Cerebral arteriovenous malformation: Difference between revisions
No edit summary |
No edit summary |
||
| Line 14: | Line 14: | ||
}} | }} | ||
{{Search infobox}} | {{Search infobox}} | ||
{{CMG}} | {{CMG}} {{AE}}:{{KD}} | ||
'''''Synonyms and keywords:''''' AVM | '''''Synonyms and keywords:''''' AVM | ||
| Line 20: | Line 20: | ||
==Overview== | ==Overview== | ||
A '''cerebral arteriovenous malformation (AVM)''' is a [[congenital disorder]] of [[blood vessel]]s within the [[human brain|brain]], characterized by tangle(s) of [[vein]]s and [[artery|arteries]]. While an [[arteriovenous malformation]] can occur elsewhere in the body, this article discusses malformations found in the brain. | A '''cerebral arteriovenous malformation (AVM)''' is a [[congenital disorder]] of [[blood vessel]]s within the [[human brain|brain]], characterized by tangle(s) of [[vein]]s and [[artery|arteries]]. While an [[arteriovenous malformation]] can occur elsewhere in the body, this article discusses malformations found in the brain. | ||
==Pathophysiology== | ==Pathophysiology== | ||
AVMs are an abnormal connection between the arteries and veins in the human brain. In a normal brain [[oxygen]] enriched blood from the heart travels in sequence through smaller blood vessels going from arteries, to [[arterioles]] and then [[capillary|capillaries]].<ref name="Mayo-Causes"/> Oxygen is removed in the latter vessel to be used by the brain.<ref name="Mayo-Causes"/> After the oxygen is removed blood reaches [[venules]] and later veins which will take it back to the heart and lungs.<ref name="Mayo-Causes"/> On the other hand when there is an AVM blood goes directly from arteries to veins through the abnormal vessels disrupting the normal circulation of blood.<ref name="Mayo-Causes"/> | |||
==Causes== | |||
Arteriovenous malformations are most commonly of [[prenatal]] origin.<ref name="Mayo-Causes">{{Cite web|url=http://www.mayoclinic.com/health/brain-avm/DS01126/DSECTION=causes |title=Brain AVM (arteriovenous malformation)-Causes |author=Mayo Clinic staff |month=02 |year=2009|publisher=Mayo Foundation for Medical Education and Research |accessdate=2010-05-30}}</ref> The cause of AVMs remains unknown.<ref name="Mayo-Causes"/> | |||
==Epidemiology and Demographics== | |||
