Gastritis pathophysiology: Difference between revisions
No edit summary |
No edit summary |
||
| Line 46: | Line 46: | ||
*The main role of the [[mucosa]] in the [[immune]] response is that the [[IgA]] prevents [[bacterial]] [[adhesion]] and [[IgG]] causes [[opsonization]] and [[complement]] activation. | *The main role of the [[mucosa]] in the [[immune]] response is that the [[IgA]] prevents [[bacterial]] [[adhesion]] and [[IgG]] causes [[opsonization]] and [[complement]] activation. | ||
*Due to the acidic environment, the [[antibodies]] produced quickly lose their adhesive properties and [[catalase]] produced by ''[[H. pylori]]'' protects against polymorphs. | *Due to the acidic environment, the [[antibodies]] produced quickly lose their adhesive properties and [[catalase]] produced by ''[[H. pylori]]'' protects against polymorphs. | ||
*However, this immune response is insufficient to eradicate the organism leading to the development of immune response directed towards preventing the damaging effects of the ''[[H. pylori]]''. | *However, this [[immune response]] is insufficient to eradicate the organism leading to the development of immune response directed towards preventing the damaging effects of the ''[[H. pylori]]''. | ||
*Hence the persistent antigenic stimulation leads to the formation of [[lymphoid follicles]], which is the consistent feature of chronic ''[[H. pylori]]'' infection. | *Hence the persistent [[antigenic]] stimulation leads to the formation of [[lymphoid follicles]], which is the consistent feature of chronic ''[[H. pylori]]'' infection. | ||
*These [[lymphoid follicles]] in the [[gastric mucosa]] constitutes [[MALT|mucosa-associated lymphoid tissue (MALT)]] from which gastric [[marginal zone]] [[B-cell lymphoma|B-cell lymphoma (MALToma)]] arises. | *These [[lymphoid follicles]] in the [[gastric mucosa]] constitutes [[MALT|mucosa-associated lymphoid tissue (MALT)]] from which gastric [[marginal zone]] [[B-cell lymphoma|B-cell lymphoma (MALToma)]] arises. | ||
Also, these | Also, these polymorphs accumulate around the pit isthmus, which is a proliferative compartment, causing lethal damage to [[stem cells]] resulting in [[glandular]] [[atrophy]]. | ||
====Microscopic pathology==== | ====Microscopic pathology==== | ||
| Line 57: | Line 57: | ||
*[[Lymphocytes]] and [[plasma cell]] infiltration | *[[Lymphocytes]] and [[plasma cell]] infiltration | ||
*[[Lymphoid follicles]] (typical feature of chronic gastritis) | *[[Lymphoid follicles]] (typical feature of chronic gastritis) | ||
*Around one-fifth of cases with an inflamed cardia may undergo intestinal metaplasia. <ref name="pmid10566710">{{cite journal| author=Voutilainen M, Färkkilä M, Mecklin JP, Juhola M, Sipponen P| title=Chronic inflammation at the gastroesophageal junction (carditis) appears to be a specific finding related to Helicobacter pylori infection and gastroesophageal reflux disease. The Central Finland Endoscopy Study Group. | journal=Am J Gastroenterol | year= 1999 | volume= 94 | issue= 11 | pages= 3175-80 | pmid=10566710 | doi=10.1111/j.1572-0241.1999.01513.x | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=10566710 }} </ref> | *Around one-fifth of cases with an [[inflamed]] [[cardia]] may undergo [[intestinal]] [[metaplasia]]. <ref name="pmid10566710">{{cite journal| author=Voutilainen M, Färkkilä M, Mecklin JP, Juhola M, Sipponen P| title=Chronic inflammation at the gastroesophageal junction (carditis) appears to be a specific finding related to Helicobacter pylori infection and gastroesophageal reflux disease. The Central Finland Endoscopy Study Group. | journal=Am J Gastroenterol | year= 1999 | volume= 94 | issue= 11 | pages= 3175-80 | pmid=10566710 | doi=10.1111/j.1572-0241.1999.01513.x | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=10566710 }} </ref> | ||
<gallery widths="150px"> | <gallery widths="150px"> | ||
| Line 90: | Line 90: | ||
| style="background:#DCDCDC; + " | [[Atrophy]] | | style="background:#DCDCDC; + " | [[Atrophy]] | ||
