Fungal meningitis pathophysiology
|
Fungal meningitis Microchapters |
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Fungal meningitis pathophysiology On the Web |
|
American Roentgen Ray Society Images of Fungal meningitis pathophysiology |
|
Risk calculators and risk factors for Fungal meningitis pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Rim Halaby; Prince Tano Djan, BSc, MBChB [2]
Overview
The pathophysiology of fungal meningitis is not very well studied however, it is known to have a lot of similarities with bacterial meningitis. Fungal meningitis usually occurs in immunocompromised patients. The initial step in fungal meningitis is the pulmonary exposure to the fungi by the inhalation of airborne fungal spores. The pulmonary infection is usually self limited and maybe asymptomatic. Fungal infections are not contagious so they do not spread from one person to another.With an associated impaired immune response the fungus may disseminate. For instance in cryptococcal infection, the fungus may remain dormant in the lungs until the immune system weakens and then can reactivate and disseminate to the CNS. Cryptococcus has predilection for CNS dessimination. Although this remains unclear, the presence of a receptor on glial cells for a ligand on the organism has been suggested to enhance its invasion.[1] Cryptococcal meningitis is most common due to the virulence factors of the organism that enhance invasion of the blood brain barrier. These factors include: polysaccharide capsule which makes the organism withstand phagocytosis and host immune system, melanin production, ability to thrive at mammalian body temperatures, urease production and phospholipase production.[2][3][4][5][6][7][8][9][10] Once the fungi cross the blood brain barrier they cause an inflammation of the meninges and arachnoid space. The inflammation promotes cytokine release mainly tumor necrosis factor (TNF), interleukin 1, interleukin 2 , interleukin 6, interleukin 12, colony-stimulating factors, and interferon-λ.[11][12][13] The cytokines lead to modulation of host system resuting in fever, increase in the permeability of the blood brain barrier and subsequent cerebral edema and increase in the intracranial pressure. The increase in the permeability of the blood brain barrier is the cause of the observed elevation of the protein level in the cerebral spinal fluid.[14]
Pathophysiology
Pathogenesis
The Steps in Meningeal Fungal Infection
The steps involved in the pathogenesis of fungal meningitis is a complex process. Majority of cases result from an imbalance between the host immune response and virulence factors of pathogen causing infection. Outlined below are the steps explaining the underlying process in a comprehensive way.[15][16][17]
- The initial step in fungal meningitis is the pulmonary exposure to the fungi by the inhalation of airborne fungal spores.
- Inflammation results leading to a primary pulmonary and lymph node focus limiting the inhaled organism from further spread.[15]
- The pulmonary infection is usually self limited and maybe asymptomatic.
- With an associated impaired immune response the fungus may disseminate. For instance in cryptococcal infection, the fungus may remain dormant in the lungs until the immune system weakens and then can reactivate and disseminate to the CNS. Cryptococcus has predilection for CNS dessimination. Although this remains unclear, the presence of a receptor on glial cells for a ligand on the organism has been suggested to enhance its invasion.[1]
- Fungal infections are not contagious so they do not spread from one person to another.
- In most cases of fungal meningitis, the fungi undergo hematogenous spread.
- Patients with immunosuppression are the most vulnerable to fungal meningitis.
- Fungal meningitis may uncommonly occur In patients with no underlying immunosuppression. This usually is as a result of predisposing factors for instance some medical conditions such as pregnancy, certain lymphoreticular malignancies, iron chelation therapy, and diabetes impair host immune responses. These permit dissemination of even low-virulent pathogens.
- Cryptococcal meningitis is most common due to the virulence factors of the organism that enhancing invasion of the blood brain barrier. These factors include:[2][3][4][5][6][7][8][9][10]
- Polysaccharide capsule which makes the organism withstand phagocytosis and host immune system.
- Melanin production
- Ability to thrive at mammalian body temperatures
- Urease production
- Phospholipase production
- Once the fungi cross the blood brain barrier they cause an inflammation of the meninges and arachnoid space.
