Calcium apatite deposition disease: Difference between revisions
m (Bot: Removing from Primary care) |
|||
| (47 intermediate revisions by 2 users not shown) | |||
| Line 4: | Line 4: | ||
{{CMG}} {{AE}} {{MKK}} | {{CMG}} {{AE}} {{MKK}} | ||
Synonyms: Calcific periarthritis | '''''Synonyms and Keywords: '''''Calcific periarthritis; calcific bursitis; periarthritis calcarea; hydroxyapatite rheumatism | ||
==Overview== | ==Overview== | ||
Calcium apatite deposition disease is a [[chronic]] condition usually characterized by deposition of calcium apatite crystals within and around [[connective tissues]] and [[tendons]], most commonly around the periarticular location. The risk factors for calcium apatite deposition disease are the genetic predisposition to [[HLA-A1|HLA-A1 gene]], newly onset adult [[diabetes]], [[estrogen]], and thyroid disorders. The most common site of involvement is [[shoulder]], mostly involving the [[supraspinatus]] and [[infraspinatus]] tendons. Next common location is [[hip]], followed by the [[spine]]. It occurs between the ages of 30–60, most common in [[females]] and usually asymptomatic. The patient also present with acute episodes of [[pain]], which is recurrent after one episode. Common symptoms are the [[pain]] and [[swelling]] of the involved joint. Physical examination shows restricted [[joint]] movements and [[swelling]]. Diagnosis is made by radiography. [[MRI]] is the gold standard for the diagnosis of [[calcification]]. Treatment is usually conservative such as [[NSAIDS]], [[physiotherapy]], and hot compresses. Those are refractory to conservative treatment are referred to surgical treatment like open [[resection]], [[arthroscopic]] [[resection]], [[ultrasound]]-guided needle lavage ([[barbotage]]), and [[extracorporeal shockwave therapy]] (ESWT). | |||
==Historical Perspective== | ==Historical Perspective== | ||
*[ | *In 1966, McCarty and Gatten had found [[calcium hydroxyapatite]] as the crystal involved in idiopathic calcific periarthritis. | ||
*In [ | *In 2001 and 2006, Hamada had identified the [[calcium]] deposits of [[calcific tendinitis]] to be made up of carbonate apatite instead of [[hydroxyapatite]].<ref name="pmid11327256">{{cite journal |vauthors=Hamada J, Ono W, Tamai K, Saotome K, Hoshino T |title=Analysis of calcium deposits in calcific periarthritis |journal=J. Rheumatol. |volume=28 |issue=4 |pages=809–13 |date=April 2001 |pmid=11327256 |doi= |url=}}</ref><ref name="pmid16465665">{{cite journal |vauthors=Hamada J, Tamai K, Ono W, Saotome K |title=Does the nature of deposited basic calcium phosphate crystals determine clinical course in calcific periarthritis of the shoulder? |journal=J. Rheumatol. |volume=33 |issue=2 |pages=326–32 |date=February 2006 |pmid=16465665 |doi= |url=}}</ref> | ||
==Classification== | ==Classification== | ||
*Calcium apatite deposition disease may be classified into two phases based on symptoms:<ref name="pmid28042481">{{cite journal |vauthors=Beckmann NM |title=Calcium Apatite Deposition Disease: Diagnosis and Treatment |journal=Radiol Res Pract |volume=2016 |issue= |pages=4801474 |date=2016 |pmid=28042481 |pmc=5155096 |doi=10.1155/2016/4801474 |url=}}</ref> | |||
**Acutely [[symptomatic]] phase | |||
**[[Chronic]] or asymptomatic phase | |||
*Based on the duration of symptoms, calcium apatite deposition disease may be classified as either acute or chronic. | |||
==Pathophysiology== | ==Pathophysiology== | ||
*The pathogenesis of calcium apatite deposition disease is not clear. Various authors have formulated the different hypothesis about the pathophysiology of calcium apatite deposition disease. | *The pathogenesis of calcium apatite deposition disease is not clear. Various authors have formulated the different hypothesis about the pathophysiology of calcium apatite deposition disease. | ||
*Uhthoff and Loebr described the pathogenesis in four phases: | *Uhthoff and Loebr described the pathogenesis in four phases which include:<ref name="pmid10797220">{{cite journal |vauthors=Uhthoff HK, Loehr JW |title=Calcific Tendinopathy of the Rotator Cuff: Pathogenesis, Diagnosis, and Management |journal=J Am Acad Orthop Surg |volume=5 |issue=4 |pages=183–191 |date=July 1997 |pmid=10797220 |doi= |url=}}</ref> | ||
