Coxsackie virus: Difference between revisions
Usama Talib (talk | contribs) No edit summary |
|||
| Line 75: | Line 75: | ||
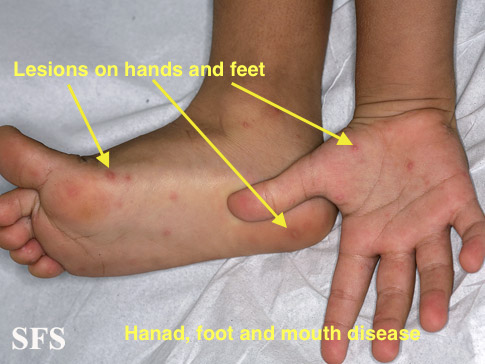
|[[Hand foot and mouth disease]] | |[[Hand foot and mouth disease]] | ||
| | | | ||
*Fever | *[[Fever]] | ||
*Headache | *[[Headache]] | ||
*Loss of appetite | *Loss of [[appetite]] | ||
*Maculopapular or vesicular rash with very small blisters on | *Maculopapular or [[vesicular rash]] with very small blisters on [[hand]]s, [[feet]], and diaper area; may be tender or painful if pressed | ||
*Sore throat* | *[[Sore throat]] | ||
Ulcers in the throat (including | *[[Ulcers]] in the [[throat]] (including [[tonsil]]s), [[mouth]], and [[tongue]] | ||
| | | | ||
*Throat and lesion swabs | *Throat and lesion swabs | ||
| Line 103: | Line 103: | ||
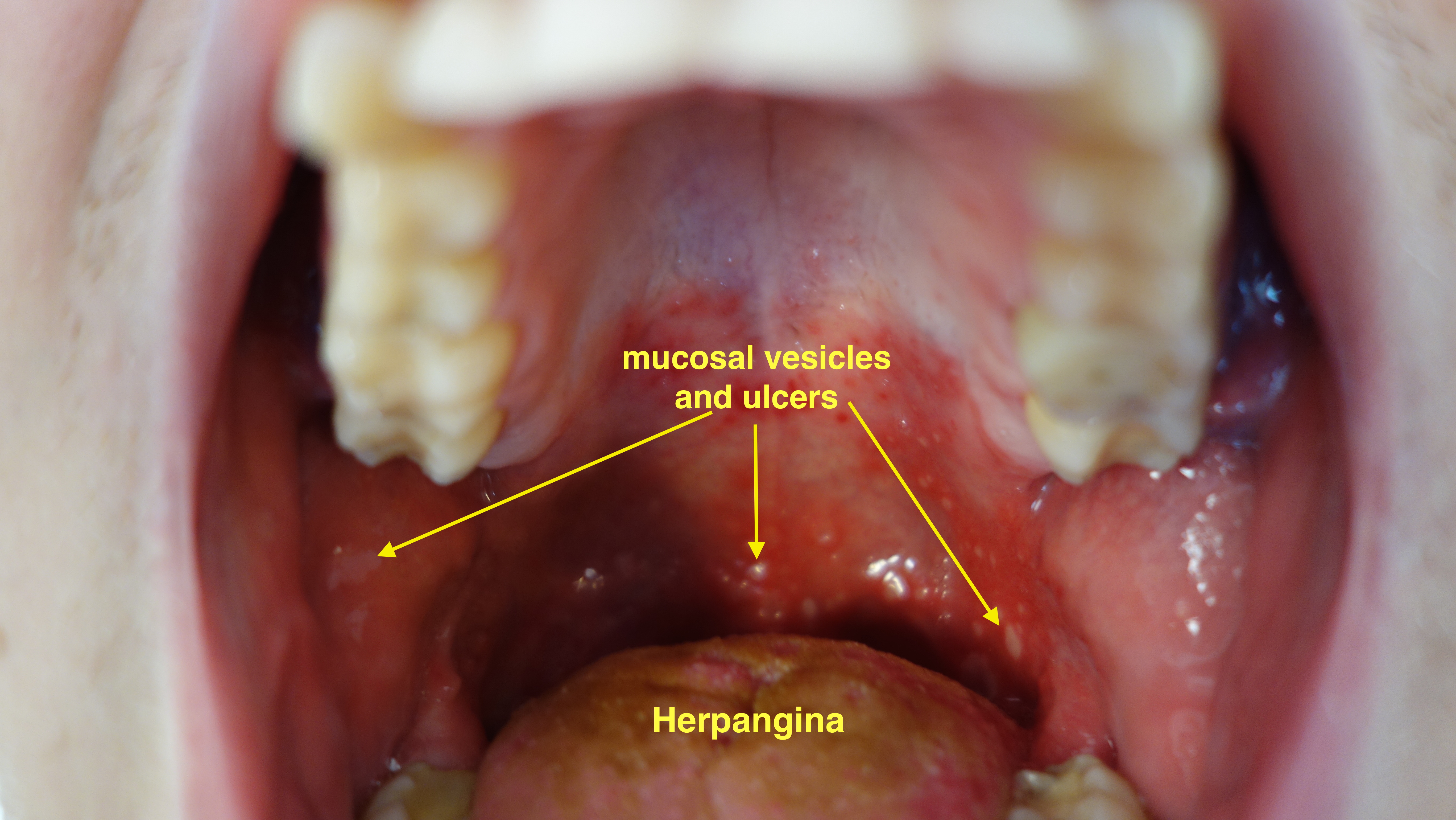
|[[Herpangina]] | |[[Herpangina]] | ||
| | | | ||
*Sudden fever | *Sudden [[fever]] | ||
*[[Sore throat]] and [[dysphagia]]- May occur up to 24 hours before the appearance of the | *[[Sore throat]] and [[dysphagia]]- May occur up to 24 hours before the appearance of the xanthem | ||
* | *[[Vomiting]] | ||
*Abdominal pain | *[[Abdominal pain]] | ||
*[[Myalgia]] | *[[Myalgia]] | ||
*Headache | *[[Headache]] | ||
*Pharyngeal lesions | *[[Pharyngeal]] lesions | ||
| | | | ||
*Primarily clinical | *Primarily clinical | ||
*Pharyngeal viral | *[[Pharyngeal]] viral [[culture]]s may be helpful | ||
* Approximately 1 week after infection, type-specific [[antibodies]] appear in the blood | * Approximately 1 week after infection, type-specific [[antibodies]] appear in the blood | ||
| [[File:Herpangina 2.jpg|Herpangina|400px]] | | [[File:Herpangina 2.jpg|Herpangina|400px]] | ||
| Line 121: | Line 121: | ||
*[[Nuchal rigidity]] | *[[Nuchal rigidity]] | ||
*[[Fever]] | *[[Fever]] | ||
*Altered mental status | *[[Altered mental status]] | ||
| | | | ||
*Clinical | *Clinical | ||
*[[Lumbar puncture]] CSF analysis | *[[Lumbar puncture]] [[CSF]] analysis | ||
*CT rarely | *[[CT]] rarely | ||
| | | | ||
|- | |- | ||
| Line 140: | Line 140: | ||
*Clinical | *Clinical | ||
*[[EKG]] | *[[EKG]] | ||
*Cardiac | *[[Cardiac biomarkers]] | ||