| style="background:#F5F5F5; + " | | | style="background:#F5F5F5; + " | | ||
*Loss of specialized glands from either antrum or corpus | *Loss of specialized [[glands]] from either [[antrum]] or corpus | ||
| style="background:#F5F5F5; + " | | | style="background:#F5F5F5; + " | | ||
* Mild, moderate, or severe loss | * Mild, moderate, or severe loss | ||
| Line 104: | Line 104: | ||
| style="background:#DCDCDC; + " | Intestinal [[Metaplasia]] | | style="background:#DCDCDC; + " | Intestinal [[Metaplasia]] | ||
| style="background:#F5F5F5; + " | | | style="background:#F5F5F5; + " | | ||
*Intestinal [[metaplasia]] of the epithelium | *[[Intestinal]] [[metaplasia]] of the epithelium | ||
| style="background:#F5F5F5; + " | | | style="background:#F5F5F5; + " | | ||
* Mild: less than one-third of mucosa involved | * Mild: less than one-third of mucosa involved | ||
| Line 112: | Line 112: | ||
===Atrophic Gastritis=== | ===Atrophic Gastritis=== | ||
[[Atrophy]] of [[stomach]] is defined as loss of glandular tissue due to continuous mucosal injury. This leads to thinning of [[gastric mucosa]]. | [[Atrophy]] of [[stomach]] is defined as loss of [[glandular]] tissue due to continuous [[mucosal]] injury. This leads to thinning of [[gastric mucosa]]. | ||
*The [[prevalence]] and severity of [[atrophy]] of [[stomach]] increases with age among the patient's [[chronic]] [[gastritis]] due to longer duration of ''[[H. pylori]]'' infection. | *The [[prevalence]] and severity of [[atrophy]] of [[stomach]] increases with age among the patient's [[chronic]] [[gastritis]] due to longer duration of ''[[H. pylori]]'' infection. | ||
*Due to glandular [[atrophy]], the prevalence of ''[[H. pylori]]'' positivity decreases. The main reasons are as follows: | *Due to glandular [[atrophy]], the prevalence of ''[[H. pylori]]'' positivity decreases. The main reasons are as follows: | ||
:*Due to intestinal [[metaplasia]] that is usually present in atrophic | :*Due to [[intestinal]] [[metaplasia]] that is usually present in [[atrophic]] [[stomach]], the organisms are absent as they usually colonize only [[gastric]] [[epithelium]]. | ||
:*As ''[[H. pylori]]'' requires partially acidic environment to thrive, [[hypochlorhydria]] creats hostile environment to ''[[H. pylori]]'' to survive.<ref name="pmid1916500">{{cite journal| author=Neithercut WD, Milne A, Chittajallu RS, el Nujumi AM, McColl KE| title=Detection of Helicobacter pylori infection of the gastric mucosa by measurement of gastric aspirate ammonium and urea concentrations. | journal=Gut | year= 1991 | volume= 32 | issue= 9 | pages= 973-6 | pmid=1916500 | doi= | pmc=1379031 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=1916500 }} </ref> | :*As ''[[H. pylori]]'' requires partially acidic environment to thrive, [[hypochlorhydria]] creats hostile environment to ''[[H. pylori]]'' to survive.<ref name="pmid1916500">{{cite journal| author=Neithercut WD, Milne A, Chittajallu RS, el Nujumi AM, McColl KE| title=Detection of Helicobacter pylori infection of the gastric mucosa by measurement of gastric aspirate ammonium and urea concentrations. | journal=Gut | year= 1991 | volume= 32 | issue= 9 | pages= 973-6 | pmid=1916500 | doi= | pmc=1379031 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=1916500 }} </ref> | ||
:*The [[metaplasia|metaplastic epithelium]] secretes acidic [[glycoproteins]] which create the most hostile environment for ''[[H. pylori]]''. | :*The [[metaplasia|metaplastic epithelium]] secretes acidic [[glycoproteins]] which create the most hostile environment for ''[[H. pylori]]''. | ||
| Line 121: | Line 121: | ||
====Pathogenesis==== | ====Pathogenesis==== | ||
*The continuous mucosal injury due to long-standing ''[[H. pylori]] | *The continuous mucosal injury due to long-standing ''[[H. pylori]] i''nfection, leads to [[atrophy]] of stomach. | ||
