Hepatoblastoma: Difference between revisions
Nima Nasiri (talk | contribs) |
Aditya Ganti (talk | contribs) |
||
| (30 intermediate revisions by one other user not shown) | |||
| Line 3: | Line 3: | ||
'''For patient information, click [[Hepatoblastoma (patient information)|here]]''' | '''For patient information, click [[Hepatoblastoma (patient information)|here]]''' | ||
{{Hepatoblastoma}} | {{Hepatoblastoma}} | ||
{{CMG}}; {{AE}} {{Nnasiri | {{CMG}}; {{AE}} {{Nnasiri}} | ||
{{SK}} Epithelial hepatoblastoma; Fetal hepatoblastoma; Embryonal hepatoblatoma; Macrotrabecular hepatoblastoma; Mixed hepatoblastoma; Rhabdoid hepatoblastoma; Small cell hepatoblastoma; Undifferentiated hepatoblastoma; Cholangioblastic hepatoblastoma; Teratoid hepatoblastoma; Chondroid hepatoblastoma; Osteoid hepatoblastoma; Rhabdomyoblastic hepatoblastoma; Neuroid-melanocytic hepatoblastoma; Well differentiated hepatoblastoma; HB | {{SK}} Epithelial hepatoblastoma; Fetal hepatoblastoma; Embryonal hepatoblatoma; Macrotrabecular hepatoblastoma; Mixed hepatoblastoma; Rhabdoid hepatoblastoma; Small cell hepatoblastoma; Undifferentiated hepatoblastoma; Cholangioblastic hepatoblastoma; Teratoid hepatoblastoma; Chondroid hepatoblastoma; Osteoid hepatoblastoma; Rhabdomyoblastic hepatoblastoma; Neuroid-melanocytic hepatoblastoma; Well differentiated hepatoblastoma; HB | ||
==Overview== | ==Overview== | ||
'''Hepatoblastoma''' is the most common primary [[liver tumor]] occurs in infant and children, usually less than 3 years old, more frequently in male, and accounting for over 1% of pediatric cancers. The [[etiology]] is unknown and not well understood, but it has been associated with [[Beckwith-Weidemann Syndrome|Beckwith-Weidemann]] syndrome, [[familial adenomatous polyposis]], and other factors such as [[low birth weight]], [[preeclampsia]], [[hemihypertrophy]]. The primary treatment is [[surgical]] resection, however, [[chemotherapy]] plays an important role by increasing the number of tumors that are respectable, [[chemotherapeutic agents]] helps in shrinkage of the tumor and make it easier to be resected by [[surgery]]. [[Prognosis]] of the tumor depends on various criteria such as resectability of the tumor, distant [[metastasis]], tumor size, PRETEXT [[Staging (pathology)|staging]], and recurrence of the tumor. The mainstay of treatment is [[surgery]], but the adjuvant [[Chemotherapeutic agent|chemotherapeutic]] agents and [[liver transplantation]] also are helpful. | '''Hepatoblastoma''' is the most common primary [[liver tumor]] occurs in infant and children, usually less than 3 years old, more frequently in [[male]], and accounting for over 1% of pediatric [[cancers]]. The [[etiology]] is unknown and not well understood, but it has been associated with [[Beckwith-Weidemann Syndrome|Beckwith-Weidemann]] syndrome, [[familial adenomatous polyposis]], and other factors such as [[low birth weight]], [[preeclampsia]], [[hemihypertrophy]]. The primary treatment is [[surgical]] resection, however, [[chemotherapy]] plays an important role by increasing the number of [[tumors]] that are respectable, [[chemotherapeutic agents]] helps in shrinkage of the [[tumor]] and make it easier to be resected by [[surgery]]. [[Prognosis]] of the [[tumor]] depends on various criteria such as resectability of the [[tumor]], distant [[metastasis]], tumor size, PRETEXT [[Staging (pathology)|staging]], and recurrence of the [[tumor]]. The mainstay of treatment is [[surgery]], but the [[adjuvant]] [[Chemotherapeutic agent|chemotherapeutic]] agents and [[liver transplantation]] also are helpful. | ||
==Historical Perspective== | ==Historical Perspective== | ||
In 1898, the first case of hepatoblastoma was published in English literature, the [[tumor]] was diagnosed in a 6-week old boy in Prague, by a physician named Misick, who found a large tumor on the [[autopsy]] of his [[liver]]. Decades later on 1962 Willis used the term, hepatoblastoma for this type of [[liver]] [[tumor]] because of it's [[Embryo|embryonal]] origin <ref name="pmid25336801">{{cite journal |vauthors=Aronson DC, Czauderna P, Maibach R, Perilongo G, Morland B |title=The treatment of hepatoblastoma: Its evolution and the current status as per the SIOPEL trials |journal=J Indian Assoc Pediatr Surg |volume=19 |issue=4 |pages=201–7 |date=October 2014 |pmid=25336801 |pmc=4204244 |doi=10.4103/0971-9261.142001 |url=}}</ref> | |||
==Classification== | ==Classification== | ||
*Hepatoblastoma are divided into | *Hepatoblastoma are divided into two broad categories:<ref name="pmid12228903">{{cite journal |vauthors=Rowland JM |title=Hepatoblastoma: assessment of criteria for histologic classification |journal=Med. Pediatr. Oncol. |volume=39 |issue=5 |pages=478–83 |date=November 2002 |pmid=12228903 |doi=10.1002/mpo.10171 |url=}}</ref><ref name="pmid24322718">{{cite journal |vauthors=Czauderna P, Lopez-Terrada D, Hiyama E, Häberle B, Malogolowkin MH, Meyers RL |title=Hepatoblastoma state of the art: pathology, genetics, risk stratification, and chemotherapy |journal=Curr. Opin. Pediatr. |volume=26 |issue=1 |pages=19–28 |date=February 2014 |pmid=24322718 |doi=10.1097/MOP.0000000000000046 |url=}}</ref> | ||
**[[Epithelial]] type (E-HB) | **[[Epithelial]] type (E-HB) | ||
***[[Fetal]], which has four subtypes: | ***[[Fetal]], which has four subtypes: | ||
****Well differentiated | ****Well differentiated | ||
****Crowded or | ****Crowded or [[mitotic]]<nowiki/>ally active | ||
****[[Pleomorphic]] | ****[[Pleomorphic]] | ||
****Poorly differentiated | ****Poorly differentiated | ||
| Line 25: | Line 25: | ||
***Macrotubular small cell [[undifferentiated]] (SCU) | ***Macrotubular small cell [[undifferentiated]] (SCU) | ||
***Cholangioblastic | ***Cholangioblastic | ||
**Mixed [[epithelial]] and [[mesenchymal]] type (MEM-HB). | **Mixed [[epithelial]] and [[mesenchymal]] type (MEM-HB). The mixed type is subdivided into: | ||
***[[Stromal]] derivatives | ***[[Stromal]] derivatives | ||
***[[Teratoid]] variants | ***[[Teratoma|Teratoid]] variants | ||
==Pathophysiology== | ==Pathophysiology== | ||