**Precalcific phase: In this | **'''Precalcific phase''': In this phase, [[fibrocartilage]] [[tissue]] is formed due to the [[metaplasia]] of [[collagen]] fibers of the [[tendon]]. | ||
**Formative phase: | **'''Formative phase''': In this phase, in the areas of [[fibrocartilage]] [[Formation matrix|formation]], [[Chondrocyte|chondrocytes]] start depositing which further leads to the formation of calcified apatite crystals. Sometimes calcified apatite crystal will go into the '''resting''' '''phase''' for long period of time. | ||
**'''Resorptive phase''': In this phase, [[calcification]] will further undergo to an [[inflammatory]] resorptive phase, which is characterized by the prsence of [[leukocytes]], [[lymphocytes]], and [[giant cells]] leading to the formation of a calcium granuloma. | |||
**Resorptive phase: | **'''Postcalcific phase''': Reparative process allows new [[capillary]] and [[collagen]] fiber formation that is when [[calcification]] enters the postcalcific phase. | ||
**Postcalcific phase: Reparative process allows new capillary and collagen fiber formation that is when calcification enters the postcalcific phase. | *The [[HLA-A1]] [[gene]] has been associated with the development of calcium apatite deposition disease.<ref name="pmid3496685">{{cite journal |vauthors=Sengar DP, McKendry RJ, Uhthoff HK |title=Increased frequency of HLA-A1 in calcifying tendinitis |journal=Tissue Antigens |volume=29 |issue=3 |pages=173–4 |date=March 1987 |pmid=3496685 |doi= |url=}}</ref> | ||
*The HLA-A1 gene has been associated with the development of calcium apatite deposition disease.<ref name="pmid3496685">{{cite journal |vauthors=Sengar DP, McKendry RJ, Uhthoff HK |title=Increased frequency of HLA-A1 in calcifying tendinitis |journal=Tissue Antigens |volume=29 |issue=3 |pages=173–4 |date=March 1987 |pmid=3496685 |doi= |url=}}</ref> | |||
==Differentiating | ==Differentiating Calcium Apatite Deposition Disease from other Diseases== | ||
*Calcium apatite deposition disease must be differentiated from the following disease: | *Calcium apatite deposition disease must be differentiated from the following disease: | ||
**Calcium pyrophosphate dihydrate deposition disease (CPPD) | **Calcium pyrophosphate dihydrate deposition disease (CPPD) | ||
**Dystrophic calcification | **[[Dystrophic calcification]] | ||
**Renal osteodystrophy | **[[Renal]] [[osteodystrophy]] | ||
**Hyperparathyroidism | **[[Hyperparathyroidism]] | ||
**Hypoparathyroidism | **[[Hypoparathyroidism]] | ||
**Collagen vascular disease | **[[Collagen vascular diseases|Collagen vascular disease]] | ||
**Milk-alkali syndrome | **[[Milk-alkali syndrome]] | ||
**Hypervitaminosis D | **[[Hypervitaminosis D]] | ||
==Epidemiology and Demographics== | ==Epidemiology and Demographics== | ||
=== Prevalence === | |||
*The prevalence of calcium apatite deposition disease is approximately 7.8% in asymptomatic patients and 42.5% in patients with subacromial pain syndrome.<ref name="pmid28042481">{{cite journal |vauthors=Beckmann NM |title=Calcium Apatite Deposition Disease: Diagnosis and Treatment |journal=Radiol Res Pract |volume=2016 |issue= |pages=4801474 |date=2016 |pmid=28042481 |pmc=5155096 |doi=10.1155/2016/4801474 |url=}}</ref> | *The prevalence of calcium apatite deposition disease is approximately 7.8% in asymptomatic patients and 42.5% in patients with subacromial pain syndrome.<ref name="pmid28042481">{{cite journal |vauthors=Beckmann NM |title=Calcium Apatite Deposition Disease: Diagnosis and Treatment |journal=Radiol Res Pract |volume=2016 |issue= |pages=4801474 |date=2016 |pmid=28042481 |pmc=5155096 |doi=10.1155/2016/4801474 |url=}}</ref> | ||
===Age=== | ===Age=== | ||