*This continuous pathological process results in [[gastric erosion|erosion]] or [[ulcer|ulceration]] of the mucosa leading to the destruction of the glandular layer and followed by fibrous replacement. | *This continuous pathological process results in [[gastric erosion|erosion]] or [[ulcer|ulceration]] of the [[mucosa]] leading to the destruction of the [[glandular]] layer and followed by [[fibrous]] replacement. | ||
*The destruction of the glandular [[basement membrane]] and the sheath of supporting cells prevents orderly regeneration. This uneven regeneration follows a divergent differentiation pathway producing [[metaplasia|metaplastic glands]] (pseudo-pyloric appearance) which are composed of cells of the 'ulcer-associated cell lineage'(UACL).<ref name="pmid11358897">{{cite journal| author=Pera M, Heppell J, Poulsom R, Teixeira FV, Williams J| title=Ulcer associated cell lineage glands expressing trefoil peptide genes are induced by chronic ulceration in ileal pouch mucosa. | journal=Gut | year= 2001 | volume= 48 | issue= 6 | pages= 792-6 | pmid=11358897 | doi= | pmc=1728308 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11358897 }} </ref> | *The destruction of the [[glandular]] [[basement membrane]] and the sheath of supporting cells prevents orderly regeneration. This uneven regeneration follows a divergent differentiation pathway producing [[metaplasia|metaplastic glands]] (pseudo-[[pyloric]] appearance) which are composed of cells of the 'ulcer-associated cell lineage' (UACL).<ref name="pmid11358897">{{cite journal| author=Pera M, Heppell J, Poulsom R, Teixeira FV, Williams J| title=Ulcer associated cell lineage glands expressing trefoil peptide genes are induced by chronic ulceration in ileal pouch mucosa. | journal=Gut | year= 2001 | volume= 48 | issue= 6 | pages= 792-6 | pmid=11358897 | doi= | pmc=1728308 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11358897 }} </ref> | ||
====Microscopic pathology==== | ====Microscopic pathology==== | ||
*Reduced number of [[oxyntic cells]]. No intestinal [[metaplasia]] | *Reduced number of [[oxyntic cells]]. No intestinal [[metaplasia]] | ||
*The [[mucosa]] is infiltrated with [[neutrophils]] | *The [[mucosa]] is infiltrated with [[neutrophils]] | ||
*''[[H. pylori]]'' is not seen on [[H&E stain]]. [[Immunohistochemical | *''[[H. pylori]]'' is not seen on [[H&E stain]]. | ||
*[[Immunohistochemical]] stain of ''[[H. pylori]]'' detects the organisms. | |||
[[image:Atrophic_gastritis.jpg|thumb|200px|center|Atrophic Gastritis, By Radioxoma (Own work) [CC BY-SA 3.0 (https://creativecommons.org/licenses/by-sa/3.0)], via Wikimedia Commons<ref name="urlFile:Atrophic gastritis (low zoom).jpg - Wikimedia Commons">{{cite web |url=https://commons.wikimedia.org/wiki/File%3AAtrophic_gastritis_(low_zoom).jpg |title=File:Atrophic gastritis (low zoom).jpg - Wikimedia Commons |format= |work= |accessdate=}}</ref>]] | [[image:Atrophic_gastritis.jpg|thumb|200px|center|Atrophic Gastritis, By Radioxoma (Own work) [CC BY-SA 3.0 (https://creativecommons.org/licenses/by-sa/3.0)], via Wikimedia Commons<ref name="urlFile:Atrophic gastritis (low zoom).jpg - Wikimedia Commons">{{cite web |url=https://commons.wikimedia.org/wiki/File%3AAtrophic_gastritis_(low_zoom).jpg |title=File:Atrophic gastritis (low zoom).jpg - Wikimedia Commons |format= |work= |accessdate=}}</ref>]] | ||
| Line 134: | Line 135: | ||
==Gross pathology== | ==Gross pathology== | ||
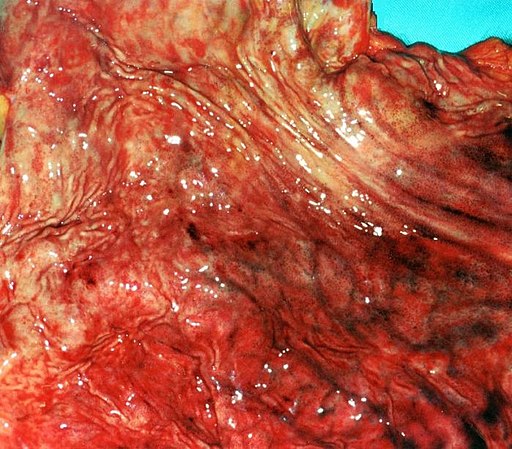
*'''Erosive Gastritis:''' | *'''Erosive Gastritis:''' | ||
**Erosive | **Erosive gastritis results due to the loss of [[superficial]] [[epithelium]] causing and it does not extend beyond the [[muscularis]] [[mucosa]]. | ||
**The crypts may present as dilated and contain acute inflammatory cells | **The crypts may present as [[dilated]] and contain acute [[inflammatory]] cells. | ||
[[image:Gastritis_erosiva.2278.jpg|thumb|300px|center|Erosive Gastritis, By Amadalvarez (Own work) [CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0)], via Wikimedia Commons<ref name="urlFile:Gastritis erosiva.2278.jpg - Wikimedia Commons">{{cite web |url=https://commons.wikimedia.org/wiki/File%3AGastritis_erosiva.2278.jpg |title=File:Gastritis erosiva.2278.jpg - Wikimedia Commons |format= |work= |accessdate=}}</ref>]] | [[image:Gastritis_erosiva.2278.jpg|thumb|300px|center|Erosive Gastritis, By Amadalvarez (Own work) [CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0)], via Wikimedia Commons<ref name="urlFile:Gastritis erosiva.2278.jpg - Wikimedia Commons">{{cite web |url=https://commons.wikimedia.org/wiki/File%3AGastritis_erosiva.2278.jpg |title=File:Gastritis erosiva.2278.jpg - Wikimedia Commons |format= |work= |accessdate=}}</ref>]] | ||