*The exact [[pathogenesis]] of hepatoblastoma is not fully understood. <ref name="pmid19619488">{{cite journal |vauthors=MacDonald BT, Tamai K, He X |title=Wnt/beta-catenin signaling: components, mechanisms, and diseases |journal=Dev. Cell |volume=17 |issue=1 |pages=9–26 |date=July 2009 |pmid=19619488 |pmc=2861485 |doi=10.1016/j.devcel.2009.06.016 |url=}}</ref> | *The exact [[pathogenesis]] of hepatoblastoma is not fully understood. <ref name="pmid19619488">{{cite journal |vauthors=MacDonald BT, Tamai K, He X |title=Wnt/beta-catenin signaling: components, mechanisms, and diseases |journal=Dev. Cell |volume=17 |issue=1 |pages=9–26 |date=July 2009 |pmid=19619488 |pmc=2861485 |doi=10.1016/j.devcel.2009.06.016 |url=}}</ref> | ||
*Loss of function [[mutations]] in [[APC]] leads to [[intracellular]] accumulation of the [[protooncogene]] [[beta-catenin]], which leads to [[germline]] mutation of [[Wnt signalling pathway|Wnt signal]] transduction and pathway. | *Loss of function [[mutations]] in [[APC]] leads to [[intracellular]] accumulation of the [[protooncogene]] [[beta-catenin]], which leads to [[germline]] [[mutation]] of [[Wnt signalling pathway|Wnt signal]] [[transduction]] and pathway. | ||
*Hepatoblastomas originate from primitive hepatic [[stem cells]]. | *Hepatoblastomas originate from primitive [[hepatic]] [[stem cells]]. | ||
*B-catenin [[mutations]] have been shown to be common in the majority of sporadic hepatoblastomas. | *[[Beta-catenin|B-catenin]] [[mutations]] have been shown to be common in the majority of [[sporadic]] hepatoblastomas. | ||
*Studies revealed that tumor occurs more often in families affected by [[familial adenomatous polyposis]]([[FAP]]), which is caused by inactivation of the [[adenomatous polyposis coli]]([[APC]]), a [[tumor-suppressor gene]] that [[down-regulate]] the amount of [[beta-catenin]]. | *Studies revealed that [[tumor]] occurs more often in families affected by [[familial adenomatous polyposis]]([[FAP]]), which is caused by inactivation of the [[adenomatous polyposis coli]] ([[APC]]), a [[tumor-suppressor gene]] that [[down-regulate]] the amount of [[beta-catenin]]. | ||
*[[Immunohistochemical]] markers such as expression of CK19, [[beta-catenin]] and EpCAM were correlated with | *[[Immunohistochemical]] markers such as expression of CK19, [[beta-catenin]] and EpCAM were correlated with [[tumor]] behaviour, response to [[chemotherapy]] and survival.<ref name="pmid29755772">{{cite journal |vauthors=Kiruthiga KG, Ramakrishna B, Saha S, Sen S |title=Histological and immunohistochemical study of hepatoblastoma: correlation with tumour behaviour and survival |journal=J Gastrointest Oncol |volume=9 |issue=2 |pages=326–337 |date=April 2018 |pmid=29755772 |pmc=5934143 |doi=10.21037/jgo.2018.01.08 |url=}}</ref> | ||
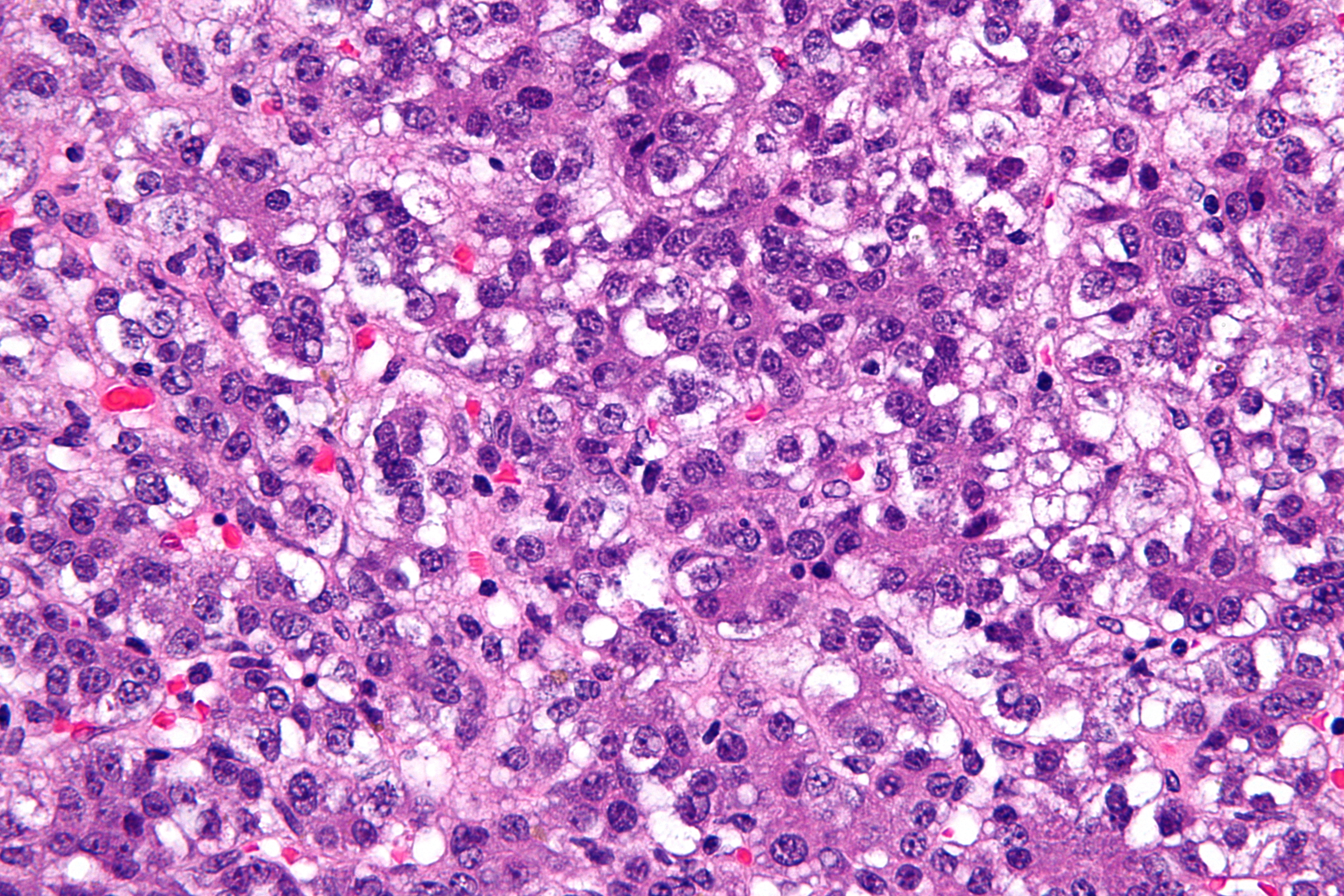
[[File:Hepatoblastoma.jpg|150px|thumb|left|Hepatoblastoma H&E[https://commons.wikimedia.org/wiki source:wikipedia]]]<br style="clear:left" /> | [[File:Hepatoblastoma.jpg|150px|thumb|left|Hepatoblastoma H&E[https://commons.wikimedia.org/wiki source:wikipedia]]]<br style="clear:left" /> | ||
==Causes== | ==Causes== | ||
*Underlying causes of hepatoblastoma poorly understood and most tumors are sporadic but there are some [[risk factors]] and conditions that have a strong association with this tumor such as:<ref name="pmid23558166">{{cite journal |vauthors=Heck JE, Meyers TJ, Lombardi C, Park AS, Cockburn M, Reynolds P, Ritz B |title=Case-control study of birth characteristics and the risk of hepatoblastoma |journal=Cancer Epidemiol |volume=37 |issue=4 |pages=390–5 |date=August 2013 |pmid=23558166 |pmc=3679264 |doi=10.1016/j.canep.2013.03.004 |url=}}</ref><ref name="pmid17425379">{{cite journal |vauthors=Finegold MJ, Lopez-Terrada DH, Bowen J, Washington MK, Qualman SJ |title=Protocol for the examination of specimens from pediatric patients with hepatoblastoma |journal=Arch. Pathol. Lab. Med. |volume=131 |issue=4 |pages=520–9 |date=April 2007 |pmid=17425379 |doi=10.1043/1543-2165(2007)131[520:PFTEOS]2.0.CO;2 |url=}}</ref><ref name="pmid30270492">{{cite journal |vauthors=Mussa A, Duffy KA, Carli D, Ferrero GB, Kalish JM |title=Defining an optimal time window to screen for hepatoblastoma in children with Beckwith-Wiedemann syndrome |journal=Pediatr Blood Cancer |volume=66 |issue=1 |pages=e27492 |date=January 2019 |pmid=30270492 |doi=10.1002/pbc.27492 |url=}}</ref> | *Underlying causes of hepatoblastoma poorly understood and most tumors are sporadic but there are some [[risk factors]] and conditions that have a strong association with this [[tumor]] such as:<ref name="pmid23558166">{{cite journal |vauthors=Heck JE, Meyers TJ, Lombardi C, Park AS, Cockburn M, Reynolds P, Ritz B |title=Case-control study of birth characteristics and the risk of hepatoblastoma |journal=Cancer Epidemiol |volume=37 |issue=4 |pages=390–5 |date=August 2013 |pmid=23558166 |pmc=3679264 |doi=10.1016/j.canep.2013.03.004 |url=}}</ref><ref name="pmid17425379">{{cite journal |vauthors=Finegold MJ, Lopez-Terrada DH, Bowen J, Washington MK, Qualman SJ |title=Protocol for the examination of specimens from pediatric patients with hepatoblastoma |journal=Arch. Pathol. Lab. Med. |volume=131 |issue=4 |pages=520–9 |date=April 2007 |pmid=17425379 |doi=10.1043/1543-2165(2007)131[520:PFTEOS]2.0.CO;2 |url=}}</ref><ref name="pmid30270492">{{cite journal |vauthors=Mussa A, Duffy KA, Carli D, Ferrero GB, Kalish JM |title=Defining an optimal time window to screen for hepatoblastoma in children with Beckwith-Wiedemann syndrome |journal=Pediatr Blood Cancer |volume=66 |issue=1 |pages=e27492 |date=January 2019 |pmid=30270492 |doi=10.1002/pbc.27492 |url=}}</ref> | ||