*Calcium apatite deposition disease | *Calcium apatite deposition disease has a bimodal pattern which affects both children around 3 years of age and adult between 30–60 years old.<ref name="pmid25870115">{{cite journal |vauthors=Louwerens JK, Sierevelt IN, van Hove RP, van den Bekerom MP, van Noort A |title=Prevalence of calcific deposits within the rotator cuff tendons in adults with and without subacromial pain syndrome: clinical and radiologic analysis of 1219 patients |journal=J Shoulder Elbow Surg |volume=24 |issue=10 |pages=1588–93 |date=October 2015 |pmid=25870115 |doi=10.1016/j.jse.2015.02.024 |url=}}</ref><ref name="pmid11845156">{{cite journal |vauthors=Sakamoto K, Kozuki K |title=Calcific tendinitis at the biceps brachii insertion of a child: a case report |journal=J Shoulder Elbow Surg |volume=11 |issue=1 |pages=88–91 |date=2002 |pmid=11845156 |doi=10.1067/mse.2002.119854 |url=}}</ref> | ||
===Gender=== | ===Gender=== | ||
| Line 51: | Line 52: | ||
==Risk Factors== | ==Risk Factors== | ||
*Common risk factors in the development of calcium apatite deposition disease are: | *Common risk factors in the [[development]] of calcium apatite deposition disease are: | ||
** | **Genetic predisposition to the [[HLA-A1]] gene <ref name="pmid3496685">{{cite journal |vauthors=Sengar DP, McKendry RJ, Uhthoff HK |title=Increased frequency of HLA-A1 in calcifying tendinitis |journal=Tissue Antigens |volume=29 |issue=3 |pages=173–4 |date=March 1987 |pmid=3496685 |doi= |url=}}</ref> | ||
**Adult-onset diabetes | **Adult-onset [[diabetes mellitus]]<ref name="pmid2930276">{{cite journal |vauthors=Mavrikakis ME, Drimis S, Kontoyannis DA, Rasidakis A, Moulopoulou ES, Kontoyannis S |title=Calcific shoulder periarthritis (tendinitis) in adult onset diabetes mellitus: a controlled study |journal=Ann. Rheum. Dis. |volume=48 |issue=3 |pages=211–4 |date=March 1989 |pmid=2930276 |pmc=1003723 |doi= |url=}}</ref> | ||
**Thyroid | **[[Thyroid disease|Thyroid disorders]] | ||
**Estrogen hormone disorder<ref name="pmid17188907">{{cite journal |vauthors=Harvie P, Pollard TC, Carr AJ |title=Calcific tendinitis: natural history and association with endocrine disorders |journal=J Shoulder Elbow Surg |volume=16 |issue=2 |pages=169–73 |date=2007 |pmid=17188907 |doi=10.1016/j.jse.2006.06.007 |url=}}</ref> | |||
== Natural History, Complications and Prognosis== | == Natural History, Complications and Prognosis== | ||
*The majority of patients with calcium apatite deposition disease remain asymptomatic for an indefinite period of time. | *The majority of patients with calcium apatite deposition disease may remain asymptomatic for an indefinite period of time. | ||
*Early clinical features include acute pain or chronic mild pain. | *Early clinical features include acute [[pain]] or chronic mild pain. | ||
*If left untreated, intraarticular calcification may progress to develop joint destruction. | *If left untreated, [[intraarticular]] calcification may progress to develop [[joint]] destruction. | ||
*Common complications of calcium apatite deposition disease | *Common complications of calcium apatite deposition disease | ||
**Intraarticular calcification | **Intraarticular calcification | ||
**Milwaukee shoulder syndrome | **[[Joint]] destruction | ||
**Milwaukee shoulder syndrome | |||
== Diagnosis == | == Diagnosis == | ||
| Line 69: | Line 72: | ||
=== Symptoms === | === Symptoms === | ||
*Patients with calcium apatite deposition disease are usually asymptomatic. | *Patients with calcium apatite deposition disease are usually [[asymptomatic]]. However, patients might experience following symptoms: | ||
* | **Acute episodes of [[pain]] which might be:<ref name="pmid23422589">{{cite journal |vauthors=Kim JK, Park ES |title=Acute calcium deposits in the hand and wrist; comparison of acute calcium peritendinitis and acute calcium periarthritis |journal=J Hand Surg Eur Vol |volume=39 |issue=4 |pages=436–9 |date=May 2014 |pmid=23422589 |doi=10.1177/1753193413478393 |url=}}</ref> | ||
*Acute episodes of pain | ***Spontaneously resolved | ||
* | ***Recurrent | ||
*Some patients also present with the symptoms of neuropathy | ***Associated with [[swelling]] | ||
**Chronic mild [[pain]] | |||
*Some patients also present with the symptoms of [[neuropathy]] such as: <ref name="pmid20936391">{{cite journal |vauthors=Garayoa SA, Romero-Muñoz LM, Pons-Villanueva J |title=Acute compartment syndrome of the forearm caused by calcific tendinitis of the distal biceps |journal=Musculoskelet Surg |volume=94 |issue=3 |pages=137–9 |date=December 2010 |pmid=20936391 |doi=10.1007/s12306-010-0079-2 |url=}}</ref> | |||
