | ||
{{family tree| | | | | | | |!| | | | | | }} | {{family tree| | | | | | | |!| | | | | | }} | ||
| Line 303: | Line 293: | ||
'''Abdominal system:''' <br> | '''Abdominal system:''' <br> | ||
❑ | ❑ Hepatojugular reflex<br> | ||
❑ [[Hepatomegaly]] <br> | ❑ [[Hepatomegaly]] <br> | ||
❑ [[Ascites]]<br> | ❑ [[Ascites]]<br> | ||
| Line 312: | Line 302: | ||
{{Family tree| | | | | | | |!| | | | | | }} | {{Family tree| | | | | | | |!| | | | | | }} | ||
{{Family tree| | | | | | | D01 | | | | | D01= <div style="float: left; text-align: left; width:25em; padding:1em;">'''Order [[electrocardiogram]] (urgent):''' | {{Family tree| | | | | | | D01 | | | | | D01= <div style="float: left; text-align: left; width:25em; padding:1em;">'''Order [[electrocardiogram]] (urgent):''' | ||
❑ In [[MR|acute MR]]<br> | ❑ In [[MR|acute MR]]<br> | ||
:❑ Mostly normal | :❑ Mostly normal | ||
| Line 322: | Line 311: | ||
:❑ Findings of [[Atrial fibrillation electrocardiogram|atrial fibrillation]] complication | :❑ Findings of [[Atrial fibrillation electrocardiogram|atrial fibrillation]] complication | ||
[[Image:P mitrale.gif|center|150px|thumb|Left atrial enlargement produces a broad, bifid P wave in lead II ('''P mitrale''')]] | [[Image:P mitrale.gif|center|150px|thumb|Left atrial enlargement produces a broad, bifid P wave in lead II ('''P mitrale''')]] | ||
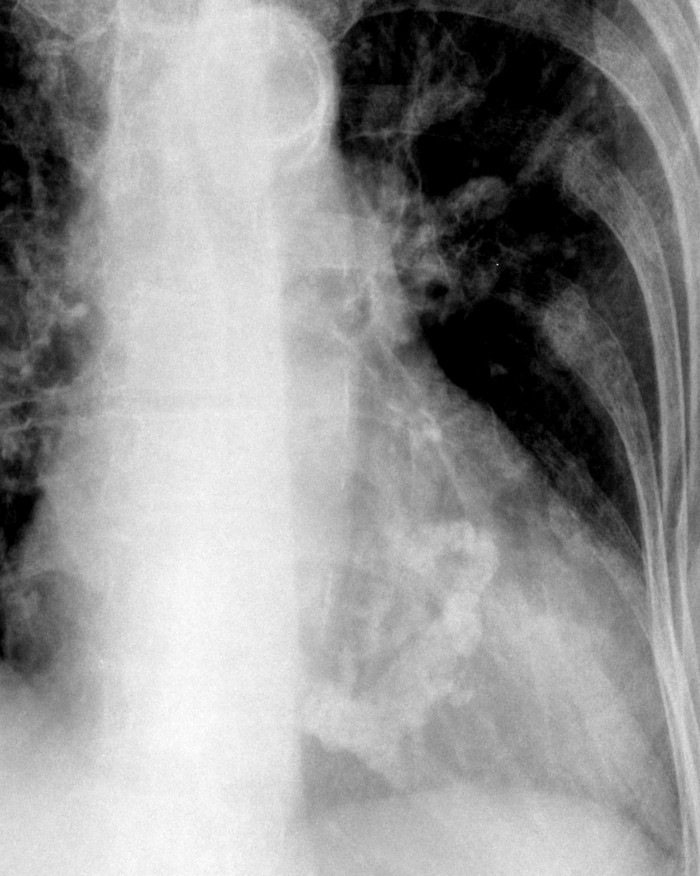
'''Order [[chest X-ray]] (urgent):'''<br> | '''Order [[chest X-ray]] (urgent):'''<br> | ||
❑ [[MR|Acute MR]]<br> | ❑ [[MR|Acute MR]]<br> | ||
:❑ Normal size cardiac silhouette | :❑ Normal size cardiac silhouette | ||
| Line 334: | Line 322: | ||
[[Image:mitral-valve02.jpg|150px|center|thumb|Calcification of the mitral annulus around the margins of the posterior leaflet forming a “C”]]<br clear="left"/> | [[Image:mitral-valve02.jpg|150px|center|thumb|Calcification of the mitral annulus around the margins of the posterior leaflet forming a “C”]]<br clear="left"/> | ||
'''Order [[transthoracic echocardiography]] ([[TTE]]) (urgent):'''<br> | '''Order [[transthoracic echocardiography]] ([[TTE]]) (urgent):'''<br> | ||
❑ Confirmatory<br> | ❑ Confirmatory<br> | ||
❑ To determine severity and assess hemodynamic consequences <br> | ❑ To determine severity and assess hemodynamic consequences <br> | ||
❑ To establish etiology<br> | ❑ To establish etiology<br> | ||
❑ To determine prognosis and evaluate for timing of intervention | ❑ To determine prognosis and evaluate for timing of intervention | ||
'''Order lab tests:'''<br> | '''Order lab tests:'''<br> | ||
❑ [[CBC]]<br> | ❑ [[CBC]]<br> | ||
❑ [[Electrolytes]] <br> | ❑ [[Electrolytes]] <br> | ||
| Line 349: | Line 335: | ||
❑ [[Troponin|Serum cardiac troponin I and T]] <br> | ❑ [[Troponin|Serum cardiac troponin I and T]] <br> | ||
❑ [[Creatine kinase]] (CK-MB) <br> | ❑ [[Creatine kinase]] (CK-MB) <br> | ||
❑ [[Blood cultures]] (in case of fever) <br> | |||
❑ Serum [[urea]] and [[creatinine]] <br> | ❑ Serum [[urea]] and [[creatinine]] <br> | ||
'''Other tests'''<br> | '''Other tests:'''<br> | ||
❑ [[Transesophageal echocardiography]] ([[TEE]] if [[TTE]] is equivocal)<br> | ❑ [[Transesophageal echocardiography]] ([[TEE]] if [[TTE]] is equivocal)<br> | ||
❑ [[Cardiac catheterization]]:<br> | ❑ [[Cardiac catheterization]]:<br> | ||
| Line 364: | Line 350: | ||
❑ [[MRI|Cardiac MRI]]<br> | ❑ [[MRI|Cardiac MRI]]<br> | ||