**[[Creatine kinase]]<ref name="spodick">{{cite journal | author= Spodick DH | title= Acute pericarditis: current concepts and practice | journal= JAMA | year=2003 | pages=1150–3 | volume=289 | issue=9 | pmid=12622586 | doi= 10.1001/jama.289.9.1150}}</ref><ref name="karja">{{cite journal | author= Karjalainen J, Heikkila J | title= "Acute pericarditis": myocardial enzyme release as evidence for myocarditis | journal= Am Heart J| year=1986| pages=546–52 | volume=111 | issue=3 | pmid=3953365 | doi= 10.1016/0002-8703(86)90062-1}}</ref> | **[[Creatine kinase]]<ref name="spodick">{{cite journal | author= Spodick DH | title= Acute pericarditis: current concepts and practice | journal= JAMA | year=2003 | pages=1150–3 | volume=289 | issue=9 | pmid=12622586 | doi= 10.1001/jama.289.9.1150}}</ref><ref name="karja">{{cite journal | author= Karjalainen J, Heikkila J | title= "Acute pericarditis": myocardial enzyme release as evidence for myocarditis | journal= Am Heart J| year=1986| pages=546–52 | volume=111 | issue=3 | pmid=3953365 | doi= 10.1016/0002-8703(86)90062-1}}</ref> | ||
**[[Cardiac troponin]]-I (cTnI)<ref name="bonnefoy">{{cite journal | author= Bonnefoy E, Godon P, Kirkorian G, Fatemi M, Chevalier P, Touboul P | title= Serum cardiac troponin I and ST-segment elevation in patients with acute pericarditis | journal= Eur Heart J| year=2000| pages=832–6 | volume=21 | issue=10 | pmid=10781355 | doi= 10.1053/euhj.1999.1907}}</ref><ref name="imazio">{{cite journal | author= Imazio M, Demichelis B, Cecchi E, Belli R, Ghisio A, Bobbio M, Trinchero R | title= Cardiac troponin I in acute pericarditis | journal= J Am Coll Cardiol| year=2003| pages=2144–8 | volume=42 | issue=12 | pmid=14680742 | doi= 10.1016/j.jacc.2003.02.001}}</ref> | **[[Cardiac troponin]]-I (cTnI)<ref name="bonnefoy">{{cite journal | author= Bonnefoy E, Godon P, Kirkorian G, Fatemi M, Chevalier P, Touboul P | title= Serum cardiac troponin I and ST-segment elevation in patients with acute pericarditis | journal= Eur Heart J| year=2000| pages=832–6 | volume=21 | issue=10 | pmid=10781355 | doi= 10.1053/euhj.1999.1907}}</ref><ref name="imazio">{{cite journal | author= Imazio M, Demichelis B, Cecchi E, Belli R, Ghisio A, Bobbio M, Trinchero R | title= Cardiac troponin I in acute pericarditis | journal= J Am Coll Cardiol| year=2003| pages=2144–8 | volume=42 | issue=12 | pmid=14680742 | doi= 10.1016/j.jacc.2003.02.001}}</ref> | ||
| Line 173: | Line 173: | ||
| | | | ||
*[[Chest pain]] | *[[Chest pain]] | ||
*Dyspnea | *[[Dyspnea]] | ||