**[[Weakness]] | |||
**[[Tingling]] | |||
**[[Paresthesia|Numbness]] | |||
*If it involves [[Longus colli muscle|longus colli muscle]], following symptoms are experienced by the patient which include:<ref name="pmid23192216">{{cite journal |vauthors=Paik NC, Lim CS, Jang HS |title=Tendinitis of longus colli: computed tomography, magnetic resonance imaging, and clinical spectra of 9 cases |journal=J Comput Assist Tomogr |volume=36 |issue=6 |pages=755–61 |date=2012 |pmid=23192216 |doi=10.1097/RCT.0b013e318269880c |url=}}</ref><ref name="pmid23525848">{{cite journal |vauthors=Horowitz G, Ben-Ari O, Brenner A, Fliss DM, Wasserzug O |title=Incidence of retropharyngeal calcific tendinitis (longus colli tendinitis) in the general population |journal=Otolaryngol Head Neck Surg |volume=148 |issue=6 |pages=955–8 |date=June 2013 |pmid=23525848 |doi=10.1177/0194599813482289 |url=}}</ref> | |||
**[[Neck pain]] | |||
**Decreased range of motion | |||
**[[Neck stiffness]] | |||
**[[Odynophagia]] | |||
**[[Dysphagia]] | |||
=== Physical Examination === | === Physical Examination === | ||
*Patients with calcium apatite deposition disease usually appear | *Patients with calcium apatite deposition disease usually appear tired and in [[pain]]. | ||
*Physical examination of the involved joint is remarkable for: | *Physical examination of the involved [[joint]] is remarkable for: | ||
**Redness | **[[Redness]] | ||
**Swelling | **[[Swelling]] | ||
** | **Warmth | ||
**Restricted range of movement | |||
*Some patients show signs of [[neuropathy]] such as: | |||
**[[Muscle weakness|Weakness]] | |||
**Decreased [[sensation]] | |||
**[[Hyporeflexia]] | |||
=== Laboratory Findings === | === Laboratory Findings === | ||
*There are no specific laboratory findings associated with calcium apatite deposition disease. | *There are no specific laboratory findings associated with calcium apatite deposition disease. | ||
*Some of the general tests indicating [[inflammation]] are abnormal which includes: | |||
**Increased [[ESR]] | |||
**Increased [[CRP]] | |||
===Imaging Findings=== | ===Imaging Findings=== | ||
* | *X-ray is used to see calcification in affected joint.<ref name="pmid10797220">{{cite journal |vauthors=Uhthoff HK, Loehr JW |title=Calcific Tendinopathy of the Rotator Cuff: Pathogenesis, Diagnosis, and Management |journal=J Am Acad Orthop Surg |volume=5 |issue=4 |pages=183–191 |date=July 1997 |pmid=10797220 |doi= |url=}}</ref> | ||
*CT scan is not used to diagnose, but it is used to find out deep tissue [[infections]] and soft tissue [[edema]].<ref name="pmid2157572">{{cite journal |vauthors=Gärtner J, Simons B |title=Analysis of calcific deposits in calcifying tendinitis |journal=Clin. Orthop. Relat. Res. |volume= |issue=254 |pages=111–20 |date=May 1990 |pmid=2157572 |doi= |url=}}</ref> | |||
*[ | *[[Ultrasound]] is not used for diagnosis, but it is used in image-guided treatment of the calcifications.<ref name="pmid11516532">{{cite journal |vauthors=Chiou HJ, Chou YH, Wu JJ, Huang TF, Ma HL, Hsu CC, Chang CY |title=The role of high-resolution ultrasonography in management of calcific tendonitis of the rotator cuff |journal=Ultrasound Med Biol |volume=27 |issue=6 |pages=735–43 |date=June 2001 |pmid=11516532 |doi= |url=}}</ref> | ||
*On | *MRI is the imaging modality of choice for calcium apatite deposition disease. | ||
*[ | *On MRI, calcification is characterized by:<ref name="pmid23729205">{{cite journal |vauthors=Garner HW, Whalen JL |title=Acute calcific tendinosis of the flexor hallucis brevis: case report |journal=Foot Ankle Int |volume=34 |issue=10 |pages=1451–5 |date=October 2013 |pmid=23729205 |doi=10.1177/1071100713491562 |url=}}</ref> | ||
**Homogeneous and discrete calcifications | |||
= | **Ill-defined inhomogeneous calcifications | ||
**Soft tissue edema | |||
[[Image:Calcific-tendinitis-6 (1).jpg|200px|left|thumbnail|Calcific-tendinitis of the shoulder joint <br> Source :Case courtesy of Dr Andrew Lawson, <ref>href="https://radiopaedia.org/">Radiopaedia.org</ref><ref>href="https://radiopaedia.org/cases/25858">rID: 25858</ref>]] | |||
