Brain herniation: Difference between revisions
Parul Pahal (talk | contribs) |
Parul Pahal (talk | contribs) |
||
| Line 32: | Line 32: | ||
{{familytree | | | | | | | | | B01 | | | | | | | | | | | B02 | | | | | | | | | | | |B01='''[[Supratentorial]] Herniation'''<br> occurs above<br> the tentorial notch|B02='''[[Infratentorial]] Herniation'''<br> occurs below<br> the tentorial notch}} | {{familytree | | | | | | | | | B01 | | | | | | | | | | | B02 | | | | | | | | | | | |B01='''[[Supratentorial]] Herniation'''<br> occurs above<br> the tentorial notch|B02='''[[Infratentorial]] Herniation'''<br> occurs below<br> the tentorial notch}} | ||
{{familytree | | | |,|-|-|-|v|-|^|-|v|-|-|-|.| | | |,|-|-|^|-|-|.|}} | {{familytree | | | |,|-|-|-|v|-|^|-|v|-|-|-|.| | | |,|-|-|^|-|-|.|}} | ||
{{familytree | | | D01 | | D02 | | D03 | | D04 | | | D05 | | D06 |D01=Uncal|D02=Central<br> or transtentorial|D03=Cingulate<br> or subfalcine<br> (most common type)|D04=Transcalvarial<br> | {{familytree | | | D01 | | D02 | | D03 | | D04 | | | D05 | | D06 |D01=Uncal|D02=Central<br> or transtentorial|D03=Cingulate<br> or subfalcine<br> (most common type)|D04=Transcalvarial<br> or<br> External herniation|D05=Upward<br> transtentorial<br> or<br> Upward<br> Cerebellar|D06=Tonsillar<br> or<br> Downward<br> Cerebellar}} | ||
{{familytree/end}} | {{familytree/end}} | ||
Latest revision as of 15:15, 20 August 2020
| Brain herniation | |
| ICD-10 | G93.5 |
|---|---|
| ICD-9 | 348.4 |
| MedlinePlus | 001421 |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Parul Pahal, M.B.B.S[2]
|
WikiDoc Resources for Brain herniation |
|
Articles |
|---|
|
Most recent articles on Brain herniation Most cited articles on Brain herniation |
|
Media |
|
Powerpoint slides on Brain herniation |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Brain herniation at Clinical Trials.gov Trial results on Brain herniation Clinical Trials on Brain herniation at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Brain herniation NICE Guidance on Brain herniation
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Brain herniation Discussion groups on Brain herniation Patient Handouts on Brain herniation Directions to Hospitals Treating Brain herniation Risk calculators and risk factors for Brain herniation
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Brain herniation |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
For patient information click here
Keywords and synonyms: Cerebral herniation, cerebellar herniation, uncal herniation, central herniation, supratentorial herniation, infratentorial herniation, transtentorial herniation, tonsillar herniation, cingulate herniation, transcalvarial herniation
Overview
Herniation, a deadly side effect of very high intracranial pressure, occurs when the brain shifts across structures within the skull. The brain can shift by such structures as the falx cerebri, the tentorium cerebelli, and even through the hole called the foramen magnum in the base of the skull (through which the spinal cord connects with the brain). Herniation can be caused by a number of factors that increase intracranial pressure such as traumatic brain injury. Because herniation puts extreme pressure on parts of the brain, it is often fatal. Therefore, extreme measures are taken in hospital settings to prevent the condition by reducing intracranial pressure.