**[[Beckwith-Weidemann Syndrome|Beckwith-Weidemann syndrome]] | **[[Beckwith-Weidemann Syndrome|Beckwith-Weidemann syndrome]] | ||
**[[Familial adenomatous polyposis]] (FAP) | **[[Familial adenomatous polyposis]] (FAP) | ||
**[[Down syndrome]] | **[[Down syndrome]] | ||
**Edward syndrome ([[trisomy 18]]) | **[[Edward's syndrome|Edward syndrome]] ([[trisomy 18]]) | ||
**[[Nephroblastoma]], | **[[Nephroblastoma]], | ||
**[[Low birth weight]] infants are at higher risk of developing a hepatoblastoma | **[[Low birth weight]] infants are at higher risk of developing a hepatoblastoma | ||
| Line 59: | Line 59: | ||
==Differentiating hepatoblastoma from Other Diseases== | ==Differentiating hepatoblastoma from Other Diseases== | ||
*Hepatoblastoma must be differentiated from other diseases that cause rapidly enlarging abdominal mass in pediatrics such as:<ref name="pmid26835349">{{cite journal |vauthors=Hiyama E |title=Pediatric hepatoblastoma: diagnosis and treatment |journal=Transl Pediatr |volume=3 |issue=4 |pages=293–9 |date=October 2014 |pmid=26835349 |pmc=4728840 |doi=10.3978/j.issn.2224-4336.2014.09.01 |url=}}</ref> | *Hepatoblastoma must be differentiated from other diseases that cause rapidly enlarging abdominal mass in pediatrics such as:<ref name="pmid26835349">{{cite journal |vauthors=Hiyama E |title=Pediatric hepatoblastoma: diagnosis and treatment |journal=Transl Pediatr |volume=3 |issue=4 |pages=293–9 |date=October 2014 |pmid=26835349 |pmc=4728840 |doi=10.3978/j.issn.2224-4336.2014.09.01 |url=}}</ref> | ||
**[[Hepatocellular carcinoma]] ([[HCC]]) | **[[Hepatocellular carcinoma]] ([[HCC]]) of liver | ||
**[[Focal]] [[nodular]] [[hyperplasia]] | **[[Focal]] [[nodular]] [[hyperplasia]] of liver | ||
**[[Hepatic adenoma]] | **[[Hepatic adenoma]] of liver | ||
**[[Lymphoma]], and [[metastases]] | **[[Lymphoma]], and [[metastases]] to liver | ||
==Epidemiology and Demographics== | ==Epidemiology and Demographics== | ||
| Line 68: | Line 68: | ||
*The incidence/[[prevalence]] of hepatoblastoma is approximately 0.05–0.15 patients per 100000 population in children younger than 15 years.<ref name="pmid23600968">{{cite journal |vauthors=Allan BJ, Parikh PP, Diaz S, Perez EA, Neville HL, Sola JE |title=Predictors of survival and incidence of hepatoblastoma in the paediatric population |journal=HPB (Oxford) |volume=15 |issue=10 |pages=741–6 |date=October 2013 |pmid=23600968 |pmc=3791112 |doi=10.1111/hpb.12112 |url=}}</ref> | *The incidence/[[prevalence]] of hepatoblastoma is approximately 0.05–0.15 patients per 100000 population in children younger than 15 years.<ref name="pmid23600968">{{cite journal |vauthors=Allan BJ, Parikh PP, Diaz S, Perez EA, Neville HL, Sola JE |title=Predictors of survival and incidence of hepatoblastoma in the paediatric population |journal=HPB (Oxford) |volume=15 |issue=10 |pages=741–6 |date=October 2013 |pmid=23600968 |pmc=3791112 |doi=10.1111/hpb.12112 |url=}}</ref> | ||
*Peak [[incidence]] means of 18 months, mostly in [[infants]] and children younger than 3 years old, with a male predilection. | *Peak [[incidence]] means of 18 months, mostly in [[infants]] and children younger than 3 years old, with a male predilection. | ||
* | *Hepatoblastoma accounts for one percent of all primary [[malignancies]] in [[pediatrics]]. | ||
==Risk Factors== | ==Risk Factors== | ||
| Line 77: | Line 77: | ||
**[[Fetal distress]] | **[[Fetal distress]] | ||
**[[Premature labor]] | **[[Premature labor]] | ||
**[[Chromosomal anomalies]] such as [[Down syndrome]], [[ | **[[Chromosomal anomalies]] such as [[Down syndrome]], [[Edwards syndrome]]. | ||
**Parental [[tobacco]] [[smoking]] before and during [[pregnancy]] | **Parental [[tobacco]] [[smoking]] before and during [[pregnancy]] | ||
**[[Oxygen therapy]] | **[[Oxygen therapy]] | ||
**Certain medication ([[furosemide]]) | **Certain medication ([[furosemide]]) | ||
**[[Total parenteral nutrition]] ([[TPN]]) | **[[Total parenteral nutrition]] ([[TPN]]) | ||
==Screening== | ==Screening== | ||
*[[Ultrasound]] is the main | *There is no screening method for detecting hepatoblastoma. | ||
*[[Ultrasound]] is the main tool for suspected [[hepatic]] lesions in children.<ref name="pmid27526937">{{cite journal |vauthors=Shelmerdine SC, Roebuck DJ, Towbin AJ, McHugh K |title=MRI of paediatric liver tumours: How we review and report |journal=Cancer Imaging |volume=16 |issue=1 |pages=21 |date=August 2016 |pmid=27526937 |pmc=4986178 |doi=10.1186/s40644-016-0083-3 |url=}}</ref> | |||
*Serum [[alpha-fetoprotein]] ([[AFP]]) is the most important [[clinical]] marker of hepatoblastoma and helps to estimate [[malignant]] change, response to the treatment, and [[relapse]]. <ref name="pmid26835349">{{cite journal |vauthors=Hiyama E |title=Pediatric hepatoblastoma: diagnosis and treatment |journal=Transl Pediatr |volume=3 |issue=4 |pages=293–9 |date=October 2014 |pmid=26835349 |pmc=4728840 |doi=10.3978/j.issn.2224-4336.2014.09.01 |url=}}</ref> | *Serum [[alpha-fetoprotein]] ([[AFP]]) is the most important [[clinical]] marker of hepatoblastoma and helps to estimate [[malignant]] change, response to the treatment, and [[relapse]]. <ref name="pmid26835349">{{cite journal |vauthors=Hiyama E |title=Pediatric hepatoblastoma: diagnosis and treatment |journal=Transl Pediatr |volume=3 |issue=4 |pages=293–9 |date=October 2014 |pmid=26835349 |pmc=4728840 |doi=10.3978/j.issn.2224-4336.2014.09.01 |url=}}</ref> | ||
| Line 93: | Line 94: | ||