[[Image:Calcific-tendinitis-of-the-longus-colli-muscle-1.jpg|200px|left|thumbnail|Calcific tendinitis of the longuscolli muscle <br> Source:Case courtesy of Dr Behrang Amini,<ref>href="https://radiopaedia.org/">Radiopaedia.org</ref><ref>href="https://radiopaedia.org/cases/36426">rID: 36426</ref>]] | |||
<br style="clear:left" /> | |||
== Treatment == | == Treatment == | ||
=== Medical Therapy === | === Medical Therapy === | ||
*There is | *There is the conservative treatment for the [[pain]]. Most of the calcifications resolve in size with conservative therapy.<ref name="pmid19800263">{{cite journal |vauthors=Cho NS, Lee BG, Rhee YG |title=Radiologic course of the calcific deposits in calcific tendinitis of the shoulder: does the initial radiologic aspect affect the final results? |journal=J Shoulder Elbow Surg |volume=19 |issue=2 |pages=267–72 |date=March 2010 |pmid=19800263 |doi=10.1016/j.jse.2009.07.008 |url=}}</ref> | ||
*Conservative treatment options are [[NSAIDS]], hot compresses, and [[physiotherapy]]. | |||
* | *Patients refractory to conservative therapy, following options are used: | ||
*[ | **[[Platelet]]-rich plasma injection | ||
* | **[[Steroid]] injection | ||
=== Surgery === | === Surgery === | ||
*Surgery is the | *Surgery is the choice of therapy for [[refractory]] cases of calcium apatite deposition disease. Following options are used:<ref name="pmid10468172">{{cite journal |vauthors=Rochwerger A, Franceschi JP, Viton JM, Roux H, Mattei JP |title=Surgical management of calcific tendinitis of the shoulder: an analysis of 26 cases |journal=Clin. Rheumatol. |volume=18 |issue=4 |pages=313–6 |date=1999 |pmid=10468172 |doi= |url=}}</ref><ref name="pmid24774621">{{cite journal |vauthors=Louwerens JK, Sierevelt IN, van Noort A, van den Bekerom MP |title=Evidence for minimally invasive therapies in the management of chronic calcific tendinopathy of the rotator cuff: a systematic review and meta-analysis |journal=J Shoulder Elbow Surg |volume=23 |issue=8 |pages=1240–9 |date=August 2014 |pmid=24774621 |doi=10.1016/j.jse.2014.02.002 |url=}}</ref> | ||
*[ | **Open [[resection]] | ||
*[ | **[[Arthroscopic]] [[resection]] | ||
**[[Ultrasound]]-guided needle lavage (barbotage) | |||
**[[Extracorporeal shockwave therapy]] (ESWT) | |||
=== Prevention === | === Prevention === | ||
*There | *There is no primary prevention for calcium apatite deposition disease. | ||
==References== | ==References== | ||
{{Reflist|2}} | {{Reflist|2}} | ||
[[Category:Medicine]] | |||
[[Category:Rheumatology]] | |||
[[Category:Up-To-Date]] | |||
Latest revision as of 20:46, 29 July 2020
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Manpreet Kaur, MD [2]
Synonyms and Keywords: Calcific periarthritis; calcific bursitis; periarthritis calcarea; hydroxyapatite rheumatism
Overview
Calcium apatite deposition disease is a chronic condition usually characterized by deposition of calcium apatite crystals within and around connective tissues and tendons, most commonly around the periarticular location. The risk factors for calcium apatite deposition disease are the genetic predisposition to HLA-A1 gene, newly onset adult diabetes, estrogen, and thyroid disorders. The most common site of involvement is shoulder, mostly involving the supraspinatus and infraspinatus tendons. Next common location is hip, followed by the spine. It occurs between the ages of 30–60, most common in females and usually asymptomatic. The patient also present with acute episodes of pain, which is recurrent after one episode. Common symptoms are the pain and swelling of the involved joint. Physical examination shows restricted joint movements and swelling. Diagnosis is made by radiography. MRI is the gold standard for the diagnosis of calcification. Treatment is usually conservative such as NSAIDS, physiotherapy, and hot compresses. Those are refractory to conservative treatment are referred to surgical treatment like open resection, arthroscopic resection, ultrasound-guided needle lavage (barbotage), and extracorporeal shockwave therapy (ESWT).
Historical Perspective
- In 1966, McCarty and Gatten had found calcium hydroxyapatite as the crystal involved in idiopathic calcific periarthritis.