* The annual new detection rate [[incidence (epidemiology)|incidence]] of AVMs is approximately 1 per 100000 a year. The [[point prevalence]] in adults is approximately 18 per 100000.<ref name="pmid11571210">{{Cite journal|author=Al-Shahi R, Warlow C |title=A systematic review of the frequency and prognosis of arteriovenous malformations of the brain in adults |journal=Brain |volume=124 |issue=Pt 10 |pages=1900–26 |year=2001 |month=October |pmid=11571210 |doi= 10.1093/brain/124.10.1900|url=http://brain.oxfordjournals.org/cgi/content/full/124/10/1900?view=long&pmid=11571210 |accessdate=2010-05-18}}</ref> | |||
* AVMs are more common in males than females, although in females [[pregnancy]] may start or worsen symptoms due the increase in [[blood flow]] and [[blood volume|volume]] it usually brings.<ref name="Mayo-RF">{{Cite web|url=http://www.mayoclinic.com/health/brain-avm/DS01126/DSECTION=risk-factors |title=Brain AVM (arteriovenous malformation)-Risk factors |author=Mayo Clinic staff |month=02 |year=2009|publisher=Mayo Foundation for Medical Education and Research |accessdate=2010-05-30}}</ref> | |||
< | |||
< | |||
== | |||
The | |||
==Diagnosis== | ==Diagnosis== | ||
===History and Symptoms=== | |||
The most frequently observed problems related to an AVM are | |||
===MRI=== | * [[Headache]] | ||
* [[Seizure]] | |||
* Symptoms of [[intracranial hemorrhage]] may be present which include | |||
# [[loss of consciousness]] | |||
# [[nausea]] | |||
# [[vomiting]] | |||
# [[incontinence]] | |||
# [[blurred vision]] | |||
# [[hemiparesis]] | |||
# [[aphasia]] | |||
# a loss of touch sensation on one side of the body | |||
===Physical Examination=== | |||
===HEENT=== | |||
* [[Hydrocephalus]] may be present | |||
===Neurologic=== | |||
* [[Meningeal signs]] may be present | |||
* [[hemiparesis]] may be present | |||
* [[aphasia]] may be present | |||
* [[Hemianesthesia]] may be present | |||
===Laboratory findings=== | |||
===[[Lumbar puncture]]=== | |||
Lumbar puncture can be used to examine spinal fluid for red blood cells; this condition is indicative of leakage of blood from the bleeding vessels into the [[subarachnoid space]]. | |||
===[[CT]]=== | |||
[[CT]] head can reveal the site of the bleed. | |||
===[[MRI]]=== | |||
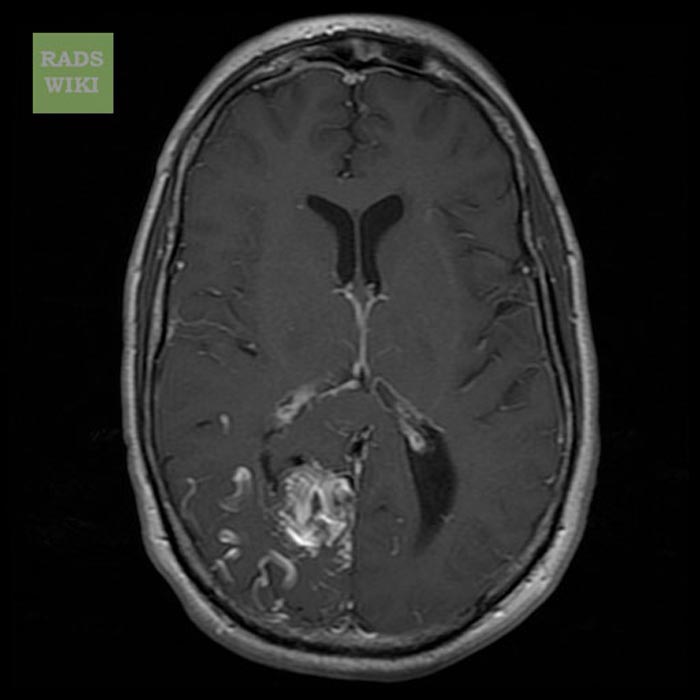
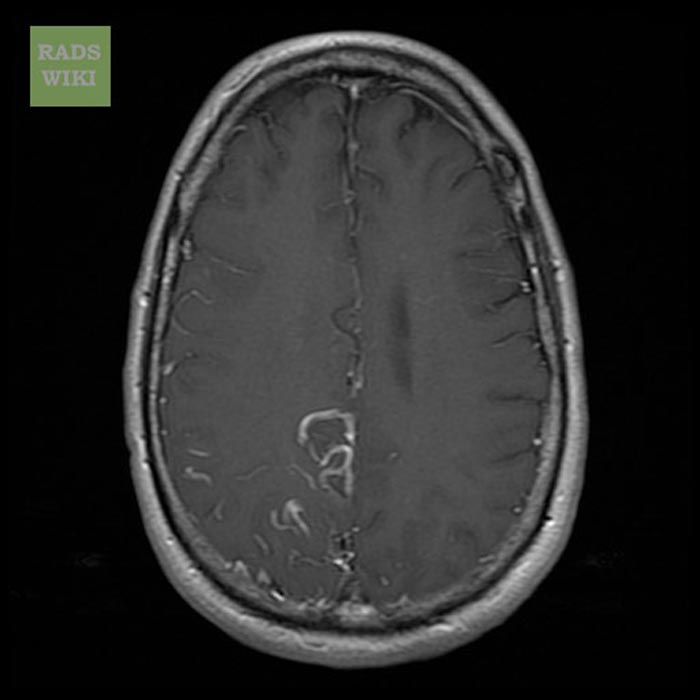
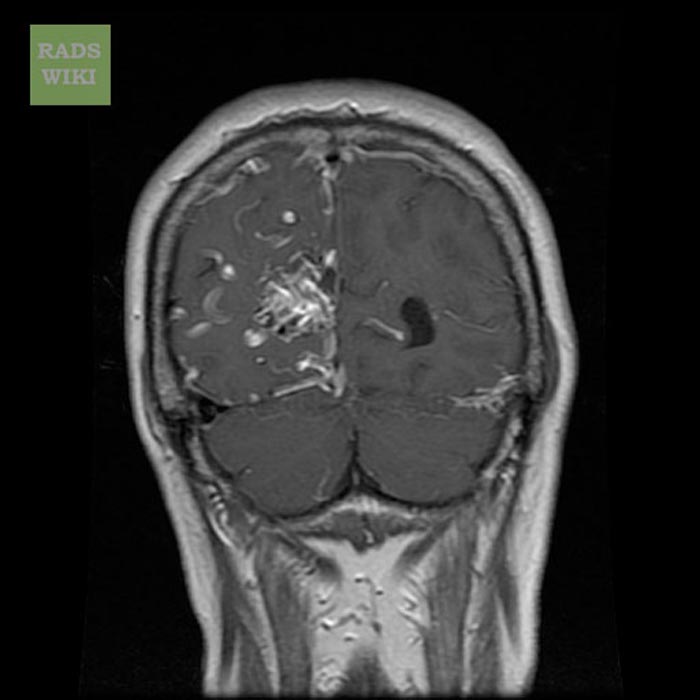
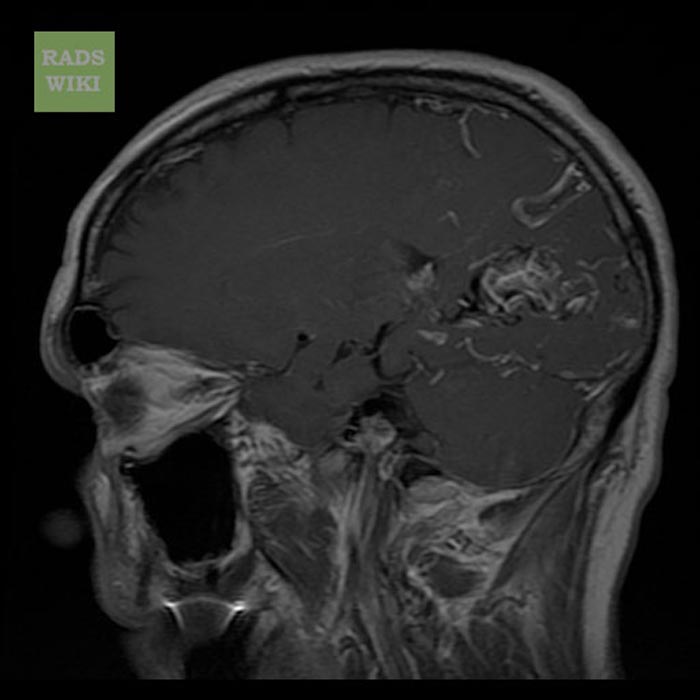
More detailed pictures of the tangle of blood vessels that compose an AVM can be obtained by using [[MRI]] head. | |||
Images shown below are courtesy of RadsWiki | Images shown below are courtesy of RadsWiki | ||