**[[Alpha-fetoprotein]] ([[AFP]]) levels, drop in [[Alpha-fetoprotein|AFP]] level after [[chemotherapy]] means better response to treatment. | **[[Alpha-fetoprotein]] ([[AFP]]) levels, drop in [[Alpha-fetoprotein|AFP]] level after [[chemotherapy]] means better response to treatment. | ||
**[[Histologic]] subtype, the well-differentiated [[fetal]] subtype has a better [[prognosis]] compared with small cell undifferentiated ones. | **[[Histologic]] subtype, the well-differentiated [[fetal]] subtype has a better [[prognosis]] compared with small cell undifferentiated ones. | ||
**Pretreatment extent of disease (PRETEXT) which was developed to stage the [[tumor]] before [[surgical]] removal and compare the [[efficacy]] of varous adjuvant [[chemotherapeutic agents]]. It is based on [[anatomy]] of [[liver]] and depending on tumor free sectors of [[liver]].<ref name="pmid15718322">{{cite journal |vauthors=Aronson DC, Schnater JM, Staalman CR, Weverling GJ, Plaschkes J, Perilongo G, Brown J, Phillips A, Otte JB, Czauderna P, MacKinlay G, Vos A |title=Predictive value of the pretreatment extent of disease system in hepatoblastoma: results from the International Society of Pediatric Oncology Liver Tumor Study Group SIOPEL-1 study |journal=J. Clin. Oncol. |volume=23 |issue=6 |pages=1245–52 |date=February 2005 |pmid=15718322 |doi=10.1200/JCO.2005.07.145 |url=}}</ref> | **Pretreatment extent of disease (PRETEXT) which was developed to stage the [[tumor]] before [[surgical]] removal and compare the [[efficacy]] of varous adjuvant [[chemotherapeutic agents]]. It is based on [[anatomy]] of [[liver]] and depending on [[tumor]] free sectors of [[liver]].<ref name="pmid15718322">{{cite journal |vauthors=Aronson DC, Schnater JM, Staalman CR, Weverling GJ, Plaschkes J, Perilongo G, Brown J, Phillips A, Otte JB, Czauderna P, MacKinlay G, Vos A |title=Predictive value of the pretreatment extent of disease system in hepatoblastoma: results from the International Society of Pediatric Oncology Liver Tumor Study Group SIOPEL-1 study |journal=J. Clin. Oncol. |volume=23 |issue=6 |pages=1245–52 |date=February 2005 |pmid=15718322 |doi=10.1200/JCO.2005.07.145 |url=}}</ref> | ||
*Complications of hepatoblastoma includes: | *Complications of hepatoblastoma includes: | ||
**[[Pancytopenia]] | **[[Pancytopenia]] | ||
| Line 109: | Line 110: | ||
*The majority of patients with hepatoblastoma have an [[abdominal mass]] or [[abdominal distension]]. <ref name="pmid26835349">{{cite journal |vauthors=Hiyama E |title=Pediatric hepatoblastoma: diagnosis and treatment |journal=Transl Pediatr |volume=3 |issue=4 |pages=293–9 |date=October 2014 |pmid=26835349 |pmc=4728840 |doi=10.3978/j.issn.2224-4336.2014.09.01 |url=}}</ref> | *The majority of patients with hepatoblastoma have an [[abdominal mass]] or [[abdominal distension]]. <ref name="pmid26835349">{{cite journal |vauthors=Hiyama E |title=Pediatric hepatoblastoma: diagnosis and treatment |journal=Transl Pediatr |volume=3 |issue=4 |pages=293–9 |date=October 2014 |pmid=26835349 |pmc=4728840 |doi=10.3978/j.issn.2224-4336.2014.09.01 |url=}}</ref> | ||
*Other symptoms of hepatoblastoma include: | *Other symptoms of hepatoblastoma include: | ||
**[[Abdominal discomfort]] | **[[Abdominal discomfort]] | ||
**Generalized [[Fatigue (medical)|fatigue]] | **Generalized [[Fatigue (medical)|fatigue]] | ||
**Loss of appetite ([[Anorexia]]) | **Loss of appetite ([[Anorexia]]) | ||
**[[Nausea]] and [[vomiting]] | **[[Nausea]] and [[vomiting]] | ||
| Line 122: | Line 123: | ||
===Laboratory Findings=== | ===Laboratory Findings=== | ||
*Laboratory findings that help with the diagnosis of hepatoblastoma includes:<ref name="pmid49416">{{cite journal |vauthors=Exelby PR, Filler RM, Grosfeld JL |title=Liver tumors in children in the particular reference to hepatoblastoma and hepatocellular carcinoma: American Academy of Pediatrics Surgical Section Survey--1974 |journal=J. Pediatr. Surg. |volume=10 |issue=3 |pages=329–37 |date=June 1975 |pmid=49416 |doi= |url=}}</ref> | *Laboratory findings that help with the diagnosis of hepatoblastoma includes:<ref name="pmid49416">{{cite journal |vauthors=Exelby PR, Filler RM, Grosfeld JL |title=Liver tumors in children in the particular reference to hepatoblastoma and hepatocellular carcinoma: American Academy of Pediatrics Surgical Section Survey--1974 |journal=J. Pediatr. Surg. |volume=10 |issue=3 |pages=329–37 |date=June 1975 |pmid=49416 |doi= |url=}}</ref> | ||
**High levels of [[Alpha-fetoprotein]] ([[AFP]]) | |||
**Mild [[liver]] function disturbances | |||
**[[Anemia]] on [[Complete blood counts|complete blood count]] | **[[Anemia]] on [[Complete blood counts|complete blood count]] | ||
**[[Thrombocytosis]] (more frequent because of the effect of [[thrombopoietin]])<ref name="pmid6153151">{{cite journal |vauthors=Nickerson HJ, Silberman TL, McDonald TP |title=Hepatoblastoma, thrombocytosis, and increased thrombopoietin |journal=Cancer |volume=45 |issue=2 |pages=315–7 |date=January 1980 |pmid=6153151 |doi= |url=}}</ref> | **[[Thrombocytosis]] (more frequent because of the effect of [[thrombopoietin]])<ref name="pmid6153151">{{cite journal |vauthors=Nickerson HJ, Silberman TL, McDonald TP |title=Hepatoblastoma, thrombocytosis, and increased thrombopoietin |journal=Cancer |volume=45 |issue=2 |pages=315–7 |date=January 1980 |pmid=6153151 |doi= |url=}}</ref> | ||
**[[Thrombocytopenia]](less common) | **[[Thrombocytopenia]] (less common) | ||
===Electrocardiogram=== | ===Electrocardiogram=== | ||
| Line 132: | Line 133: | ||
===X-ray=== | ===X-ray=== | ||
*[[Chest-X-Ray|Chest]] x-rays can be useful especially since this tumor has the affinity to [[metastasize]] to [[lungs]].<ref name="pmid11042582">{{cite journal |vauthors=Perilongo G, Brown J, Shafford E, Brock P, De Camargo B, Keeling JW, Vos A, Philips A, Pritchard J, Plaschkes J |title=Hepatoblastoma presenting with lung metastases: treatment results of the first cooperative, prospective study of the International Society of Paediatric Oncology on childhood liver tumors |journal=Cancer |volume=89 |issue=8 |pages=1845–53 |date=October 2000 |pmid=11042582 |doi= |url=}}</ref> | *[[Chest-X-Ray|Chest]] [[Chest X-ray|x-rays]] can be useful especially since this [[tumor]] has the affinity to [[metastasize]] to [[lungs]].<ref name="pmid11042582">{{cite journal |vauthors=Perilongo G, Brown J, Shafford E, Brock P, De Camargo B, Keeling JW, Vos A, Philips A, Pritchard J, Plaschkes J |title=Hepatoblastoma presenting with lung metastases: treatment results of the first cooperative, prospective study of the International Society of Paediatric Oncology on childhood liver tumors |journal=Cancer |volume=89 |issue=8 |pages=1845–53 |date=October 2000 |pmid=11042582 |doi= |url=}}</ref> | ||