:❑ To assess severity when there is a discrepancy between clinical findings and [[echocardiography]]</div>}} | :❑ To assess severity when there is a discrepancy between clinical findings and [[echocardiography]]</div>}} | ||
{{familytree | | | | | | | |!| | | | | | | | | | | | | | | | | | | | | | }} | |||
{{familytree | | | | | | | A01 | | | | | | | | | | | | | | | | | | | | A01='''Does the patient has acute or chronic [[MR]]?'''}} | |||
{{Family tree| | | |,|-|-|-|^|-|-|-|.| | }} | {{Family tree| | | |,|-|-|-|^|-|-|-|.| | }} | ||
{{Family tree| | | F01 | | | | | | F02 | | | F01=<div style="float: left; text-align: left; width:25em; padding:1em;">'''Cardinal findings | {{Family tree| | | F01 | | | | | | F02 | | | F01=<div style="float: left; text-align: left; width:25em; padding:1em;">'''Acute MR (Cardinal findings suggestive of [[MR|acute mitral regurgitation]])'''<br> | ||
❑ Sudden onset and rapid progression of [[pulmonary edema]]<br> | ❑ Sudden onset and rapid progression of [[pulmonary edema]]<br> | ||
❑ [[Cardiogenic shock physical examination|Signs and symptoms of cardiogenic shock]] <BR> | ❑ [[Cardiogenic shock physical examination|Signs and symptoms of cardiogenic shock]] <BR> | ||
| Line 376: | Line 364: | ||
:❑ Reduced EF | :❑ Reduced EF | ||
:❑ Ruptured mitral [[chordae tendinae]] (flail leaflet) | :❑ Ruptured mitral [[chordae tendinae]] (flail leaflet) | ||
:❑ Ruptured [[papillary muscle]]</div>| F02=<div style="float: left; text-align: left; width:25em; padding:1em;">''' | :❑ Ruptured [[papillary muscle]]</div>| F02=<div style="float: left; text-align: left; width:25em; padding:1em;">'''Chronic MR (cardinal findings suggestive of [[MR|chronic mitral regurgitation]])'''<br> | ||
❑ Asymptomatic to chronic symptoms<br> | ❑ Asymptomatic to chronic symptoms<br> | ||
❑ Pre-existing [[heart disease]]<br> | ❑ Pre-existing [[heart disease]]<br> | ||
| Line 387: | Line 375: | ||
:❑ Preserved to decreased [[EF]]</div>}} | :❑ Preserved to decreased [[EF]]</div>}} | ||
{{familytree | | | | | | | | | | | |!| | | | | | | | | | | | | | | | | | | | | | }} | {{familytree | | | | | | | | | | | |!| | | | | | | | | | | | | | | | | | | | | | }} | ||
{{familytree | | | | | | | | | | | F02 | | | | | | | | | | | | | | | | | | | | | F02=[[ | {{familytree | | | | | | | | | | | F02 | | | | | | | | | | | | | | | | | | | | | F02='''Does the [[mitral valve]] anatomy appear normal in [[TTE]]?'''}} | ||
{{Family tree| | | | | | | | | |,|-|^|-|.| |}} | {{Family tree| | | | | | | | | |,|-|^|-|.| |}} | ||
{{familytree | | | | | | | | | G01 | | G02 | | | | | | | | | | | | | | | | | | | G01= | {{familytree | | | | | | | | | G01 | | G02 | | | | | | | | | | | | | | | | | | | G01=Yes| G02=No}} | ||
{{familytree | | | | | | | | | |!| | | |!| | | | | | | | | | | | | | | | | | | | }} | {{familytree | | | | | | | | | |!| | | |!| | | | | | | | | | | | | | | | | | | | }} | ||
{{familytree | | | | | | | | | G01 | | G02 | | | | | | | | | | | | | | | | | | | | {{familytree | | | | | | | | | G01 | | G02 | | | | | | | | | | | | | | | | | | | G02=Chronic primary [[mitral regurgitation]]| G01=Chronic secondary [[mitral regurgitation]]}} | ||
{{familytree | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | }} | {{familytree | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | }} | ||
{{familytree/end}} | {{familytree/end}} | ||
| Line 398: | Line 386: | ||
===Treatment of Acute Mitral Regurgitation=== | ===Treatment of Acute Mitral Regurgitation=== | ||