Revision as of 16:51, 28 December 2017
|
Gastritis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Gastritis pathophysiology On the Web |
|
American Roentgen Ray Society Images of Gastritis pathophysiology |
|
Risk calculators and risk factors for Gastritis pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Aravind Reddy Kothagadi M.B.B.S[2]
Overview
Gastritis depending on the causes may be classified into acute gastritis, chronic gastritis, atrophic gastritis, and H.pylori associated gastritis. In acute gastritis, the majority of patients, the initial acute phase of gastritis is subclinical and is of short duration (about 7 to 10 days). Acute gastritis also referred to as reactive gastritis occurs as a result of the trigger by factors such as NSAIDs, stress, bile reflux, radiation, alcohol abuse, cocaine addiction, and ischemic damage. In chronic gastritis, the H. pylori infection persists leading to accumulation of large number chronic inflammatory cells leading to active chronic gastritis.
Pathophysiology
Acute gastritis
- In the majority of patients, the initial acute phase of gastritis is subclinical and is of short duration (about 7 to 10 days).
- Acute gastritis also referred to as reactive gastritis occurs as a result of the trigger by factors such as NSAIDs, stress, bile reflux, radiation, alcohol abuse, cocaine addiction, and ischemic damage.
- In the majority of cases of H.pylori infection, the infection is not eliminated and there will be gradual accumulation of chronic inflammatory cells over the next 3 or 4 weeks.[1]
- In H. pylori infection, the organisms are spontaneously cleared in a small minority of people, especially in childhood.
Pathogenesis
- Following transmission, H. pylori penetrates the gastric mucosa and multiplies close to the surface epithelial cells.
- Following adhesion to epithelial cells, the bacteria releases lipopolysaccharides (endotoxin) and chemotactic mediators which penetrate the surface epithelial cells.[2][3]
- These bacterial factors attract the polymorphonuclear leukocytes to the site of infection and also caused mast cell degranulation, which releases acute inflammatory mediators. Mast cell degranulation leads to:
- Increased vascular permeability
- Increased polymorphonuclear leukocytes emigration
- Increased expression of leukocyte adhesion molecules
- The platelet activating factors (PAF) released from mast cells causes microthrombosis in mucosal capillaries resulting in hypoxic injury to the epithelium
- The macrophages release IL-1 and tumor necrosis factor alpha (TNF-α) which stimulates gastric epithelium to produce IL-8.
- The acute phase is associated with profound hypochlorhydria and a decreased ascorbic acid secretion into the gastric juice.[4]
- The acid output reaches pre-infection levels after several weeks but the ascorbic acid remains lower than normal for the duration of chronic gastritis, indicating that it is due to persisting inflammation rather than hypochlorhydria.[4]
Microscopic pathology
Histological features observed such as:
- Hyperemia
- Acute inflammation
- Increased polymorphonuclear neutrophil in the superficial lamina propria
- Erosion of the surface epithelium
- Sloughing
- Mucosal necrosis to a greater extent
- Scarring (later sequelae)
Chronic gastritis
In the majority of cases, the H. pylori infection persists leading to accumulation of large number chronic inflammatory cells leading to active chronic gastritis.