=== | ===Ultrasound=== | ||
*Imaging studies play an important role in the diagnosis, [[Staging (pathology)|staging]], and treatment of disease, most tumors can be resected surgically and [[ultrasound]] is often used in order to detect tumor size, also the initial diagnosis is made by [[abdominal]] ultrasound. | *Imaging studies play an important role in the diagnosis, [[Staging (pathology)|staging]], and treatment of disease, most tumors can be resected surgically and [[ultrasound]] is often used in order to detect [[tumor]] size, also the initial diagnosis is made by [[abdominal]] [[ultrasound]]. | ||
===CT scan=== | ===CT scan=== | ||
*[[CT scan]] is very helpful to diagnose the disease, children with hepatoblastoma undergo either a CT or [[MRI]] scan at diagnosis. <ref name="pmid27955729">{{cite journal |vauthors=Aronson DC, Meyers RL |title=Malignant tumors of the liver in children |journal=Semin. Pediatr. Surg. |volume=25 |issue=5 |pages=265–275 |date=October 2016 |pmid=27955729 |doi=10.1053/j.sempedsurg.2016.09.002 |url=}}</ref> | *[[CT scan]] is very helpful to diagnose the disease, children with hepatoblastoma undergo either a CT or [[MRI]] scan at diagnosis. <ref name="pmid27955729">{{cite journal |vauthors=Aronson DC, Meyers RL |title=Malignant tumors of the liver in children |journal=Semin. Pediatr. Surg. |volume=25 |issue=5 |pages=265–275 |date=October 2016 |pmid=27955729 |doi=10.1053/j.sempedsurg.2016.09.002 |url=}}</ref> | ||
*Surgeons prefer an [[angiographic]] or [[biphasic]] [[CT scan]] because of better depiction of the [[hepatic]] arterial, [[portal]] venous and [[hepatic vein]] and other [[liver]] structures. | *Surgeons prefer an [[angiographic]] or [[biphasic]] [[CT scan]] because of better depiction of the [[hepatic]] arterial, [[portal]] venous and [[hepatic vein]] and other [[liver]] structures. | ||
*Concerns about [[radiation]] exposures in [[pediatrics]] has changed this modality in favor of [[MRI]], although [[MRI]] is much lengthy exam than CT has the advantage of multiplanar soft-tissue characterization, and when [[diffusion-weighted imaging]] techniques are used, [[MRI]] is exquisitely sensitive for detecting tiny liver lesions. | *Concerns about [[radiation]] exposures in [[pediatrics]] has changed this modality in favor of [[MRI]], although [[MRI]] is much lengthy exam than [[CT]] has the advantage of multiplanar [[soft-tissue]] characterization, and when [[diffusion-weighted imaging]] techniques are used, [[MRI]] is exquisitely sensitive for detecting tiny [[liver]] lesions. | ||
*[[Spiral CT scan]] findings of hypervascular lesions in the [[liver]] with delayed contrast excretion are highly suggestive of a malignant liver tumor. | *[[Spiral CT scan]] findings of hypervascular lesions in the [[liver]] with delayed contrast excretion are highly suggestive of a [[malignant]] [[liver]] [[tumor]]. | ||
===MRI=== | ===MRI=== | ||
| Line 156: | Line 157: | ||
===Medical Therapy=== | ===Medical Therapy=== | ||
*The mainstay of therapy for hepatoblastoma is [[Surgery|surger]]<nowiki/>y, however, the vast majority of the tumors cannot be completely resected because of their large size or [[metastasis]].<ref name="pmid26308249">{{cite journal |vauthors=Pham TA, Gallo AM, Concepcion W, Esquivel CO, Bonham CA |title=Effect of Liver Transplant on Long-term Disease-Free Survival in Children With Hepatoblastoma and Hepatocellular Cancer |journal=JAMA Surg |volume=150 |issue=12 |pages=1150–8 |date=December 2015 |pmid=26308249 |doi=10.1001/jamasurg.2015.1847 |url=}}</ref> | *The mainstay of therapy for hepatoblastoma is [[Surgery|surger]]<nowiki/>y, however, the vast majority of the tumors cannot be completely resected because of their large size or [[metastasis]].<ref name="pmid26308249">{{cite journal |vauthors=Pham TA, Gallo AM, Concepcion W, Esquivel CO, Bonham CA |title=Effect of Liver Transplant on Long-term Disease-Free Survival in Children With Hepatoblastoma and Hepatocellular Cancer |journal=JAMA Surg |volume=150 |issue=12 |pages=1150–8 |date=December 2015 |pmid=26308249 |doi=10.1001/jamasurg.2015.1847 |url=}}</ref> | ||
*Liver [[transplantation]] can be considered for tumors that cannot be removed by surgery.<ref name="pmid10839879">{{cite journal |vauthors=Reyes JD, Carr B, Dvorchik I, Kocoshis S, Jaffe R, Gerber D, Mazariegos GV, Bueno J, Selby R |title=Liver transplantation and chemotherapy for hepatoblastoma and hepatocellular cancer in childhood and adolescence |journal=J. Pediatr. |volume=136 |issue=6 |pages=795–804 |date=June 2000 |pmid=10839879 |doi= |url=}}</ref> | *Liver [[transplantation]] can be considered for [[tumors]] that cannot be removed by surgery.<ref name="pmid10839879">{{cite journal |vauthors=Reyes JD, Carr B, Dvorchik I, Kocoshis S, Jaffe R, Gerber D, Mazariegos GV, Bueno J, Selby R |title=Liver transplantation and chemotherapy for hepatoblastoma and hepatocellular cancer in childhood and adolescence |journal=J. Pediatr. |volume=136 |issue=6 |pages=795–804 |date=June 2000 |pmid=10839879 |doi= |url=}}</ref> | ||