Shown below is an algorithm summarizing the approach to the management of acute mitral regurgitation.<ref name="pmid19564568">{{cite journal| author=Stout KK, Verrier ED| title=Acute valvular regurgitation. | journal=Circulation | year= 2009 | volume= 119 | issue= 25 | pages= 3232-41 | pmid=19564568 | doi=10.1161/CIRCULATIONAHA.108.782292 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19564568 }} </ref><ref name="pmid24589852">{{cite journal| author=Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP, Guyton RA et al.| title=2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. | journal=Circulation | year= 2014 | volume= | issue= | pages= | pmid=24589852 | doi=10.1161/CIR.0000000000000029 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24589852 }} </ref>.<br> | Shown below is an algorithm summarizing the approach to the management of acute mitral regurgitation.<ref name="pmid19564568">{{cite journal| author=Stout KK, Verrier ED| title=Acute valvular regurgitation. | journal=Circulation | year= 2009 | volume= 119 | issue= 25 | pages= 3232-41 | pmid=19564568 | doi=10.1161/CIRCULATIONAHA.108.782292 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19564568 }} </ref><ref name="pmid24589852">{{cite journal| author=Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP, Guyton RA et al.| title=2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. | journal=Circulation | year= 2014 | volume= | issue= | pages= | pmid=24589852 | doi=10.1161/CIR.0000000000000029 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24589852 }} </ref>.<br> | ||
<span style="font-size:85%">'''Abbreviations:''' '''IE''': Infective endocarditis; '''LV''': Left ventricle; '''LVEF''': Left ventricular ejection fraction; '''MR''': Mitral regurgitation | <span style="font-size:85%">'''Abbreviations:''' '''IE''': Infective endocarditis; '''LV''': Left ventricle; '''LVEF''': Left ventricular ejection fraction; '''MR''': Mitral regurgitation </span> <br> | ||
{{familytree/start |summary=PE diagnosis Algorithm.}} | {{familytree/start |summary=PE diagnosis Algorithm.}} | ||
{{familytree | | | | | | | | B01 | | | | | | | | | | | | | | | | | | | | | | | |B01=<div style="float: left; text-align: left; width: 18em; padding:1em;">'''Does the patient has any signs of hemodynamic instability?''' <br> | |||
{{familytree | | | | | | | | B01 | | | | | | | | | | | | | | | | | | | | | | | |B01=<div style="float: left; text-align: left; width: 18em; padding:1em;">''' | |||
❑ Hemodynamic instability | ❑ Hemodynamic instability | ||
:❑ [[Hypotension]] | :❑ [[Hypotension]] | ||
| Line 413: | Line 399: | ||
{{familytree | | | | | C01 | | | | C02 | | | | | | | | | | | | | | | | | | | | |C01='''Yes'''<br>(unstable)|C02='''No'''<br>(stable)}} | {{familytree | | | | | C01 | | | | C02 | | | | | | | | | | | | | | | | | | | | |C01='''Yes'''<br>(unstable)|C02='''No'''<br>(stable)}} | ||
{{familytree | | | | | |!| | | | | |!| | | | | | | | | | | | | | | | | | | | | | }} | {{familytree | | | | | |!| | | | | |!| | | | | | | | | | | | | | | | | | | | | | }} | ||
{{familytree | | | | | D01 | | | | D02 | | | | | | | | | | | | | | | | | | | | |D01=<div style="float: left; text-align: left; width: 16em; padding:1em;"> ''' | {{familytree | | | | | D01 | | | | D02 | | | | | | | | | | | | | | | | | | | | |D01=<div style="float: left; text-align: left; width: 16em; padding:1em;"> '''Initiate resuscitative measures:'''<br> | ||
❑ Secure airway <br> | ❑ Secure airway <br> | ||
❑ O2 <br> | ❑ Administer O2 <br> | ||