| Line 63: | Line 69: | ||
Image:Arteriovenous malformation008.jpg|T1 with GAD image shows a large right AVM | Image:Arteriovenous malformation008.jpg|T1 with GAD image shows a large right AVM | ||
</gallery> | </gallery> | ||
===[[Cerebral angiography]]=== | |||
This procedure involves using a catheter, threaded through an artery up to the head, to deliver a contrast agent into the AVM. As the contrast agent flows through the AVM structure, a sequence of X-ray images can be obtained to ascertain the size, shape and extent of that structure. This provides best images of AVM. | |||
'''Spetzler-Martin Grading System''' | |||
<table border="1" cellspacing="0" cellpadding="3"><tr> | |||
<th colspan="2">Size</th> | |||
<th colspan="2">Eloquence of adjacent brain<font size="2"></font></th> | |||
<th colspan="2">Venous drainage<font size="2"></font></th> | |||
</tr><tr><td>Small (<3 cm)</td><td align="center">1</td><td>Noneloquent</td><td align="center">0</td><td>Superficial only </td><td align="center">0</td></tr><tr><td>Medium (3-6 cm)</td><td align="center">2</td><td>Eloquent</td><td align="center">1</td><td>Deep component </td><td align="center">1</td></tr><tr><td>Large (>6 cm)</td><td align="center">3</td><td colspan="2" align="center">…</td><td colspan="2" align="center">…</td></tr></table> | |||
*Size: Measure the largest diameter of the nidus of the lesion on angiography.<br> | |||
*Eloquence: Eloquent areas include sensorimotor, language, visual, thalamus, hypothalamus, internal capsule, brain stem, cerebellar peduncles, and deep cerebellar nuclei.<br> | |||
*Venous drainage: The lesion is considered superficial only if all drainage is via the cortical drainage system. | |||
==Treatment== | ==Treatment== | ||
The treatment in the case of sudden bleeding is focused on restoration of vital function. | ===Medical Therapy=== | ||
The treatment in the case of sudden bleeding is focused on restoration of vital function. | |||
In the U.S., surgical removal of the blood vessels involved ([[craniotomy]]) is the preferred curative treatment for most types of AVM. | * Anticonvulsant medications such as [[phenytoin]] are often used to control seizure | ||
* Medications or procedures may be employed to relieve intracranial pressure. | |||
* Eventually, curative treatment may be required to prevent recurrent hemorrhage. | |||
===Surgery=== | |||