*[[Chemotherapy]] is an important [[adjuvant therapy]], and cisplatin is the most commonly used [[chemotherapeutic agent]], it can reduce the volume of [[tumors]] that are too big for surgical removal.<ref name="pmid12778356">{{cite journal |vauthors=Häberle B, Bode U, von Schweinitz D |title=[Differentiated treatment protocols for high- and standard-risk hepatoblastoma--an interim report of the German Liver Tumor Study HB99] |language=German |journal=Klin Padiatr |volume=215 |issue=3 |pages=159–65 |date=2003 |pmid=12778356 |doi=10.1055/s-2003-39375 |url=}}</ref> | *[[Chemotherapy]] is an important [[adjuvant therapy]], and [[cisplatin]] is the most commonly used [[chemotherapeutic agent]], it can reduce the volume of [[tumors]] that are too big for surgical removal.<ref name="pmid12778356">{{cite journal |vauthors=Häberle B, Bode U, von Schweinitz D |title=[Differentiated treatment protocols for high- and standard-risk hepatoblastoma--an interim report of the German Liver Tumor Study HB99] |language=German |journal=Klin Padiatr |volume=215 |issue=3 |pages=159–65 |date=2003 |pmid=12778356 |doi=10.1055/s-2003-39375 |url=}}</ref> | ||
===Surgery=== | ===Surgery=== | ||
Latest revision as of 19:27, 13 March 2019
For patient information, click here
|
Hepatoblastoma Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Hepatoblastoma On the Web |
|
American Roentgen Ray Society Images of Hepatoblastoma |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Nima Nasiri, M.D.[2]
Synonyms and keywords: Epithelial hepatoblastoma; Fetal hepatoblastoma; Embryonal hepatoblatoma; Macrotrabecular hepatoblastoma; Mixed hepatoblastoma; Rhabdoid hepatoblastoma; Small cell hepatoblastoma; Undifferentiated hepatoblastoma; Cholangioblastic hepatoblastoma; Teratoid hepatoblastoma; Chondroid hepatoblastoma; Osteoid hepatoblastoma; Rhabdomyoblastic hepatoblastoma; Neuroid-melanocytic hepatoblastoma; Well differentiated hepatoblastoma; HB
Overview
Hepatoblastoma is the most common primary liver tumor occurs in infant and children, usually less than 3 years old, more frequently in male, and accounting for over 1% of pediatric cancers. The etiology is unknown and not well understood, but it has been associated with Beckwith-Weidemann syndrome, familial adenomatous polyposis, and other factors such as low birth weight, preeclampsia, hemihypertrophy. The primary treatment is surgical resection, however, chemotherapy plays an important role by increasing the number of tumors that are respectable, chemotherapeutic agents helps in shrinkage of the tumor and make it easier to be resected by surgery. Prognosis of the tumor depends on various criteria such as resectability of the tumor, distant metastasis, tumor size, PRETEXT staging, and recurrence of the tumor. The mainstay of treatment is surgery, but the adjuvant chemotherapeutic agents and liver transplantation also are helpful.
Historical Perspective
In 1898, the first case of hepatoblastoma was published in English literature, the tumor was diagnosed in a 6-week old boy in Prague, by a physician named Misick, who found a large tumor on the autopsy of his liver. Decades later on 1962 Willis used the term, hepatoblastoma for this type of liver tumor because of it's embryonal origin [1]
Classification
- Hepatoblastoma are divided into two broad categories:[2][3]
- Epithelial type (E-HB)
- Fetal, which has four subtypes:
- Well differentiated
- Crowded or mitotically active
- Pleomorphic
- Poorly differentiated
- Anaplastic
- Embryonal
- Macrotubular small cell undifferentiated (SCU)
- Cholangioblastic
- Fetal, which has four subtypes:
- Mixed epithelial and mesenchymal type (MEM-HB). The mixed type is subdivided into:
- Epithelial type (E-HB)
Pathophysiology
- The exact pathogenesis of hepatoblastoma is not fully understood. [4]
- Loss of function mutations in APC leads to intracellular accumulation of the protooncogene beta-catenin, which leads to germline mutation of Wnt signal transduction and pathway.
- Hepatoblastomas originate from primitive hepatic stem cells.
- B-catenin mutations have been shown to be common in the majority of sporadic hepatoblastomas.
- Studies revealed that tumor occurs more often in families affected by familial adenomatous polyposis(FAP), which is caused by inactivation of the adenomatous polyposis coli (APC), a tumor-suppressor gene that down-regulate the amount of beta-catenin.
- Immunohistochemical markers such as expression of CK19, beta-catenin and EpCAM were correlated with tumor behaviour, response to chemotherapy and survival.[5]
Causes
- Underlying causes of hepatoblastoma poorly understood and most tumors are sporadic but there are some risk factors and conditions that have a strong association with this tumor such as:[6][7][8]
- Beckwith-Weidemann syndrome
- Familial adenomatous polyposis (FAP)
- Down syndrome
- Edward syndrome (trisomy 18)
- Nephroblastoma,
- Low birth weight infants are at higher risk of developing a hepatoblastoma
- Preeclampsia
- Parental tobacco smoking
- Oxygen therapy
- Certain medication (furosemide)
- Radiation
- Total parenteral nutrition (TPN)
- The most common genetic mutation which plays role in etiology of sporadic cases include:[9]
- The Wnt signaling pathway which results in the accumulation of beta-catenin.
Differentiating hepatoblastoma from Other Diseases
- Hepatoblastoma must be differentiated from other diseases that cause rapidly enlarging abdominal mass in pediatrics such as:[10]
- Hepatocellular carcinoma (HCC) of liver
- Focal nodular hyperplasia of liver
- Hepatic adenoma of liver
- Lymphoma, and metastases to liver
Epidemiology and Demographics
- Hepatoblastoma is the most common primary liver cancer in infants and children, tumor involves right lobe of liver more often.[11]
- The incidence/prevalence of hepatoblastoma is approximately 0.05–0.15 patients per 100000 population in children younger than 15 years.[12]
- Peak incidence means of 18 months, mostly in infants and children younger than 3 years old, with a male predilection.
- Hepatoblastoma accounts for one percent of all primary malignancies in pediatrics.
Risk Factors
- Common risk factors in the development of hepatoblastoma include:[6]
- Low birth weight infants
- Preeclampsia
- Fetal distress
- Premature labor
- Chromosomal anomalies such as Down syndrome, Edwards syndrome.