❑ 2 wide bore IV access <br> | ❑ Establish 2 wide bore IV access <br> | ||
❑ | ❑ Establish an arterial line<br> | ||
❑ ECG monitor<br> | ❑ Connect to ECG monitor<br> | ||
❑ Monitor vitals continuously<br> | ❑ Monitor vitals continuously<br> | ||
❑ ICU admission | ❑ Consider ICU admission<br> | ||
❑ Consider [[Mechanical ventilation]]<br> | |||
❑ Consider [[Pulmonary artery catheterization]] | |||
❑ [[ | |||
❑ | |||
---- | ---- | ||
''' | '''Stabilize the patient:'''<br> | ||
❑ Initiate medical stabilization: | |||
❑ [[ | :❑ [[Vasodilator]] (IV [[nitroprusside]]) '''PLUS''' inotropic agents (IV [[dobutamine]]) <br> | ||
❑ [[ | ❑ Establish [[intra-aortic balloon pump]]:<br> | ||
:❑ If medical therapy is not effective to maintain hemodynamic stability<br> | |||
❑ O2 <br> | </div>| D02=<div style="float: left; text-align: left; width: 16em; padding:1em;"> '''Initiate resuscitative measures:'''<br> | ||
❑ 2 wide bore IV access <br> | ❑ Administer O2 <br> | ||
❑ Establish 2 wide bore IV access <br> | |||
❑ Connect to ECG monitor<br> | |||
❑ Monitor vitals continuously<br> | ❑ Monitor vitals continuously<br> | ||
---- | ---- | ||
'''Initiate medical therapy:'''<br> | '''Initiate medical therapy:'''<br> | ||
❑ [[Vasodilator]] therapy: IV [[nitroprusside]]<br></div>}} | ❑ [[Vasodilator]] therapy: IV [[nitroprusside]]<br></div>}} | ||
{{familytree | | | | | |`|-|-|v|-|-|'| | | | | | | | | | | | | | | | | | | | | | }} | {{familytree | | | | | |`|-|-|v|-|-|'| | | | | | | | | | | | | | | | | | | | | | }} | ||
| Line 447: | Line 429: | ||
{{familytree | | | | | |!| | | I02 | | I03 | | | | | | | | | | | | | | | | | | | | I02=[[MR]] due to heart failure exacerbation(functional [[MR]])| I03= [[MR]] due to [[IE]] (organic [[MR]])}} | {{familytree | | | | | |!| | | I02 | | I03 | | | | | | | | | | | | | | | | | | | | I02=[[MR]] due to heart failure exacerbation(functional [[MR]])| I03= [[MR]] due to [[IE]] (organic [[MR]])}} | ||
{{familytree | | | | | |!| | | |!| | | |!| | | | | | | | | | | | | | | | | | }} | {{familytree | | | | | |!| | | |!| | | |!| | | | | | | | | | | | | | | | | | }} | ||
{{familytree | | | | | E01 | | E02 | | E03 | | | | | | | | | | | | | | | | |E01=<div style="float: left; text-align: left; width: 16em; padding:1em;"> ''' | {{familytree | | | | | E01 | | E02 | | E03 | | | | | | | | | | | | | | | | |E01=<div style="float: left; text-align: left; width: 16em; padding:1em;"> '''Perform reperfusion or revascularization surgery:'''<br> | ||
❑ [[CABG]] or [[coronary angioplasty]] should be done for acute coronary syndrome <br> | |||
❑ [[CABG]] or [[coronary angioplasty]] <br> | |||
❑ Early reperfusion can reduce localized [[LV]] remodeling and hence [[MR]]<br> | ❑ Early reperfusion can reduce localized [[LV]] remodeling and hence [[MR]]<br> | ||
''' | '''Consider mitral valve surgery:'''<br> | ||
❑ Indications of mitral valve surgery in ischemic MR: | |||
❑ [[Papillary muscle rupture]]<br> | :❑ [[Papillary muscle rupture]]<br> | ||
❑ Moderate to severe [[ischemic MR]] who are undergoing [[CABG]]<br> | :❑ Moderate to severe [[ischemic MR]] who are undergoing [[CABG]]<br> | ||
❑ [[Mitral valve repair]]: <br> | ❑ [[Mitral valve repair]]: <br> | ||
:❑ Most preferred | :❑ Most preferred | ||
| Line 475: | Line 443: | ||
:❑ In complex [[MR]] with extensive destruction | :❑ In complex [[MR]] with extensive destruction | ||
:❑ Lateral [[LV]] wall motion abnormality | :❑ Lateral [[LV]] wall motion abnormality | ||
''' | '''Consider medical therapy:'''<br> | ||