[[Embolization]] | In the U.S., surgical removal of the blood vessels involved ([[craniotomy]]) is the preferred curative treatment for most types of AVM. While this surgery results in an immediate, complete removal of the AVM, risks exist depending on the size and the location of the malformation. | ||
===Radiation therapy=== | |||
[[Radiosurgery]] has been widely used on smaller AVMs with considerable success. The Gamma Knife, developed by Swedish physician Lars Leksell, is one apparatus used in radiosurgery to precisely apply a controlled radiation dosage to the volume of the brain occupied by the AVM. While this treatment is [[non-invasive]], two to three years may pass before the complete effects are known. Complete [[occlusion]] of the AVM may or may not occur, and 8%-10% of patients develop long term neurological symptoms after radiation. | |||
===[[Embolization]]=== | |||
Occlusion of blood vessels with coils or particles introduced by a radiographically guided catheter, is frequently used as an adjunct to either surgery or radiation treatment. However, embolization alone is rarely successful in completely blocking blood flow through the AVM. | |||
==References== | ==References== | ||
{{reflist|2}} | {{reflist|2}} | ||
{{Congenital malformations and deformations of circulatory system}} | {{Congenital malformations and deformations of circulatory system}} | ||
| Line 94: | Line 104: | ||
[[Category:Congenital disorders]] | [[Category:Congenital disorders]] | ||
[[Category:Cardiology]] | [[Category:Cardiology]] | ||
[[Category:Disease]] | |||
[[ja:脳動静脈奇形]] | [[ja:脳動静脈奇形]] | ||
Revision as of 16:06, 24 July 2012
| Cerebral arteriovenous malformation | |
 | |
|---|---|
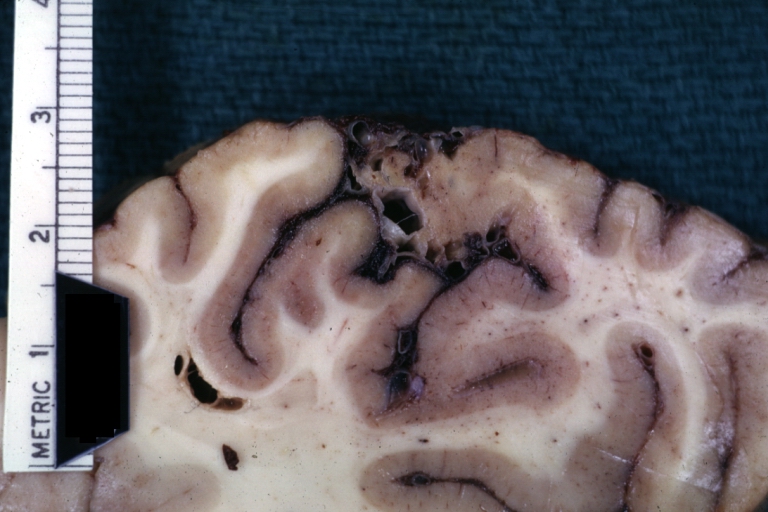
| Brain: Arteriovenous Malformation: Gross fixed tissue close-up view of malformation in meninges and cerebral cortex. Image courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology | |
| ICD-10 | Q28.2 |
| ICD-9 | 747.81 |
| OMIM | 108010 |
| DiseasesDB | 2224 |
| MedlinePlus | 000779 |
| eMedicine | neuro/21 |
| MeSH | D002538 |
Template:Search infobox Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: :Kalsang Dolma, M.B.B.S.[2]
Synonyms and keywords: AVM
Overview
A cerebral arteriovenous malformation (AVM) is a congenital disorder of blood vessels within the brain, characterized by tangle(s) of veins and arteries. While an arteriovenous malformation can occur elsewhere in the body, this article discusses malformations found in the brain.