- In 2001 and 2006, Hamada had identified the calcium deposits of calcific tendinitis to be made up of carbonate apatite instead of hydroxyapatite.[1][2]
Classification
- Calcium apatite deposition disease may be classified into two phases based on symptoms:[3]
- Acutely symptomatic phase
- Chronic or asymptomatic phase
- Based on the duration of symptoms, calcium apatite deposition disease may be classified as either acute or chronic.
Pathophysiology
- The pathogenesis of calcium apatite deposition disease is not clear. Various authors have formulated the different hypothesis about the pathophysiology of calcium apatite deposition disease.
- Uhthoff and Loebr described the pathogenesis in four phases which include:[4]
- Precalcific phase: In this phase, fibrocartilage tissue is formed due to the metaplasia of collagen fibers of the tendon.
- Formative phase: In this phase, in the areas of fibrocartilage formation, chondrocytes start depositing which further leads to the formation of calcified apatite crystals. Sometimes calcified apatite crystal will go into the resting phase for long period of time.
- Resorptive phase: In this phase, calcification will further undergo to an inflammatory resorptive phase, which is characterized by the prsence of leukocytes, lymphocytes, and giant cells leading to the formation of a calcium granuloma.
- Postcalcific phase: Reparative process allows new capillary and collagen fiber formation that is when calcification enters the postcalcific phase.
- The HLA-A1 gene has been associated with the development of calcium apatite deposition disease.[5]
Differentiating Calcium Apatite Deposition Disease from other Diseases
- Calcium apatite deposition disease must be differentiated from the following disease:
- Calcium pyrophosphate dihydrate deposition disease (CPPD)
- Dystrophic calcification
- Renal osteodystrophy
- Hyperparathyroidism
- Hypoparathyroidism
- Collagen vascular disease
- Milk-alkali syndrome
- Hypervitaminosis D
Epidemiology and Demographics
Prevalence
- The prevalence of calcium apatite deposition disease is approximately 7.8% in asymptomatic patients and 42.5% in patients with subacromial pain syndrome.[3]
Age
- Calcium apatite deposition disease has a bimodal pattern which affects both children around 3 years of age and adult between 30–60 years old.[6][7]
Gender
- Women are more commonly affected with calcium apatite deposition disease than men.[6]
Race
- There is no racial predilection for calcium apatite deposition disease.
Risk Factors
- Common risk factors in the development of calcium apatite deposition disease are:
- Genetic predisposition to the HLA-A1 gene [5]
- Adult-onset diabetes mellitus[8]
- Thyroid disorders
- Estrogen hormone disorder[9]
Natural History, Complications and Prognosis
- The majority of patients with calcium apatite deposition disease may remain asymptomatic for an indefinite period of time.
- Early clinical features include acute pain or chronic mild pain.
- If left untreated, intraarticular calcification may progress to develop joint destruction.
- Common complications of calcium apatite deposition disease
- Intraarticular calcification
- Joint destruction
- Milwaukee shoulder syndrome
Diagnosis
Diagnostic Criteria
According to the American association of rheumatology, there is no diagnostic criteria of calcium apatite deposition disease.
Symptoms
- Patients with calcium apatite deposition disease are usually asymptomatic. However, patients might experience following symptoms:
- Some patients also present with the symptoms of neuropathy such as: [11]
- If it involves longus colli muscle, following symptoms are experienced by the patient which include:[12][13]
- Neck pain
- Decreased range of motion
- Neck stiffness
- Odynophagia
- Dysphagia
Physical Examination
- Patients with calcium apatite deposition disease usually appear tired and in pain.
- Physical examination of the involved joint is remarkable for:
- Some patients show signs of neuropathy such as:
- Weakness
- Decreased sensation
- Hyporeflexia
Laboratory Findings
- There are no specific laboratory findings associated with calcium apatite deposition disease.
- Some of the general tests indicating inflammation are abnormal which includes:
Imaging Findings
- X-ray is used to see calcification in affected joint.[4]
- CT scan is not used to diagnose, but it is used to find out deep tissue infections and soft tissue edema.[14]
- Ultrasound is not used for diagnosis, but it is used in image-guided treatment of the calcifications.[15]
- MRI is the imaging modality of choice for calcium apatite deposition disease.