Pathogenesis
- The major diagnostic feature of chronic gastritis is an influx of lymphocytes and plasma cells (normally the antral mucosa is devoid of plasma cells and lymphocytes). Hence the presence of these cells is indicative of gastritis.[5]
- H. pylori colonizes more in the antrum than the corpus. Hence there is increased inflammatory cell infiltration in the antrum.
- The direct acting antigens of H. pylori like lipopolysaccharides, urease etc along with interleukins 1 and 6, activate T-helper cells which produce the variety of cytokines including IL4, IL5, and IL6.
- These interleukins differentiate into plasma cells releasing cytokines and anti-H.pylori infection like IgM-opsonizing and complement-fixing antibodies.
- The main role of the mucosa in the immune response is that the IgA prevents bacterial adhesion and IgG causes opsonization and complement activation.
- Due to the acidic environment, the antibodies produced quickly lose their adhesive properties and catalase produced by H. pylori protects against polymorphs.
- However, this immune response is insufficient to eradicate the organism leading to the development of immune response directed towards preventing the damaging effects of the H. pylori.
- Hence the persistent antigenic stimulation leads to the formation of lymphoid follicles, which is the consistent feature of chronic H. pylori infection.
- These lymphoid follicles in the gastric mucosa constitutes mucosa-associated lymphoid tissue (MALT) from which gastric marginal zone B-cell lymphoma (MALToma) arises.
Also, these polymorphs accumulate around the pit isthmus, which is a proliferative compartment, causing lethal damage to stem cells resulting in glandular atrophy.
Microscopic pathology
- Variable epithelial degeneration
- Neutrophil infiltration in the epithelium and the lamina propria
- Variable H. pylori colonization
- Lymphocytes and plasma cell infiltration
- Lymphoid follicles (typical feature of chronic gastritis)
- Around one-fifth of cases with an inflamed cardia may undergo intestinal metaplasia. [6]
-
Chronic gastritis - Intermedicate Magnification, By Nephron (Own work) [CC BY-SA 3.0 (https://creativecommons.org/licenses/by-sa/3.0) or GFDL (http://www.gnu.org/copyleft/fdl.html)], via Wikimedia Commons [7]
-
Chronic gastritis - Very-High Magnification, By Nephron (Own work) [CC BY-SA 3.0 (https://creativecommons.org/licenses/by-sa/3.0) or GFDL (http://www.gnu.org/copyleft/fdl.html)], via Wikimedia Commons [8]
Sydney system for grading of chronic gastritis[9]
| Sydney system for grading of Chronic Gastritis | ||
|---|---|---|
| Feature | Definition | Grading guidelines |
| Chronic inflammation |
|
|
| Activity |
|
|
| Atrophy |
| |
| Helicobacter pylori |
|
|
| Intestinal Metaplasia |
|
|
Atrophic Gastritis
Atrophy of stomach is defined as loss of glandular tissue due to continuous mucosal injury. This leads to thinning of gastric mucosa.
- The prevalence and severity of atrophy of stomach increases with age among the patient's chronic gastritis due to longer duration of H. pylori infection.
- Due to glandular atrophy, the prevalence of H. pylori positivity decreases. The main reasons are as follows:
- Due to intestinal metaplasia that is usually present in atrophic stomach, the organisms are absent as they usually colonize only gastric epithelium.
- As H. pylori requires partially acidic environment to thrive, hypochlorhydria creats hostile environment to H. pylori to survive.[10]
- The metaplastic epithelium secretes acidic glycoproteins which create the most hostile environment for H. pylori.
- Hence, based on above reasons, failure to demonstrate H. pylori does not deny the role of the organism in atrophic gastritis.
Pathogenesis
- The continuous mucosal injury due to long-standing H. pylori infection, leads to atrophy of stomach.
- This continuous pathological process results in erosion or ulceration of the mucosa leading to the destruction of the glandular layer and followed by fibrous replacement.
- The destruction of the glandular basement membrane and the sheath of supporting cells prevents orderly regeneration. This uneven regeneration follows a divergent differentiation pathway producing metaplastic glands (pseudo-pyloric appearance) which are composed of cells of the 'ulcer-associated cell lineage' (UACL).[11]
Microscopic pathology
- Reduced number of oxyntic cells. No intestinal metaplasia
- The mucosa is infiltrated with neutrophils
- H. pylori is not seen on H&E stain.
