Epidural hematoma: Difference between revisions
No edit summary |
(→Trivia) |
||
| Line 67: | Line 67: | ||
The incidence of epidural hematoma following epidural anaesthesia is extremely difficult to quantify; estimates vary from 1 per 10,000 to 1 per 100,000 epidural anaesthetics. This means that a typical anaesthetist or [[anesthesiologist]] is statistically unlikely to cause one in a whole career. | The incidence of epidural hematoma following epidural anaesthesia is extremely difficult to quantify; estimates vary from 1 per 10,000 to 1 per 100,000 epidural anaesthetics. This means that a typical anaesthetist or [[anesthesiologist]] is statistically unlikely to cause one in a whole career. | ||
==See also== | ==See also== | ||
Revision as of 21:24, 25 January 2009
Template:DiseaseDisorder infobox
|
WikiDoc Resources for Epidural hematoma |
|
Articles |
|---|
|
Most recent articles on Epidural hematoma Most cited articles on Epidural hematoma |
|
Media |
|
Powerpoint slides on Epidural hematoma |
|
Evidence Based Medicine |
|
Cochrane Collaboration on Epidural hematoma |
|
Clinical Trials |
|
Ongoing Trials on Epidural hematoma at Clinical Trials.gov Trial results on Epidural hematoma Clinical Trials on Epidural hematoma at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Epidural hematoma NICE Guidance on Epidural hematoma
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Epidural hematoma Discussion groups on Epidural hematoma Patient Handouts on Epidural hematoma Directions to Hospitals Treating Epidural hematoma Risk calculators and risk factors for Epidural hematoma
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Epidural hematoma |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Please Take Over This Page and Apply to be Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [2] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Epidural or extradural hematoma is a buildup of blood occurring between the dura mater (the brain's tough outer membrane) and the skull. Often due to trauma, the condition is potentially deadly because the buildup of blood may increase pressure in the intracranial space and compress delicate brain tissue. 15 to 20% of patients with epidural hematomas die of the injury.[1]
Diagnosis
Causes
The cause of epidural hematoma is usually traumatic, although spontaneous hemorrhage is known to occur. Hemorrhages commonly result from acceleration-deceleration trauma and transverse forces.[2][3] Venous epidural bleeds are usually due to shearing injury from rotational or linear forces, caused when tissues of different densities slide over one another.
Epidural hematoma commonly results from a blow to the side of the head and is frequently caused by a fracture that passes through an arterial channel in the bone, most commonly a break in temporal bone interrupting middle meningeal artery, a branch of the external carotid.[4] Thus only 20 to 30% of epidural hematomas occur outside the region of the temporal bone.[5]
Features
Epidural bleeds, like subdural and subarachnoid hemorrhages, are extra-axial bleeds, occurring outside of the brain tissue, while intra-axial hemorrhages, including intraparenchymal and intraventricular hemorrhages, occur within it.[6]
Epidural bleeding is rapid because it is usually from arteries, which are high pressure. Epidural bleeds from arteries can grow until they reach their peak size at six to eight hours post injury, spilling from 25 to 75 cubic centimeters of blood into the intracranial space.[2] As the hematoma expands, it strips the dura from the inside of the skull, causing an intense headache.
Epidural bleeds can become large and raise intracranial pressure, causing the brain to shift, lose blood supply, or be crushed against the skull. Larger hematomas cause more damage. Epidural bleeds can quickly expand and compress the brain stem, causing unconsciousness, abnormal posturing, and abnormal pupil responses to light.[7]
10% of epidural bleeds may be venous.[4]
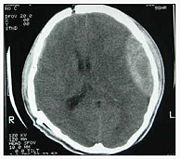
On images produced by CT scans and MRIs, epidural hematomas usually appear convex in shape because their expansion stops at skull's sutures, where the dura mater is tightly attached to the skull. Thus they expand inward toward the brain rather than along the inside of the skull, as occurs in subdural hematoma. The lens like shape of the hematoma leads the appearance of these bleeds to be called "lentiform".