*Nonspecific chest discomfort | *Nonspecific chest discomfort | ||
| | | | ||
| Line 187: | Line 187: | ||
*Attacks of severe pain in the lower chest, often on one side<ref name="pmid13042253">{{cite journal |author=WARIN JF, DAVIES JB, SANDERS FK, VIZOSO AD |title=Oxford epidemic of Bornholm disease, 1951 |journal=Br Med J |volume=1 |issue=4824 |pages=1345–51 |year=1953 |month=June |pmid=13042253 |pmc=2016648 |doi= |url=}}</ref> | *Attacks of severe pain in the lower chest, often on one side<ref name="pmid13042253">{{cite journal |author=WARIN JF, DAVIES JB, SANDERS FK, VIZOSO AD |title=Oxford epidemic of Bornholm disease, 1951 |journal=Br Med J |volume=1 |issue=4824 |pages=1345–51 |year=1953 |month=June |pmid=13042253 |pmc=2016648 |doi= |url=}}</ref> | ||
*[[Pleuritic pain]] with the slightest movement of the [[rib cage]] | *[[Pleuritic pain]] with the slightest movement of the [[rib cage]] | ||
*Dyspnea | *[[Dyspnea]] | ||
*Very few have classic muscle pain in the chest and upper abdomen | *Very few have classic muscle pain in the chest and upper abdomen | ||
*May be accompanied by a panic attack | *May be accompanied by a panic attack | ||
| | | | ||
*Clinical | *Clinical | ||
*CXR | *[[CXR]] | ||
| | | | ||
|- | |- | ||
| Line 202: | Line 202: | ||
* [[Fatigue]] | * [[Fatigue]] | ||
* [[Fever]], usually low-grade | * [[Fever]], usually low-grade | ||
* General itching | * General [[itching]] | ||
* [[Jaundice]] (yellowing of the skin or eyes) | * [[Jaundice]] (yellowing of the skin or eyes) | ||
* [[Loss of appetite]] | * [[Loss of appetite]] | ||
| Line 220: | Line 220: | ||
*[[Interstitial lung disease]] | *[[Interstitial lung disease]] | ||
*Gastrointestinal manifestations | *Gastrointestinal manifestations | ||
*CNS involvement | *[[CNS]] involvement | ||
| | | | ||
*Clinical | *Clinical | ||
*Autoantibodies | *[[Autoantibodies]] | ||
**Anti-Ro/SSA and anti-La/SSB antibodies | **Anti-Ro/SSA and anti-La/SSB antibodies | ||
**Anti-centromere antibodies | **[[Anti-centromere antibodies]] | ||
| [[File:Sjogren's syndrome-1.jpg|Sjogren's syndrome|400px]] | | [[File:Sjogren's syndrome-1.jpg|Sjogren's syndrome|400px]] | ||
|}</small> | |}</small> | ||
Revision as of 18:49, 5 April 2017
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]Associate Editor(s)-in-Chief: Usama Talib, BSc, MD [2]
|
Coxsackie Virus |
Overview