Pathophysiology
AVMs are an abnormal connection between the arteries and veins in the human brain. In a normal brain oxygen enriched blood from the heart travels in sequence through smaller blood vessels going from arteries, to arterioles and then capillaries.[1] Oxygen is removed in the latter vessel to be used by the brain.[1] After the oxygen is removed blood reaches venules and later veins which will take it back to the heart and lungs.[1] On the other hand when there is an AVM blood goes directly from arteries to veins through the abnormal vessels disrupting the normal circulation of blood.[1]
Causes
Arteriovenous malformations are most commonly of prenatal origin.[1] The cause of AVMs remains unknown.[1]
Epidemiology and Demographics
- The annual new detection rate incidence of AVMs is approximately 1 per 100000 a year. The point prevalence in adults is approximately 18 per 100000.[2]
- AVMs are more common in males than females, although in females pregnancy may start or worsen symptoms due the increase in blood flow and volume it usually brings.[3]
Diagnosis
History and Symptoms
The most frequently observed problems related to an AVM are
- Headache
- Seizure
- Symptoms of intracranial hemorrhage may be present which include
- loss of consciousness
- nausea
- vomiting
- incontinence
- blurred vision
- hemiparesis
- aphasia
- a loss of touch sensation on one side of the body
Physical Examination
HEENT
- Hydrocephalus may be present
Neurologic
- Meningeal signs may be present
- hemiparesis may be present
- aphasia may be present
- Hemianesthesia may be present
Laboratory findings
Lumbar puncture
Lumbar puncture can be used to examine spinal fluid for red blood cells; this condition is indicative of leakage of blood from the bleeding vessels into the subarachnoid space.
CT
CT head can reveal the site of the bleed.
MRI
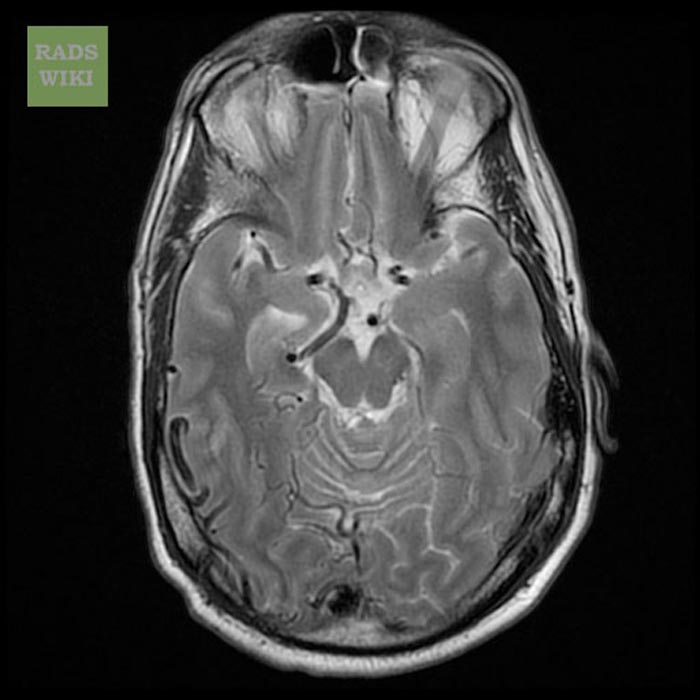
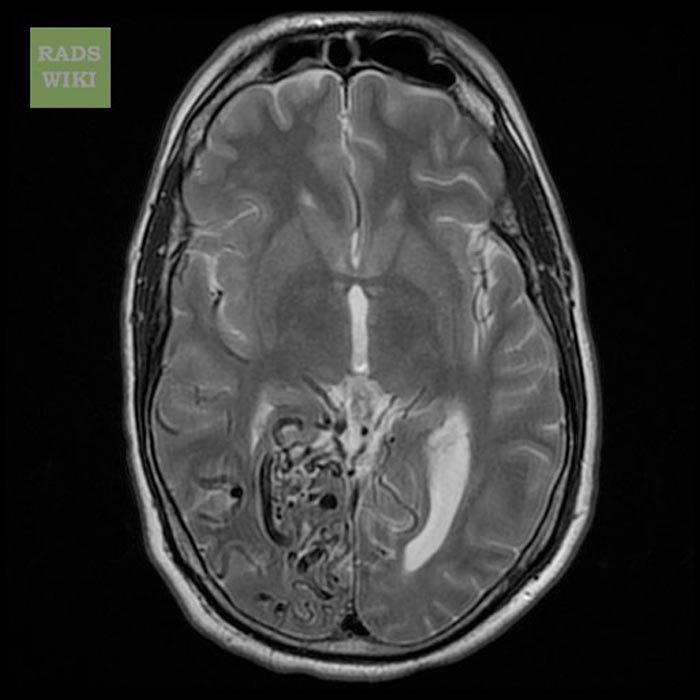
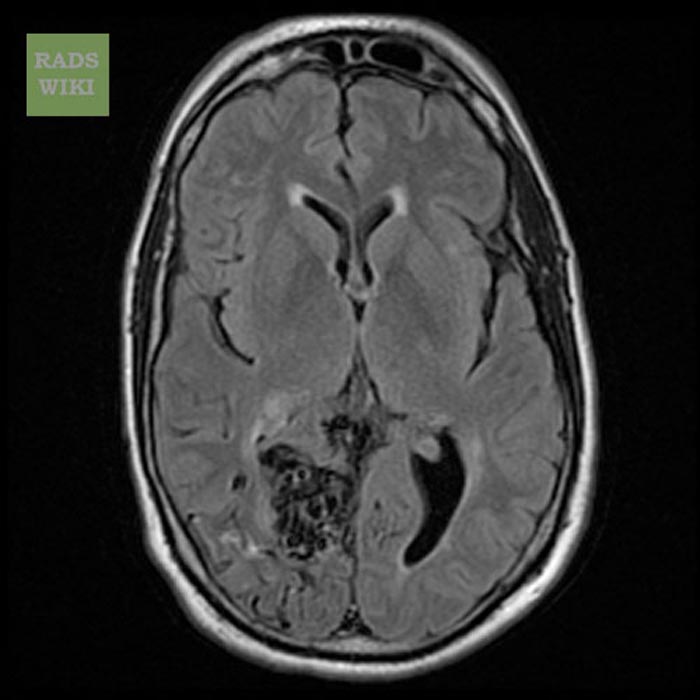
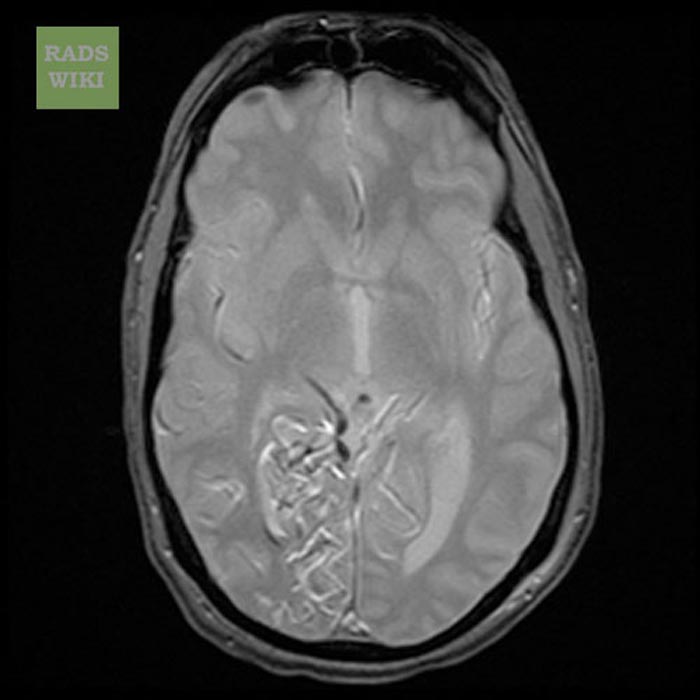
More detailed pictures of the tangle of blood vessels that compose an AVM can be obtained by using MRI head.