Epidural hematomas may occur in combination with subdural hematomas, or either may occur alone.[4] CT scans reveal subdural or epidural hematomas in 20% of unconscious patients.[8]
In the hallmark of epidural hematoma, patients may regain consciousness during what is called a lucid interval, only to descend suddenly and rapidly into unconsciousness later. The lucid interval, which depends on the extent of the injury, is a key to diagnosing epidural hemorrhage. If the patient is not treated with prompt surgical intervention, death is likely to follow.[9]
-
Epidural Hematoma [10]
-
Epidural hematomas usually look convex on CT scans
-
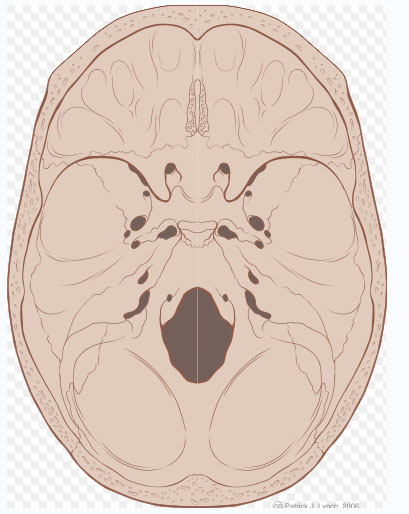
The interior of the skull has sharp ridges by which a moving brain can be injured.
Treatment
As with other types of intracranial hematomas, the blood may be aspirated surgically to remove the mass and reduce the pressure it puts on the brain.[3] The hematoma is neurosurgically evacuated through a burr hole or craniotomy. The diagnosis of epidural hematoma requires a patient to be cared for in a facility with a neurosurgeon on call to decompress the hematoma if necessary and stop the bleed by ligating the injured vessel branches.
Epidural hematoma in the spine
Bleeding into the epidural space in the spine may also cause epidural hematoma. These may arise spontaneously (e.g. during childbirth, or as a rare complication of anaesthesia (such as epidural anaesthesia) or surgery (such as laminectomy).
The anatomy of the epidural space means that spinal epidural hematoma has a different profile from cranial epidural hematoma. In the spine, the epidural space contains loose fatty tissue, and the epidural venous plexus, a network of large, thin-walled veins. This means that bleeding is likely to be venous. Anatomical abnormalities and bleeding disorders make these lesions more likely.
They may cause pressure on the spinal cord or cauda equina, which may present as pain, muscle weakness, or bladder and bowel dysfunction.
The diagnosis may be made on clinical appearance and time course of symptoms. It usually requires MRI scanning to confirm.
The treatment is surgical decompression.
The incidence of epidural hematoma following epidural anaesthesia is extremely difficult to quantify; estimates vary from 1 per 10,000 to 1 per 100,000 epidural anaesthetics. This means that a typical anaesthetist or anesthesiologist is statistically unlikely to cause one in a whole career.
See also
References
- ↑ Sanders MJ and McKenna K. 2001. Mosby’s Paramedic Textbook, 2nd revised Ed. Chapter 22, "Head and Facial Trauma." Mosby.
- ↑ 2.0 2.1 University of Vermont College of Medicine. "Neuropathology: Trauma to the CNS." Accessed through web archive. Retrieved on February 6, 2007.
- ↑ 3.0 3.1 McCaffrey P. 2001. "The Neuroscience on the Web Series: CMSD 336 Neuropathologies of Language and Cognition." California State University, Chico. Retrieved on February 6, 2007.
- ↑ 4.0 4.1 4.2 Shepherd S. 2004. "Head Trauma." Emedicine.com. Retrieved on February 6, 2007.
- ↑ Graham DI and Gennareli TA. Chapter 5, "Pathology of Brain Damage After Head Injury" Cooper P and Golfinos G. 2000. Head Injury, 4th Ed. Morgan Hill, New York.
- ↑ Wagner AL. 2006. "Subdural Hematoma." Emedicine.com. Retrieved on February 6, 2007.
- ↑ Singh J and Stock A. 2006. "Head Trauma." Emedicine.com. Retrieved on February 6, 2007.
- ↑ Downie A. 2001. "Tutorial: CT in Head Trauma". Retrieved on February 6, 2007.
- ↑ Caroline NL. 1991. Emergency Medical Treatment. Little Brown & Company.
- ↑ http://picasaweb.google.com/mcmumbi/USMLEIIImages
External links
Template:Cerebral hemorrhage
Template:Injuries, other than fractures, dislocations, sprains and strains
Template:SIB
![Epidural Hematoma [10]](/images/c/cd/Epidural_hematoma.jpg)