Coxsackie (virus) is a cytolytic virus of the picornaviridae family, an enterovirus (a group containing the polioviruses, coxsackieviruses, and echoviruses). There are 61 non-polio enteroviruses that can cause disease in humans, of which 23 are coxsackie A viruses (6 are Coxsackie B viruses). Enterovirus are the second most common viral infectious agents in humans (after the rhinoviruses)
Classification
Coxsackie viruses consist of coxsackie A virus and coxsackie B virus. Coxsackie B virus has 6 serotypes, one of the significant serotypes is called coxsackie B4 virus.
| Coxsackie Virus | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Coxsackie A virus | Coxsackie B virus[1] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Common Coxsackie B virus diseases | Coxsackie B4 virus diseases | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| • Hand, foot and mouth disease • Acute hemorrhagic conjunctivitis • Herpangina • Aseptic meningitis | • Pericarditis • Myocarditis • Pericardial effusion • Pleurodynia • Hepatitis • Sjogren's syndorme | • Diabetes mellitus • Acute flaccid myelitis[2] | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Differential Diagnosis
Coxsackie A virus and coxsackie B virus can cause multiple diseases in humans. The wide array of diseases caused by coxsackie viruses can be differentiated from one another easily on the basis of involvement of the organs systems, clinical presentation and diagnostic techniques.
| Virus Type | Disease | Clinical Features | Diagnosis | Image |
|---|---|---|---|---|
| Coxscakie A virus | Hand foot and mouth disease |
|
| |
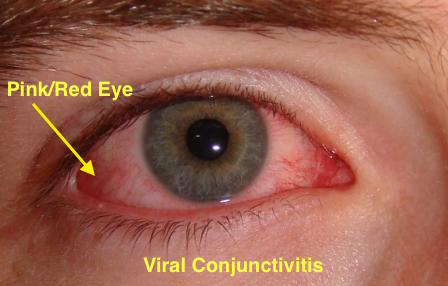
| Acute hemorrhagic conjunctivitis[3][4][5] |
|
|
| |
| Herpangina |
|
|
| |
| Aseptic Meningitis |
|
|||
| Coxsackie B virus | Pericarditis |
|
|
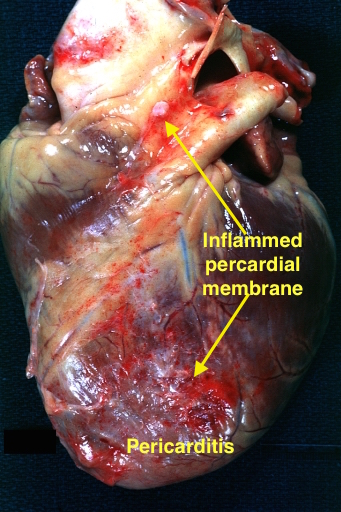
|
| Myocarditis[10][11] |
|
|
Viral myocarditis | |
| Pericardial effusion |
|
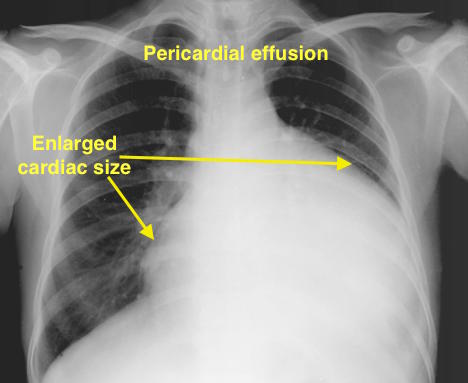
| ||
| Pleurodynia |
|
|||
| Hepatitis |
|
|||
| Sjogren's syndrome |
|
|

|
Template:Baltimore classification Template:Viral diseases
- ↑ Fields, Bernard N. (1985). Fields Virology. New York: Raven Press. pp. 739–794. ISBN 0-88167-026-X. Unknown parameter
|coauthors=ignored (help) - ↑ Cho SM, MacDonald S, Frontera JA (2017). "Coxsackie B3/B4-Related Acute Flaccid Myelitis". Neurocrit Care. doi:10.1007/s12028-017-0377-8. PMID 28324262.