❑ In cases of reduced LVEF (ischemic cardiomyopathy)<br> | |||
❑ Medications: <br> | |||
:❑ [[Angiotensin converting enzyme inhibitors]] | |||
:❑ [[Angiotensin II receptor blockers]]<br> | |||
:❑ [[Beta blockers]] | |||
'''Consider cardiac transplantation:'''<br> | |||
---- | ---- | ||
❑ On some occasions with no contraindication for surgery<br> | ❑ On some occasions with no contraindication for surgery<br> | ||
❑ In patients with severe [[LV]] dysfunction | ❑ In patients with severe [[LV]] dysfunction | ||
</div>| E02=<div style="float: left; text-align: left; width: em; padding:1em;">'''Initiate heart failure | </div>| E02=<div style="float: left; text-align: left; width: em; padding:1em;">'''Initiate treatment for heart failure:''' <br> | ||
❑ Click [[Acute heart failure resident survival guide|here]] for acute heart failure resident survival guide | ❑ Click [[Acute heart failure resident survival guide|here]] for acute heart failure resident survival guide | ||
:❑ [[ACE inhibitors]] or ([[ARBs]]) if LVEF is ≤ 40% | :❑ [[ACE inhibitors]] or ([[ARBs]]) if LVEF is ≤ 40% | ||
| Line 488: | Line 462: | ||
:❑ [[Diuretic ]]therapy | :❑ [[Diuretic ]]therapy | ||
:❑ IV [[vasodilators]] | :❑ IV [[vasodilators]] | ||
</div>| E03=<div style="float: left; text-align: left; width: 16em; padding:1em;"> | |||
'''Initiate medical therapy:'''<br> | '''Initiate medical therapy:'''<br> | ||
---- | ---- | ||
| Line 510: | Line 480: | ||
:❑ If less [[mitral valve]] destruction | :❑ If less [[mitral valve]] destruction | ||
</div>}} | </div>}} | ||
{{familytree | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | }} | {{familytree | | | | | | | | | |!| | | | | | | | | | | | | | | | | | | | | | | }} | ||
{{familytree | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | }} | {{familytree | | | | | | | | | A01 | | | | | | | | | | | | | | | | | | | | | | A01=Does the patient show any hemodynamic improvement to medical therapy }} | ||
{{familytree | | | | | | | |,|-|^|-|.| | | | | | | | | | | | | | | | | | | | | | }} | |||
{{familytree | | | | | | | A01 | | A02 | | | | | | | | | | | | | | | | | | | | A01=Yes|A02=No}} | |||
{{familytree | | | | | | | |!| | | |!| | | | | | | | | | | | | | | | | | | | | }} | |||
{{familytree | | | | | | | A01 | | A02 | | | | | | | | | | | | | | | | | | | | A01= Continue with the heart failure management and have appropriate follow ups to assess the severity of MR| A02=<div style="float: left; text-align: left; width: 16em; padding:1em;"> '''Consider mitral valve surgery:'''<br> | |||
❑ [[Mitral valve repair]]: <br> | |||
:❑ Most preferred | |||
❑ [[Mitral valve replacement]]: | |||
:❑ In cases of lateral [[LV]] wall motion abnormality | |||
</div>}} | |||
{{familytree/end}} | {{familytree/end}} | ||
Revision as of 20:37, 22 April 2014
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Raviteja Guddeti, M.B.B.S. [2]; Mugilan Poongkunran M.B.B.S [3]
| Mitral Regurgitation Resident Survival Guide Microchapters |
|---|
| Overview |
| Causes |
| FIRE |
| Complete Diagnostic Approach |
| Treatment |
| Do's |
| Don'ts |
Overview