Images shown below are courtesy of RadsWiki
-
T2 image shows a large right AVM
-
T2 image shows a large right AVM
-
FLAIR image shows a large right AVM
-
GRE image shows a large right AVM
-
T1 with GAD image shows a large right AVM
-
T1 with GAD image shows a large right AVM
-
T1 with GAD image shows a large right AVM
-
T1 with GAD image shows a large right AVM
Cerebral angiography
This procedure involves using a catheter, threaded through an artery up to the head, to deliver a contrast agent into the AVM. As the contrast agent flows through the AVM structure, a sequence of X-ray images can be obtained to ascertain the size, shape and extent of that structure. This provides best images of AVM.
Spetzler-Martin Grading System
| Size | Eloquence of adjacent brain | Venous drainage | |||
|---|---|---|---|---|---|
| Small (<3 cm) | 1 | Noneloquent | 0 | Superficial only | 0 |
| Medium (3-6 cm) | 2 | Eloquent | 1 | Deep component | 1 |
| Large (>6 cm) | 3 | … | … | ||
- Size: Measure the largest diameter of the nidus of the lesion on angiography.
- Eloquence: Eloquent areas include sensorimotor, language, visual, thalamus, hypothalamus, internal capsule, brain stem, cerebellar peduncles, and deep cerebellar nuclei.
- Venous drainage: The lesion is considered superficial only if all drainage is via the cortical drainage system.
Treatment
Medical Therapy
The treatment in the case of sudden bleeding is focused on restoration of vital function.
- Anticonvulsant medications such as phenytoin are often used to control seizure
- Medications or procedures may be employed to relieve intracranial pressure.
- Eventually, curative treatment may be required to prevent recurrent hemorrhage.
Surgery
In the U.S., surgical removal of the blood vessels involved (craniotomy) is the preferred curative treatment for most types of AVM. While this surgery results in an immediate, complete removal of the AVM, risks exist depending on the size and the location of the malformation.
Radiation therapy
Radiosurgery has been widely used on smaller AVMs with considerable success. The Gamma Knife, developed by Swedish physician Lars Leksell, is one apparatus used in radiosurgery to precisely apply a controlled radiation dosage to the volume of the brain occupied by the AVM. While this treatment is non-invasive, two to three years may pass before the complete effects are known. Complete occlusion of the AVM may or may not occur, and 8%-10% of patients develop long term neurological symptoms after radiation.
Embolization
Occlusion of blood vessels with coils or particles introduced by a radiographically guided catheter, is frequently used as an adjunct to either surgery or radiation treatment. However, embolization alone is rarely successful in completely blocking blood flow through the AVM.
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 Mayo Clinic staff (2009). "Brain AVM (arteriovenous malformation)-Causes". Mayo Foundation for Medical Education and Research. Retrieved 2010-05-30. Unknown parameter
|month=ignored (help) - ↑ Al-Shahi R, Warlow C (2001). "A systematic review of the frequency and prognosis of arteriovenous malformations of the brain in adults". Brain. 124 (Pt 10): 1900–26. doi:10.1093/brain/124.10.1900. PMID 11571210. Retrieved 2010-05-18. Unknown parameter
|month=ignored (help) - ↑ Mayo Clinic staff (2009). "Brain AVM (arteriovenous malformation)-Risk factors". Mayo Foundation for Medical Education and Research. Retrieved 2010-05-30. Unknown parameter
|month=ignored (help)