- On MRI, calcification is characterized by:[16]
- Homogeneous and discrete calcifications
- Ill-defined inhomogeneous calcifications
- Soft tissue edema

Source :Case courtesy of Dr Andrew Lawson, [17][18]
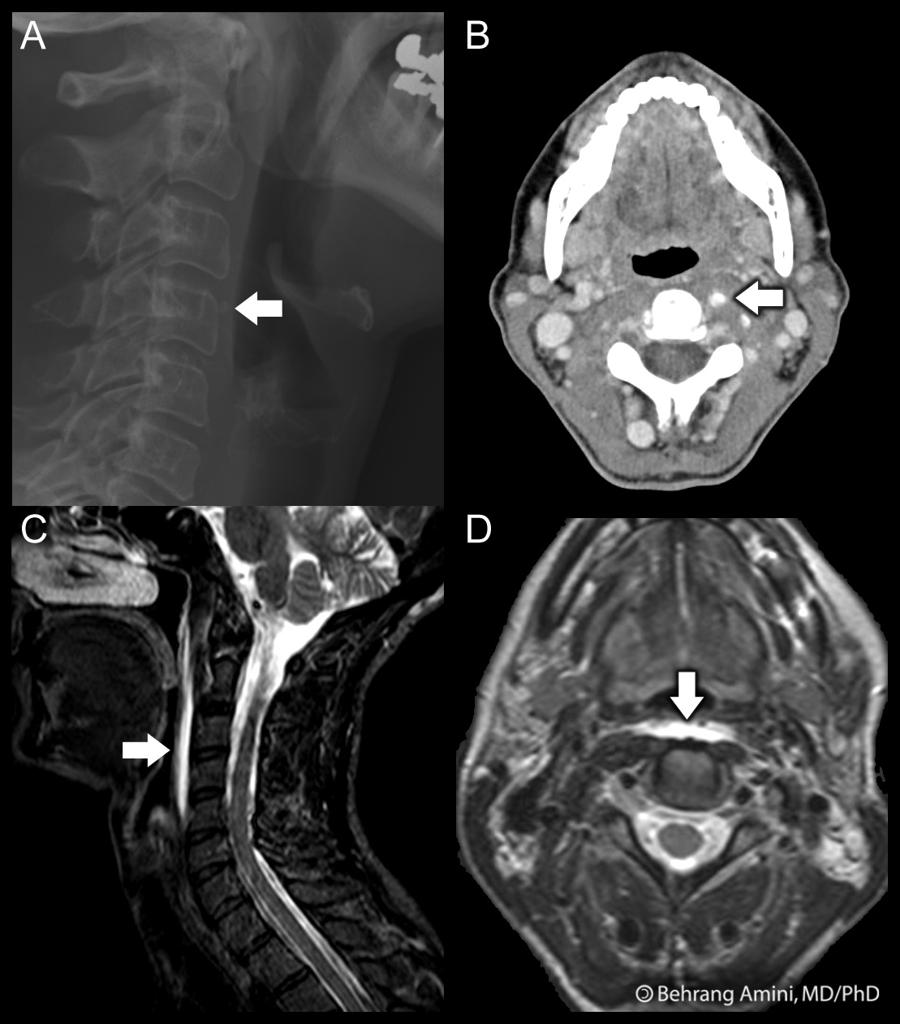
Source:Case courtesy of Dr Behrang Amini,[19][20]
Treatment
Medical Therapy
- There is the conservative treatment for the pain. Most of the calcifications resolve in size with conservative therapy.[21]
- Conservative treatment options are NSAIDS, hot compresses, and physiotherapy.
- Patients refractory to conservative therapy, following options are used:
Surgery
- Surgery is the choice of therapy for refractory cases of calcium apatite deposition disease. Following options are used:[22][23]
- Open resection
- Arthroscopic resection
- Ultrasound-guided needle lavage (barbotage)
- Extracorporeal shockwave therapy (ESWT)
Prevention
- There is no primary prevention for calcium apatite deposition disease.
References
- ↑ Hamada J, Ono W, Tamai K, Saotome K, Hoshino T (April 2001). "Analysis of calcium deposits in calcific periarthritis". J. Rheumatol. 28 (4): 809–13. PMID 11327256.
- ↑ Hamada J, Tamai K, Ono W, Saotome K (February 2006). "Does the nature of deposited basic calcium phosphate crystals determine clinical course in calcific periarthritis of the shoulder?". J. Rheumatol. 33 (2): 326–32. PMID 16465665.
- ↑ 3.0 3.1 Beckmann NM (2016). "Calcium Apatite Deposition Disease: Diagnosis and Treatment". Radiol Res Pract. 2016: 4801474. doi:10.1155/2016/4801474. PMC 5155096. PMID 28042481.
- ↑ 4.0 4.1 Uhthoff HK, Loehr JW (July 1997). "Calcific Tendinopathy of the Rotator Cuff: Pathogenesis, Diagnosis, and Management". J Am Acad Orthop Surg. 5 (4): 183–191. PMID 10797220.
- ↑ 5.0 5.1 Sengar DP, McKendry RJ, Uhthoff HK (March 1987). "Increased frequency of HLA-A1 in calcifying tendinitis". Tissue Antigens. 29 (3): 173–4. PMID 3496685.