Mitral regurgitation (MR) refers to a disorder of the heart in which the mitral valve fails to close properly during systole leading to leakage of blood from left ventricle to left atrium during systole and reduction in cardiac output. The symptoms associated with mitral regurgitation are depends on the phase of the disease process. Individuals with acute mitral regurgitation are often gravely ill with significant hemodynamic abnormalities due to decompensated congestive heart failure and low cardiac output that require urgent treatment, whereas individuals with chronic compensated mitral regurgitation may be asymptomatic, with a normal exercise tolerance and no evidence of heart failure.[1] The management of acute MR is mitral valve surgery in most cases, whereas the chronic MR management depends on whether the condition is chronic primary MR (the mitral valve is usually abnormal) or chronic secondary MR (the mitral valve is usually normal) and the severity of the valve anatomy.[2]
Causes
Life Threatening Causes
Life-threatening causes include conditions which may result in death or permanent disability within 24 hours if left untreated.
Common Causes
Acute Mitral Regurgitation
- Papillary muscle rupture:
- Ruptured mitral chordae tendinae:
- Acute rheumatic fever[3]
- Chest trauma[4]
- Mitral valve prolapse[5]
- Infective endocarditis
- Spontaneous rupture
Chronic Primary Mitral Regurgitation
Chronic Secondary Mitral Regurgitation
Click here for the complete list of causes.
FIRE: Focused Initial Rapid Evaluation
A Focused Initial Rapid Evaluation (FIRE) should be performed to identify patients in need of immediate intervention.
Boxes in salmon color signify that an urgent management is needed.
Abbreviations: ARBs: Angiotensin II receptor antagonist; CABG: Coronary artery bypass surgery; HF: Heart failure; IE: Infective endocarditis; LVEF: Left ventricular ejection fraction; LV: Left ventricle; MR: Mitral regurgitation; S1: First heart sound; S2: Second heart sound
Identify cardinal findings that increase the pretest probability of mitral regurgitation: ❑ Murmur:
❑ Heart sounds: | |||||||||||||||||||||||||||||||||||||||
Does the patient have any of the following findings of acute mitral regurgitation with instability? ❑ Sudden onset and rapid progression of pulmonary edema:
| |||||||||||||||||||||||||||||||||||||||
| Yes | No | ||||||||||||||||||||||||||||||||||||||
| Continue with complete diagnostic approach below | |||||||||||||||||||||||||||||||||||||||
Initiate resuscitative measures: ❑ Secure airway Order imaging and blood tests (urgent): | |||||||||||||||||||||||||||||||||||||||
| Does the patient has any evidence of MR in TTE? | |||||||||||||||||||||||||||||||||||||||
| Yes | No | ||||||||||||||||||||||||||||||||||||||
Stabilize the patient:
❑ Establish intra-aortic balloon pump:
Initiate treatment for specific etiologies: | Consider other possible diagnosis: | ||||||||||||||||||||||||||||||||||||||
Does the patient have any findings on TTE that require mitral valve surgery? ❑ Flail mitral leaflet (papillary muscle or chordal rupture)
| |||||||||||||||||||||||||||||||||||||||
| Yes | No | ||||||||||||||||||||||||||||||||||||||
Perform mitral valve surgery:
| Perform reperfusion or revascularization: ❑ In patients with acute coronary syndrome, CABG or coronary angioplasty should be performed | ||||||||||||||||||||||||||||||||||||||
Perform reperfusion or revascularization: ❑ Perform CABG or coronary angioplasty at the time of mitral valve surgery in patients with myocardial infarction Consider cardiac transplantation: | |||||||||||||||||||||||||||||||||||||||
Complete Diagnostic Approach to Mitral Regurgitation
A complete diagnostic approach should be carried out after a focused initial rapid evaluation is conducted and following initiation of any urgent intervention.[2].