- Parental tobacco smoking before and during pregnancy
- Oxygen therapy
- Certain medication (furosemide)
- Total parenteral nutrition (TPN)
Screening
- There is no screening method for detecting hepatoblastoma.
- Ultrasound is the main tool for suspected hepatic lesions in children.[13]
- Serum alpha-fetoprotein (AFP) is the most important clinical marker of hepatoblastoma and helps to estimate malignant change, response to the treatment, and relapse. [10]
Natural History, Complications, and Prognosis
- Prognosis is based on different factors including:[14][5]
- Age of diagnosis, younger children have a better prognosis.
- Metastases,
- Alpha-fetoprotein (AFP) levels, drop in AFP level after chemotherapy means better response to treatment.
- Histologic subtype, the well-differentiated fetal subtype has a better prognosis compared with small cell undifferentiated ones.
- Pretreatment extent of disease (PRETEXT) which was developed to stage the tumor before surgical removal and compare the efficacy of varous adjuvant chemotherapeutic agents. It is based on anatomy of liver and depending on tumor free sectors of liver.[15]
- Complications of hepatoblastoma includes:
- Pancytopenia
- Anemia
- Intraperitoneal tumor rupture
- Complications related to chemotherapy such as renal failure
- Post-transplant complications such as hepatic ductal obstruction, biliary leakage, thrombosis.[16]
- Psychosocial effects of treatment and painful procedures
Diagnosis
Diagnostic Study of Choice
- The diagnosis of hepatoblastoma is made when abdominal mass is detected on ultrasound or spiral CT scan, but a definitive diagnosis requires the histological evaluation of biopsy specimen after surgery.[10]
History and Symptoms
- The majority of patients with hepatoblastoma have an abdominal mass or abdominal distension. [10]
- Other symptoms of hepatoblastoma include:
- Abdominal discomfort
- Generalized fatigue
- Loss of appetite (Anorexia)
- Nausea and vomiting
- Ruptured tumor can cause symptoms of peritoneal irritation due to intraperitoneal bleeding such as severe abdominal pain, nausea, vomiting, and severe anemia.[17]
Physical Examination
- Physical examination of patients with hepatoblastoma is usually remarkable for single, mildly painful, rapidly enlarging abdominal mass that is found in the right lobe of the liver.[18][10]
- Most tumors are solitary; but can be multifocal as well.
Laboratory Findings
- Laboratory findings that help with the diagnosis of hepatoblastoma includes:[19]
- High levels of Alpha-fetoprotein (AFP)
- Mild liver function disturbances
- Anemia on complete blood count
- Thrombocytosis (more frequent because of the effect of thrombopoietin)[20]
- Thrombocytopenia (less common)
Electrocardiogram
- There are no ECG findings associated with hepatoblastoma.
X-ray
- Chest x-rays can be useful especially since this tumor has the affinity to metastasize to lungs.[21]
Ultrasound
- Imaging studies play an important role in the diagnosis, staging, and treatment of disease, most tumors can be resected surgically and ultrasound is often used in order to detect tumor size, also the initial diagnosis is made by abdominal ultrasound.
CT scan
- CT scan is very helpful to diagnose the disease, children with hepatoblastoma undergo either a CT or MRI scan at diagnosis. [22]
- Surgeons prefer an angiographic or biphasic CT scan because of better depiction of the hepatic arterial, portal venous and hepatic vein and other liver structures.
- Concerns about radiation exposures in pediatrics has changed this modality in favor of MRI, although MRI is much lengthy exam than CT has the advantage of multiplanar soft-tissue characterization, and when diffusion-weighted imaging techniques are used, MRI is exquisitely sensitive for detecting tiny liver lesions.
- Spiral CT scan findings of hypervascular lesions in the liver with delayed contrast excretion are highly suggestive of a malignant liver tumor.
MRI
- MRI has the advantage of multiplanar soft-tissue characterization, lack of harmful ionizing radiation and when diffusion-weighted imaging techniques are used, MRI is exquisitely sensitive for detecting tiny liver lesions.[13]
Other Imaging Findings
- Other imaging studies such as PET scan or even bone scan when there is evidence of metastasis to bone may be helpful in the diagnosis of hepatoblastoma. PET scan can be helpful in localizing recurrent hepatoblastoma.[23][24]
Other Diagnostic Studies
- Other diagnostic studies for hepatoblastoma include evaluation of serum level of alpha-fetoprotein, serum hCG level in rare cases of precocious puberty.[25][26]
Treatment
Medical Therapy
- The mainstay of therapy for hepatoblastoma is surgery, however, the vast majority of the tumors cannot be completely resected because of their large size or metastasis.[27]
- Liver transplantation can be considered for tumors that cannot be removed by surgery.[28]
- Chemotherapy is an important adjuvant therapy, and cisplatin is the most commonly used chemotherapeutic agent, it can reduce the volume of tumors that are too big for surgical removal.[29]
Surgery
- Surgery is the mainstay of treatment for hepatoblastoma.[30]
- The feasibility of surgery depends on the resectability of tumor at diagnosis.
Primary Prevention
- There are no established measures for the primary prevention of hepatoblastoma.
Secondary Prevention
- There are no established measures for the secondary prevention of hepatoblastoma.
References
- ↑ Aronson DC, Czauderna P, Maibach R, Perilongo G, Morland B (October 2014). "The treatment of hepatoblastoma: Its evolution and the current status as per the SIOPEL trials". J Indian Assoc Pediatr Surg. 19 (4): 201–7. doi:10.4103/0971-9261.142001. PMC 4204244. PMID 25336801.
- ↑ Rowland JM (November 2002). "Hepatoblastoma: assessment of criteria for histologic classification". Med. Pediatr. Oncol. 39 (5): 478–83. doi:10.1002/mpo.10171. PMID 12228903.
- ↑ Czauderna P, Lopez-Terrada D, Hiyama E, Häberle B, Malogolowkin MH, Meyers RL (February 2014). "Hepatoblastoma state of the art: pathology, genetics, risk stratification, and chemotherapy". Curr. Opin. Pediatr. 26 (1): 19–28. doi:10.1097/MOP.0000000000000046. PMID 24322718.
- ↑ MacDonald BT, Tamai K, He X (July 2009). "Wnt/beta-catenin signaling: components, mechanisms, and diseases". Dev. Cell. 17 (1): 9–26. doi:10.1016/j.devcel.2009.06.016. PMC 2861485. PMID 19619488.
- ↑ 5.0 5.1 Kiruthiga KG, Ramakrishna B, Saha S, Sen S (April 2018). "Histological and immunohistochemical study of hepatoblastoma: correlation with tumour behaviour and survival". J Gastrointest Oncol. 9 (2): 326–337. doi:10.21037/jgo.2018.01.08. PMC 5934143. PMID 29755772.
- ↑ 6.0 6.1 Heck JE, Meyers TJ, Lombardi C, Park AS, Cockburn M, Reynolds P, Ritz B (August 2013). "Case-control study of birth characteristics and the risk of hepatoblastoma". Cancer Epidemiol. 37 (4): 390–5. doi:10.1016/j.canep.2013.03.004. PMC 3679264. PMID 23558166.
- ↑ Finegold MJ, Lopez-Terrada DH, Bowen J, Washington MK, Qualman SJ (April 2007). "Protocol for the examination of specimens from pediatric patients with hepatoblastoma". Arch. Pathol. Lab. Med. 131 (4): 520–9. doi:10.1043/1543-2165(2007)131[520:PFTEOS]2.0.CO;2. PMID 17425379.