- The inflammation promotes cytokine release mainly tumor necrosis factor (TNF), interleukin 1, interleukin 2 , interleukin 6, interleukin 12, colony-stimulating factors, and interferon-λ.[11][12][13]
- The cytokines cause the fever observed in meningitis
- The cytokines promotes an increase in the permeability of the blood brain barrier and subsequent cerebral edema and increase in the intracranial pressure
- Cerebral edema leads to decreased blood flow to the brain and hypoxia
- The glucose level in the cerebral spinal fluid (CSF) will decrease due to a decreased transport of glucose coupled to an increased use of glucose by the fungi
- The increase in the permeability of the blood brain barrier is the cause of the observed elevation of the proteins level in the cerebral spinal fluid.[14]
The Underlying Mechanisms of the Symptoms
- Stimulation of the nociceptive fibers by inflammatory processes:
- Cerebral edema and obstructive of the cerebral spinal fluid's pathway:
- Increased intracranial pressure:
- Vascular damage:
- Cognitive and behavioral changes, seizures, stroke, myelopathy
- Seeding of inflammatory processes by the cerebral spinal fluid to the brainstem and cranial nerves (CN):
- Injury to spinal motor and sensory roots:
- Radiculopathy with associated radicular pain, sensory loss, motor weakness[18]
Genetics
Homozygous neutrophil dependent mutation of caspase recruitment domain 9 (CARD9) have been discovered to predispose to invasive chronic candida infections, especially of the central nervous system.[19]
Gross pathology
On gross pathology, there is cerebral edema.
Microscopic pathology
The image below is a microscopic pathology showing fungal component (multiple yellow arrow) in a section of brain tissue.
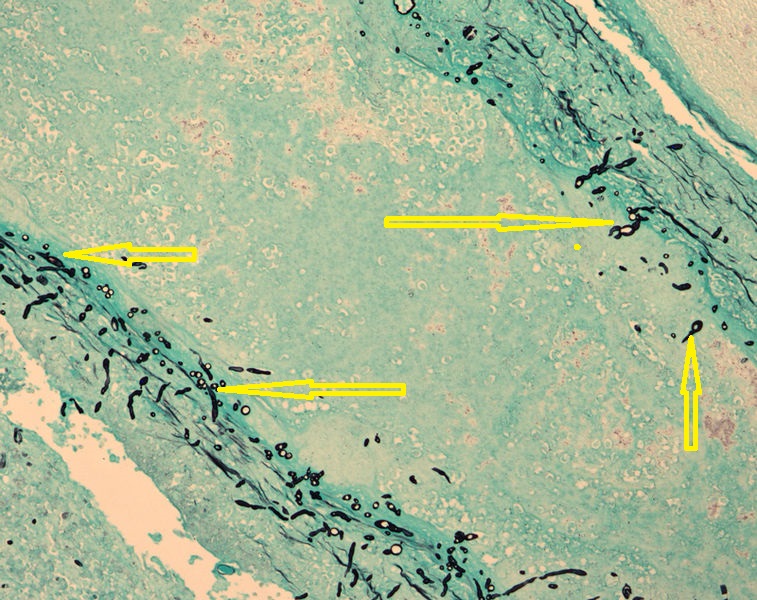
Cryptococcosis (PAS stain)
References
- ↑ 1.0 1.1 Merkel GJ, Scofield BA (1993). "Conditions affecting the adherence of Cryptococcus neoformans to rat glial and lung cells in vitro". J Med Vet Mycol. 31 (1): 55–64. PMID 8483058.
- ↑ 2.0 2.1 Granger DL, Perfect JR, Durack DT (1985). "Virulence of Cryptococcus neoformans. Regulation of capsule synthesis by carbon dioxide". J Clin Invest. 76 (2): 508–16. doi:10.1172/JCI112000. PMC 423853. PMID 3928681.
- ↑ 3.0 3.1 Jong A, Wu CH, Gonzales-Gomez I, Kwon-Chung KJ, Chang YC, Tseng HK; et al. (2012). "Hyaluronic acid receptor CD44 deficiency is associated with decreased Cryptococcus neoformans brain infection". J Biol Chem. 287 (19): 15298–306. doi:10.1074/jbc.M112.353375. PMC 3346080. PMID 22418440.
- ↑ 4.0 4.1 Kwon-Chung KJ, Rhodes JC (1986). "Encapsulation and melanin formation as indicators of virulence in Cryptococcus neoformans". Infect Immun. 51 (1): 218–23. PMC 261090. PMID 3079732.