Abbreviations: AF: Atrial fibrillation; MR: Mitral regurgitation; EKG: Electrocardiogram; EF: Ejection fraction; S1: First heart sound; S2: Second heart sound; S3: Third heart sound; LV: Left ventricle; MVP: Mitral valve prolapse
Characterize the symptoms: Acute mitral regurgitation:
❑ Symptoms of shock and pulmonary edema:
❑ Symptoms suggestive of precipitating events:
Chronic mitral regurgitation: ❑ Asymptomatic
❑ Symptoms associated with decreased forward flow and increased backflow across mitral valve (left ventricular failure):
❑ Symptoms associated with complications:
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Obtain a detailed history: ❑ Past medical history:
❑ Family history: ❑ Medications: | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Examine the patient: Vital signs:
Skin: Cardiovascular system:
❑ Thrill (in acute MR and severe chronic MR)
Auscultation:
❑ Murmur
Respiratory system: Abdominal system: Neurological system: | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Order electrocardiogram (urgent):
❑ In acute MR
❑ In chronic MR
 Order chest X-ray (urgent):
 Order transthoracic echocardiography (TTE) (urgent): Order lab tests: Other tests:
❑ Exercise testing:
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Does the patient has acute or chronic MR? | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Acute MR (Cardinal findings suggestive of acute mitral regurgitation) ❑ Sudden onset and rapid progression of pulmonary edema
| Chronic MR (cardinal findings suggestive of chronic mitral regurgitation) ❑ Asymptomatic to chronic symptoms
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Does the mitral valve anatomy appear normal in TTE? | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Yes | No | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Chronic secondary mitral regurgitation | Chronic primary mitral regurgitation | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Treatment
Treatment of Acute Mitral Regurgitation
Shown below is an algorithm summarizing the approach to the management of acute mitral regurgitation.[1][2].
Abbreviations: IE: Infective endocarditis; LV: Left ventricle; LVEF: Left ventricular ejection fraction; MR: Mitral regurgitation
Does the patient has any signs of hemodynamic instability? ❑ Hemodynamic instability | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Yes (unstable) | No (stable) | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Initiate resuscitative measures: ❑ Secure airway Stabilize the patient:
❑ Establish intra-aortic balloon pump:
| Initiate resuscitative measures: ❑ Administer O2 Initiate medical therapy: | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Ischemic mitral regurgitation | Non-ischemic mitral regurgitation | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| MR due to heart failure exacerbation(functional MR) | MR due to IE (organic MR) | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Perform reperfusion or revascularization surgery: ❑ CABG or coronary angioplasty should be done for acute coronary syndrome Consider mitral valve surgery:
Consider medical therapy: Consider cardiac transplantation: ❑ On some occasions with no contraindication for surgery | Initiate treatment for heart failure: ❑ Click here for acute heart failure resident survival guide
| Initiate medical therapy: ❑ Click here for infective endocarditis resident survival guide and antimicrobial treatment Mitral valve surgery: ❑ Urgent surgery:
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Does the patient show any hemodynamic improvement to medical therapy | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Yes | No | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Continue with the heart failure management and have appropriate follow ups to assess the severity of MR | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Treatment of Chronic Mitral Regurgitation
Chronic Primary Mitral Regurgitation
Shown below is an algorithm summarizing the approach to the management of chronic primary mitral regurgitation.[2].
Abbreviations: AF: Atrial fibrillation; IE: Infective endocarditis; LVEF: Left ventricular ejection fraction; LVESD: Left ventricular end systolic dimension; MR: Mitral regurgitation; MVP: Mitral valve proplapse; PASP: Pulmonary artery systolic pressure; RHD: Rheumatic heart disease
| Chronic primary mitral regurgitation | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Severe MR: ❑ Etiologies:
❑ Left ventricular dilation | Progressive MR (Stage B): ❑ Etiologies: ❑ No Left ventricular dilation | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Symptomatic (Stage D) | Asymptomatic (Stage C) | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Initiate medical therapy:
❑ Beta blocker Mitral valve surgery:
Revascularisation: ❑ Concurrent coronary artery disease Anticoagulation therapy: ❑ Warfarin:
❑ Aspirin:
Endocarditis prophylaxis: ❑ Initiate infective endocarditis antimicrobial prophylaxis after mitral valve surgery | Mitral valve surgery: ❑ Performed in the following patients:
Revascularization: ❑ Concurrent coronary artery disease Periodic monitoring: ❑ In stage C1 patients with the following:
❑ Clinical evaluation:
Anticoagulation therapy: ❑ Warfarin:
❑ Aspirin:
Endocarditis prophylaxis: | Periodic monitoring: ❑ Clinical evaluation:
Anticoagulation therapy: ❑ Warfarin:
❑ Aspirin:
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Chronic Secondary Mitral Regurgitation
Shown below is an algorithm summarizing the approach to the management of chronic secondary mitral regurgitation.[2].