- ↑ Yin-Murphy M (1976). "Simple tests for the diagnosis of picornavirus epidemic conjunctivitis (acute hemorrhagic conjunctivitis)". Bull World Health Organ. 54 (6): 675–9. PMC 2366581. PMID 1088513.
- ↑ Pinto RD, Lira RP, Arieta CE, Castro RS, Bonon SH (2015). "The prevalence of adenoviral conjunctivitis at the Clinical Hospital of the State University of Campinas, Brazil". Clinics (Sao Paulo). 70 (11): 748–50. doi:10.6061/clinics/2015(11)06. PMC 4642493. PMID 26602522.
- ↑ Jhanji V, Chan TC, Li EY, Agarwal K, Vajpayee RB (2015). "Adenoviral keratoconjunctivitis". Surv Ophthalmol. 60 (5): 435–43. doi:10.1016/j.survophthal.2015.04.001. PMID 26077630.
- ↑ Spodick DH (2003). "Acute pericarditis: current concepts and practice". JAMA. 289 (9): 1150–3. doi:10.1001/jama.289.9.1150. PMID 12622586.
- ↑ Karjalainen J, Heikkila J (1986). ""Acute pericarditis": myocardial enzyme release as evidence for myocarditis". Am Heart J. 111 (3): 546–52. doi:10.1016/0002-8703(86)90062-1. PMID 3953365.
- ↑ Bonnefoy E, Godon P, Kirkorian G, Fatemi M, Chevalier P, Touboul P (2000). "Serum cardiac troponin I and ST-segment elevation in patients with acute pericarditis". Eur Heart J. 21 (10): 832–6. doi:10.1053/euhj.1999.1907. PMID 10781355.
- ↑ Imazio M, Demichelis B, Cecchi E, Belli R, Ghisio A, Bobbio M, Trinchero R (2003). "Cardiac troponin I in acute pericarditis". J Am Coll Cardiol. 42 (12): 2144–8. doi:10.1016/j.jacc.2003.02.001. PMID 14680742.
- ↑ Feldman AM, McNamara D. Myocarditis. N Engl J Med 2000;343:1388-98. PMID 11070105.
- ↑ Sarda L, Colin P, Boccara F, Daou D, Lebtahi R, Faraggi M; et al. (2001). "Myocarditis in patients with clinical presentation of myocardial infarction and normal coronary angiograms". J Am Coll Cardiol. 37 (3): 786–92. PMID 11693753.
- ↑ 12.0 12.1 Smith SC, Ladenson JH, Mason JW, Jaffe AS (1997). "Elevations of cardiac troponin I associated with myocarditis. Experimental and clinical correlates". Circulation. 95 (1): 163–8. PMID 8994432.
- ↑ Lauer B, Niederau C, Kühl U, Schannwell M, Pauschinger M, Strauer BE; et al. (1997). "Cardiac troponin T in patients with clinically suspected myocarditis". J Am Coll Cardiol. 30 (5): 1354–9. PMID 9350939.
- ↑ Soongswang J, Durongpisitkul K, Ratanarapee S, Leowattana W, Nana A, Laohaprasitiporn D; et al. (2002). "Cardiac troponin T: its role in the diagnosis of clinically suspected acute myocarditis and chronic dilated cardiomyopathy in children". Pediatr Cardiol. 23 (5): 531–5. PMID 12211203.
- ↑ WARIN JF, DAVIES JB, SANDERS FK, VIZOSO AD (1953). "Oxford epidemic of Bornholm disease, 1951". Br Med J. 1 (4824): 1345–51. PMC 2016648. PMID 13042253. Unknown parameter
|month=ignored (help)