- ↑ 5.0 5.1 Polacheck I, Platt Y, Aronovitch J (1990). "Catecholamines and virulence of Cryptococcus neoformans". Infect Immun. 58 (9): 2919–22. PMC 313587. PMID 2117574.
- ↑ 6.0 6.1 Jacobson ES, Emery HS (1991). "Catecholamine uptake, melanization, and oxygen toxicity in Cryptococcus neoformans". J Bacteriol. 173 (1): 401–3. PMC 207201. PMID 1898925.
- ↑ 7.0 7.1 Jacobson ES, Tinnell SB (1993). "Antioxidant function of fungal melanin". J Bacteriol. 175 (21): 7102–4. PMC 206840. PMID 8226653.
- ↑ 8.0 8.1 Chang YC, Kwon-Chung KJ (1994). "Complementation of a capsule-deficient mutation of Cryptococcus neoformans restores its virulence". Mol Cell Biol. 14 (7): 4912–9. PMC 358863. PMID 8007987.
- ↑ 9.0 9.1 Cox GM, Mukherjee J, Cole GT, Casadevall A, Perfect JR (2000). "Urease as a virulence factor in experimental cryptococcosis". Infect Immun. 68 (2): 443–8. PMC 97161. PMID 10639402.
- ↑ 10.0 10.1 Cox GM, McDade HC, Chen SC, Tucker SC, Gottfredsson M, Wright LC; et al. (2001). "Extracellular phospholipase activity is a virulence factor for Cryptococcus neoformans". Mol Microbiol. 39 (1): 166–75. PMID 11123698.
- ↑ 11.0 11.1 Levitz SM, Dupont MP (1993). "Phenotypic and functional characterization of human lymphocytes activated by interleukin-2 to directly inhibit growth of Cryptococcus neoformans in vitro". J Clin Invest. 91 (4): 1490–8. doi:10.1172/JCI116354. PMC 288124. PMID 7682573.
- ↑ 12.0 12.1 Brummer E, Stevens DA (1994). "Macrophage colony-stimulating factor induction of enhanced macrophage anticryptococcal activity: synergy with fluconazole for killing". J Infect Dis. 170 (1): 173–9. PMID 8014494.
- ↑ 13.0 13.1 Perfect JR, Granger DL, Durack DT (1987). "Effects of antifungal agents and gamma interferon on macrophage cytotoxicity for fungi and tumor cells". J Infect Dis. 156 (2): 316–23. PMID 3110308.
- ↑ 14.0 14.1 John Marx. Chapter 107. Central Nervous System Infections. Marx: Rosen's Emergency Medicine, 7th ed.. Mosby: Elsevier; 2009.
- ↑ 15.0 15.1 Baker RD (1976). "The primary pulmonary lymph node complex of crytptococcosis". Am J Clin Pathol. 65 (1): 83–92. PMID 1246992.
- ↑ Gottfredsson M, Perfect JR (2000). "Fungal meningitis". Semin Neurol. 20 (3): 307–22. doi:10.1055/s-2000-9394. PMID 11051295.
- ↑ Pettit AC, Kropski JA, Castilho JL, Schmitz JE, Rauch CA, Mobley BC; et al. (2012). "The index case for the fungal meningitis outbreak in the United States". N Engl J Med. 367 (22): 2119–25. doi:10.1056/NEJMoa1212292. PMID 23083311.
- ↑ Koroshetz WJ. Chapter 382. Chronic and Recurrent Meningitis. In: Longo DL, Fauci AS, Kasper DL, Hauser SL, Jameson JL, Loscalzo J, eds. Harrison's Principles of Internal Medicine. 18th ed. New York: McGraw-Hill; 2012.
- ↑ Herbst M, Gazendam R, Reimnitz D, Sawalle-Belohradsky J, Groll A, Schlegel PG; et al. (2015). "Chronic Candida albicans Meningitis in a 4-Year-Old Girl with a Homozygous Mutation in the CARD9 Gene (Q295X)". Pediatr Infect Dis J. 34 (9): 999–1002. doi:10.1097/INF.0000000000000736. PMID 25933095.