Abbreviations: AF: Atrial fibrillation; CAD: Coronary artery disease; HF: Heart failure; IE: Infective endocarditis; LV: Left ventricle; MR: Mitral regurgitation
| Chronic secondary mitral regurgitation | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Heart failure treatment: ❑ Click here for heart failure resident survival guide
| CAD treatment: ❑ Click here for coronary artery disease medical therapy ❑ Coronary angiography | Cardiac resynchronization therapy: ❑ Cardiac resynchronization therapy with biventricular pacing:
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Severe MR: ❑ Echo findings:
❑ LV dilation and systolic dysfunction due to primary myocardial disease | Progressive MR (Stage B): ❑ Echo findings:
❑ LV dilation and systolic dysfunction due to primary myocardial disease | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Stage D: Symptomatic (HF symptoms due to MR persist even after revascularization and medical therapy) | Stage C: Asymptomatic (HF and coronary ischemia symptoms respond to revascularization and medical herapy) | HF and coronary ischemia symptoms respond to revascularization and medical herapy | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Mitral valve surgery:
Anticoagulation therapy: ❑ Warfarin:
❑ Aspirin:
Endocarditis prophylaxis: | Periodic monitoring: ❑ Clinical evaluation:
Mitral valve surgery: ❑ Only in patients undergoing other cardiac surgery
Anticoagulation therapy: ❑ Warfarin:
❑ Aspirin:
Endocarditis prophylaxis: | Periodic monitoring: ❑ Clinical evaluation:
Mitral valve surgery: ❑ Only in patients undergoing other cardiac surgery
Anticoagulation therapy: ❑ Warfarin:
❑ Aspirin:
Endocarditis prophylaxis: | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Do's
- Always consult a multidisciplinary heart valve team for patients with acute MR, severe chronic MR and with multiple comorbidities.
- Consider vasodilator therapy in patients with chronic MR based upon the presence or absence of symptoms and the functional state of the left ventricle.
- Always consider patients with chronic MR who become symptomatic to be candidates for corrective mitral surgery.
- Perform mitral valve repair for patients with chronic severe primary MR limited to the posterior leaflet.
Don'ts
- Don't initiate vasodilator therapy for normotensive asymptomatic patients with chronic primary MR (stages B and C1) and normal systolic LV function.
- Don't recommend cardiovascular magnetic resonance (CMR) for routine diagnosis of MR.
- Don't prefer mitral valve repair to replacement to chronic severe primary MR patients involving the anterior leaflet or both leaflets when a successful and durable repair cannot be accomplished.
- Don't perform mitral valve replacement in patients with isolated severe primary MR limited to less than one half of the posterior leaflet unless mitral valve repair has been attempted and was unsuccessful.
- Don't perform coronary angiography before valve surgery in patients who are hemodynamically unstable.
- Avoid coronary angiography in patients of acute coronary syndrome complicated by severe acute mitral regurgitation.
References
- ↑ 1.0 1.1 Stout KK, Verrier ED (2009). "Acute valvular regurgitation". Circulation. 119 (25): 3232–41. doi:10.1161/CIRCULATIONAHA.108.782292. PMID 19564568.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP, Guyton RA; et al. (2014). "2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines". Circulation. doi:10.1161/CIR.0000000000000029. PMID 24589852.
- ↑ Anderson Y, Wilson N, Nicholson R, Finucane K (2008). "Fulminant mitral regurgitation due to ruptured chordae tendinae in acute rheumatic fever". J Paediatr Child Health. 44 (3): 134–7. doi:10.1111/j.1440-1754.2007.01214.x. PMID 17854408.
- ↑ Grinberg AR, Finkielman JD, Piñeiro D, Festa H, Cazenave C (1998). "Rupture of mitral chorda tendinea following blunt chest trauma". Clin Cardiol. 21 (4): 300–1. PMID 9580528.
- ↑ Grenadier E, Alpan G, Keidar S, Palant A (1983). "The prevalence of ruptured chordae tendineae in the mitral valve prolapse syndrome". Am Heart J. 105 (4): 603–10. PMID 6837414.
- ↑ Otto CM (2001). "Clinical practice. Evaluation and management of chronic mitral regurgitation". N Engl J Med. 345 (10): 740–6. doi:10.1056/NEJMcp003331. PMID 11547744.