- ↑ Mussa A, Duffy KA, Carli D, Ferrero GB, Kalish JM (January 2019). "Defining an optimal time window to screen for hepatoblastoma in children with Beckwith-Wiedemann syndrome". Pediatr Blood Cancer. 66 (1): e27492. doi:10.1002/pbc.27492. PMID 30270492.
- ↑ Curia MC, Zuckermann M, De Lellis L, Catalano T, Lattanzio R, Aceto G, Veschi S, Cama A, Otte JB, Piantelli M, Mariani-Costantini R, Cetta F, Battista P (January 2008). "Sporadic childhood hepatoblastomas show activation of beta-catenin, mismatch repair defects and p53 mutations". Mod. Pathol. 21 (1): 7–14. doi:10.1038/modpathol.3800977. PMID 17962810.
- ↑ 10.0 10.1 10.2 10.3 10.4 Hiyama E (October 2014). "Pediatric hepatoblastoma: diagnosis and treatment". Transl Pediatr. 3 (4): 293–9. doi:10.3978/j.issn.2224-4336.2014.09.01. PMC 4728840. PMID 26835349.
- ↑ Darbari A, Sabin KM, Shapiro CN, Schwarz KB (September 2003). "Epidemiology of primary hepatic malignancies in U.S. children". Hepatology. 38 (3): 560–6. doi:10.1053/jhep.2003.50375. PMID 12939582.
- ↑ Allan BJ, Parikh PP, Diaz S, Perez EA, Neville HL, Sola JE (October 2013). "Predictors of survival and incidence of hepatoblastoma in the paediatric population". HPB (Oxford). 15 (10): 741–6. doi:10.1111/hpb.12112. PMC 3791112. PMID 23600968.
- ↑ 13.0 13.1 Shelmerdine SC, Roebuck DJ, Towbin AJ, McHugh K (August 2016). "MRI of paediatric liver tumours: How we review and report". Cancer Imaging. 16 (1): 21. doi:10.1186/s40644-016-0083-3. PMC 4986178. PMID 27526937.
- ↑ Musick SR, Babiker HM. PMID 30521216. Missing or empty
|title=(help) - ↑ Aronson DC, Schnater JM, Staalman CR, Weverling GJ, Plaschkes J, Perilongo G, Brown J, Phillips A, Otte JB, Czauderna P, MacKinlay G, Vos A (February 2005). "Predictive value of the pretreatment extent of disease system in hepatoblastoma: results from the International Society of Pediatric Oncology Liver Tumor Study Group SIOPEL-1 study". J. Clin. Oncol. 23 (6): 1245–52. doi:10.1200/JCO.2005.07.145. PMID 15718322.
- ↑ Becker K, Furch C, Schmid I, von Schweinitz D, Häberle B (January 2015). "Impact of postoperative complications on overall survival of patients with hepatoblastoma". Pediatr Blood Cancer. 62 (1): 24–8. doi:10.1002/pbc.25240. PMID 25251521.
- ↑ Ke HY, Chen JH, Jen YM, Yu JC, Hsieh CB, Chen CJ, Liu YC, Chen TW, Chan DC (October 2005). "Ruptured hepatoblastoma with massive internal bleeding in an adult". World J. Gastroenterol. 11 (39): 6235–7. PMC 4436650. PMID 16273660.
- ↑ Zhang Q, Ming J, Zhang S, Guo D, Qiu X (2013). "A rare case of adult hepatoblastoma with neuroendocrine differentiation misdiagnosed as neuroendocrine tumor". Int J Clin Exp Pathol. 6 (2): 308–13. PMC 3544231. PMID 23330017.
- ↑ Exelby PR, Filler RM, Grosfeld JL (June 1975). "Liver tumors in children in the particular reference to hepatoblastoma and hepatocellular carcinoma: American Academy of Pediatrics Surgical Section Survey--1974". J. Pediatr. Surg. 10 (3): 329–37. PMID 49416.
- ↑ Nickerson HJ, Silberman TL, McDonald TP (January 1980). "Hepatoblastoma, thrombocytosis, and increased thrombopoietin". Cancer. 45 (2): 315–7. PMID 6153151.
- ↑ Perilongo G, Brown J, Shafford E, Brock P, De Camargo B, Keeling JW, Vos A, Philips A, Pritchard J, Plaschkes J (October 2000). "Hepatoblastoma presenting with lung metastases: treatment results of the first cooperative, prospective study of the International Society of Paediatric Oncology on childhood liver tumors". Cancer. 89 (8): 1845–53. PMID 11042582.
- ↑ Aronson DC, Meyers RL (October 2016). "Malignant tumors of the liver in children". Semin. Pediatr. Surg. 25 (5): 265–275. doi:10.1053/j.sempedsurg.2016.09.002. PMID 27955729.
- ↑ Figarola MS, McQuiston SA, Wilson F, Powell R (December 2005). "Recurrent hepatoblastoma with localization by PET-CT". Pediatr Radiol. 35 (12): 1254–8. doi:10.1007/s00247-005-1568-6. PMID 16170514.
- ↑ Archer D, Babyn P, Gilday D, Greenberg MA (December 1993). "Potentially misleading bone scan findings in patients with hepatoblastoma". Clin Nucl Med. 18 (12): 1026–31. PMID 8293620.
- ↑ Nakagawara A, Ikeda K, Tsuneyoshi M, Daimaru Y, Enjoji M, Watanabe I, Iwafuchi M, Sawada T (October 1985). "Hepatoblastoma producing both alpha-fetoprotein and human chorionic gonadotropin. Clinicopathologic analysis of four cases and a review of the literature". Cancer. 56 (7): 1636–42. PMID 2411379.
- ↑ Morinaga S, Yamaguchi M, Watanabe I, Kasai M, Ojima M, Sasano N (May 1983). "An immunohistochemical study of hepatoblastoma producing human chorionic gonadotropin". Cancer. 51 (9): 1647–52. PMID 6187430.
- ↑ Pham TA, Gallo AM, Concepcion W, Esquivel CO, Bonham CA (December 2015). "Effect of Liver Transplant on Long-term Disease-Free Survival in Children With Hepatoblastoma and Hepatocellular Cancer". JAMA Surg. 150 (12): 1150–8. doi:10.1001/jamasurg.2015.1847. PMID 26308249.
- ↑ Reyes JD, Carr B, Dvorchik I, Kocoshis S, Jaffe R, Gerber D, Mazariegos GV, Bueno J, Selby R (June 2000). "Liver transplantation and chemotherapy for hepatoblastoma and hepatocellular cancer in childhood and adolescence". J. Pediatr. 136 (6): 795–804. PMID 10839879.
- ↑ Häberle B, Bode U, von Schweinitz D (2003). "[Differentiated treatment protocols for high- and standard-risk hepatoblastoma--an interim report of the German Liver Tumor Study HB99]". Klin Padiatr (in German). 215 (3): 159–65. doi:10.1055/s-2003-39375. PMID 12778356.
- ↑ Uchida H, Sakamoto S, Sasaki K, Takeda M, Hirata Y, Fukuda A, Hishiki T, Irie R, Nakazawa A, Miyazaki O, Nosaka S, Kasahara M (December 2018). "Surgical treatment strategy for advanced hepatoblastoma: Resection versus transplantation". Pediatr Blood Cancer. 65 (12): e27383. doi:10.1002/pbc.27383. PMID 30084209.