- ↑ 6.0 6.1 Louwerens JK, Sierevelt IN, van Hove RP, van den Bekerom MP, van Noort A (October 2015). "Prevalence of calcific deposits within the rotator cuff tendons in adults with and without subacromial pain syndrome: clinical and radiologic analysis of 1219 patients". J Shoulder Elbow Surg. 24 (10): 1588–93. doi:10.1016/j.jse.2015.02.024. PMID 25870115.
- ↑ Sakamoto K, Kozuki K (2002). "Calcific tendinitis at the biceps brachii insertion of a child: a case report". J Shoulder Elbow Surg. 11 (1): 88–91. doi:10.1067/mse.2002.119854. PMID 11845156.
- ↑ Mavrikakis ME, Drimis S, Kontoyannis DA, Rasidakis A, Moulopoulou ES, Kontoyannis S (March 1989). "Calcific shoulder periarthritis (tendinitis) in adult onset diabetes mellitus: a controlled study". Ann. Rheum. Dis. 48 (3): 211–4. PMC 1003723. PMID 2930276.
- ↑ Harvie P, Pollard TC, Carr AJ (2007). "Calcific tendinitis: natural history and association with endocrine disorders". J Shoulder Elbow Surg. 16 (2): 169–73. doi:10.1016/j.jse.2006.06.007. PMID 17188907.
- ↑ Kim JK, Park ES (May 2014). "Acute calcium deposits in the hand and wrist; comparison of acute calcium peritendinitis and acute calcium periarthritis". J Hand Surg Eur Vol. 39 (4): 436–9. doi:10.1177/1753193413478393. PMID 23422589.
- ↑ Garayoa SA, Romero-Muñoz LM, Pons-Villanueva J (December 2010). "Acute compartment syndrome of the forearm caused by calcific tendinitis of the distal biceps". Musculoskelet Surg. 94 (3): 137–9. doi:10.1007/s12306-010-0079-2. PMID 20936391.
- ↑ Paik NC, Lim CS, Jang HS (2012). "Tendinitis of longus colli: computed tomography, magnetic resonance imaging, and clinical spectra of 9 cases". J Comput Assist Tomogr. 36 (6): 755–61. doi:10.1097/RCT.0b013e318269880c. PMID 23192216.
- ↑ Horowitz G, Ben-Ari O, Brenner A, Fliss DM, Wasserzug O (June 2013). "Incidence of retropharyngeal calcific tendinitis (longus colli tendinitis) in the general population". Otolaryngol Head Neck Surg. 148 (6): 955–8. doi:10.1177/0194599813482289. PMID 23525848.
- ↑ Gärtner J, Simons B (May 1990). "Analysis of calcific deposits in calcifying tendinitis". Clin. Orthop. Relat. Res. (254): 111–20. PMID 2157572.
- ↑ Chiou HJ, Chou YH, Wu JJ, Huang TF, Ma HL, Hsu CC, Chang CY (June 2001). "The role of high-resolution ultrasonography in management of calcific tendonitis of the rotator cuff". Ultrasound Med Biol. 27 (6): 735–43. PMID 11516532.
- ↑ Garner HW, Whalen JL (October 2013). "Acute calcific tendinosis of the flexor hallucis brevis: case report". Foot Ankle Int. 34 (10): 1451–5. doi:10.1177/1071100713491562. PMID 23729205.
- ↑ href="https://radiopaedia.org/">Radiopaedia.org
- ↑ href="https://radiopaedia.org/cases/25858">rID: 25858
- ↑ href="https://radiopaedia.org/">Radiopaedia.org
- ↑ href="https://radiopaedia.org/cases/36426">rID: 36426
- ↑ Cho NS, Lee BG, Rhee YG (March 2010). "Radiologic course of the calcific deposits in calcific tendinitis of the shoulder: does the initial radiologic aspect affect the final results?". J Shoulder Elbow Surg. 19 (2): 267–72. doi:10.1016/j.jse.2009.07.008. PMID 19800263.
- ↑ Rochwerger A, Franceschi JP, Viton JM, Roux H, Mattei JP (1999). "Surgical management of calcific tendinitis of the shoulder: an analysis of 26 cases". Clin. Rheumatol. 18 (4): 313–6. PMID 10468172.
- ↑ Louwerens JK, Sierevelt IN, van Noort A, van den Bekerom MP (August 2014). "Evidence for minimally invasive therapies in the management of chronic calcific tendinopathy of the rotator cuff: a systematic review and meta-analysis". J Shoulder Elbow Surg. 23 (8): 1240–9. doi:10.1016/j.jse.2014.02.002. PMID 24774621.