- Immunohistochemical stain of H. pylori detects the organisms.

Gross pathology
- Erosive Gastritis:
- Erosive gastritis results due to the loss of superficial epithelium causing and it does not extend beyond the muscularis mucosa.
- The crypts may present as dilated and contain acute inflammatory cells.
Videos
Chronic gastritis {{#ev:youtube|Wvn5TiiIB4Q}}
Atrophic gastritis
{{#ev:youtube|760GB43AZqE}}
References
- ↑ Sobala GM, Crabtree JE, Dixon MF, Schorah CJ, Taylor JD, Rathbone BJ; et al. (1991). "Acute Helicobacter pylori infection: clinical features, local and systemic immune response, gastric mucosal histology, and gastric juice ascorbic acid concentrations". Gut. 32 (11): 1415–8. PMC 1379180. PMID 1752479.
- ↑ Slomiany BL, Piotrowski J, Slomiany A (1998). "Induction of caspase-3 and nitric oxide synthase-2 during gastric mucosal inflammatory reaction to Helicobacter pylori lipopolysaccharide". Biochem Mol Biol Int. 46 (5): 1063–70. PMID 9861460.
- ↑ Crabtree JE (1996). "Gastric mucosal inflammatory responses to Helicobacter pylori". Aliment Pharmacol Ther. 10 Suppl 1: 29–37. PMID 8730257.
- ↑ 4.0 4.1 Sobala GM, Schorah CJ, Shires S, Lynch DA, Gallacher B, Dixon MF; et al. (1993). "Effect of eradication of Helicobacter pylori on gastric juice ascorbic acid concentrations". Gut. 34 (8): 1038–41. PMC 1374349. PMID 8174949.
- ↑ Genta RM, Hamner HW, Graham DY (1993). "Gastric lymphoid follicles in Helicobacter pylori infection: frequency, distribution, and response to triple therapy". Hum Pathol. 24 (6): 577–83. PMID 8505036.
- ↑ Voutilainen M, Färkkilä M, Mecklin JP, Juhola M, Sipponen P (1999). "Chronic inflammation at the gastroesophageal junction (carditis) appears to be a specific finding related to Helicobacter pylori infection and gastroesophageal reflux disease. The Central Finland Endoscopy Study Group". Am J Gastroenterol. 94 (11): 3175–80. doi:10.1111/j.1572-0241.1999.01513.x. PMID 10566710.
- ↑ "File:Chronic gastritis -- intermed mag.jpg - Wikimedia Commons".
- ↑ "File:Chronic gastritis -- very high mag.jpg - Wikimedia Commons".
- ↑ Dixon MF, Genta RM, Yardley JH, Correa P (1996). "Classification and grading of gastritis. The updated Sydney System. International Workshop on the Histopathology of Gastritis, Houston 1994". Am J Surg Pathol. 20 (10): 1161–81. PMID 8827022.
- ↑ Neithercut WD, Milne A, Chittajallu RS, el Nujumi AM, McColl KE (1991). "Detection of Helicobacter pylori infection of the gastric mucosa by measurement of gastric aspirate ammonium and urea concentrations". Gut. 32 (9): 973–6. PMC 1379031. PMID 1916500.
- ↑ Pera M, Heppell J, Poulsom R, Teixeira FV, Williams J (2001). "Ulcer associated cell lineage glands expressing trefoil peptide genes are induced by chronic ulceration in ileal pouch mucosa". Gut. 48 (6): 792–6. PMC 1728308. PMID 11358897.
- ↑ "File:Atrophic gastritis (low zoom).jpg - Wikimedia Commons".
- ↑ "File:Gastritis erosiva.2278.jpg - Wikimedia Commons".
![Chronic gastritis - Intermedicate Magnification, By Nephron (Own work) [CC BY-SA 3.0 (https://creativecommons.org/licenses/by-sa/3.0) or GFDL (http://www.gnu.org/copyleft/fdl.html)], via Wikimedia Commons [7]](/images/c/cb/Chronic_gastritis_--_intermed_mag.jpg)
![Chronic gastritis - Very-High Magnification, By Nephron (Own work) [CC BY-SA 3.0 (https://creativecommons.org/licenses/by-sa/3.0) or GFDL (http://www.gnu.org/copyleft/fdl.html)], via Wikimedia Commons [8]](/images/7/71/Chronic_gastritis_--_very_high_mag.jpg)