Classification
There are two major classes of herniation: supratentorial and infratentorial.[1]. Depending on which structures of the brain have been displaced, herniation is further sub-classified.[2]
| Brain Herniation | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Supratentorial Herniation occurs above the tentorial notch | Infratentorial Herniation occurs below the tentorial notch | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Uncal | Central or transtentorial | Cingulate or subfalcine (most common type) | Transcalvarial or External herniation | Upward transtentorial or Upward Cerebellar | Tonsillar or Downward Cerebellar | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Central herniation
In central herniation, (also called "transtentorial herniation") the diencephalon and parts of the temporal lobes of both of the cerebral hemispheres are squeezed through a notch in the tentorium cerebelli.[2][3] Downward herniation can stretch branches of the basilar artery (paramedian artery), causing them to tear and bleed, known as a Duret hemorrhage. The result is usually fatal.[3]
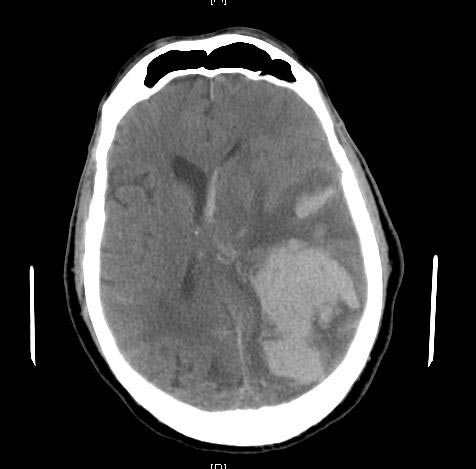
Uncal herniation
In uncal herniation, a common subtype of transtentorial herniation, the innermost part of the temporal lobe, the uncus, can be squeezed so much that it goes by the tentorium and puts pressure on the brainstem.[2] The tentorium is a structure within the skull formed by the meningeal layer the dura mater. Tissue may be stripped from the cerebral cortex in a process called decortication.[4] The uncus can squeeze the third cranial nerve, which controls parasympathetic input to the eye on the side of the affected nerve. This interrupts the parasympathetic neural transmission, causing the pupil of the affected eye to dilate and fail to constrict in response to light as it should, so a dilated unresponsive pupil is an important sign of increased intracranial pressure.[3] Pupillary dilation often precedes a later finding of cranial nerve III compression, which is deviation of the eye to a "down and out" position due to loss of innervation to all ocular motility muscles except for the lateral rectus (innervated by cranial nerve VI) and the superior oblique (innervated by cranial nerve IV). Cranial arteries may be compressed during the herniation. Compression of the posterior cerebral artery may result in loss of the contralateral visual field. A later important finding, the false localizing sign, results from compression of the contralateral cerebral crus, which contains descending corticospinal fibers. This leads to ipsilateral (to herniating uncus) hemiparesis of the body. This type of herniation can also damage the brain stem, causing lethargy, slow heart rate, respiratory abnormalities, and pupil dilation.[4] Uncal herniation may advance to central herniation.[1]
Cerebellar herniation
Increased pressure in the posterior fossa can cause the cerebellum to move up through the tentorial opening in upward, or cerebellar herniation.[2] The midbrain is pushed through the tentorial notch. This also pushes the midbrain down.
Tonsillar herniation
In tonsillar herniation, also called downward cerebellar herniation,[1] the cerebellar tonsils move downward through the foramen magnum possibly causing compression of the lower brainstem and upper cervical spinal cord as they pass through the foramen magnum.[2] Increased pressure on the brainstem can result in dysfunction of the centers in the brain responsible for controlling respiratory and cardiac function.
Tonsillar herniation of the cerebellum is also known commonly as a Chiari Malformation (CM) which previously was called an Arnold Chiari Malformation (ACM). There are at least three types of Chiari malformation that are widely recognized, and they represent very different disease processes with different symptoms and prognosis. These conditions can be found in asymptomatic patients, as an incidental finding, or can be so severe as to be life-threatening. This condition is now being diagnosed more frequently by radiologists as more and more patients undergo MRI scans of their heads. Cerebellar ectopia is a term used by radiologists to describe cerebellar tonsils that are "low lying" but that do not meet the radiographic criteria for definition as a Chiari malformation. The currently accepted radiographic definition for a Chiari malformation are cerebellar tonsils that lay at least 5mm below the level of the foramen magnum. Some clinicians have reported that some patients appear to experience symptoms consistent with a Chiari malformation without radiographic evidence of tonsillar herniation. Sometimes these patients are described as having a 'Chiari 0'.
There are many suspected causes of tonsillar herniation including (but not exclusively)- Spinal cord tethering or occult tight filum terminale (pulling down on the brainstem and surrounding structures); decreased or malformed posterior fossa (the lower, back part of the skull) not providing enough room for the cerebellum; hydrocephalus or abnormal CSF volume pushing the tonsils out; connective tissue disorders, such as Ehlers Danlos Syndrome, can be associated as well.(These may affect the ability of the brain, as well as the supporting joints, to maintain proper position/strength; in pediatric cases, ACM is often an 'incidental' finding while doing a work up for scoliosis, which is usually associated with certain connective tissue disorders).
For further evaluation of tonsillar herniation, CINE flow studies are suggested. This type of MRI will look at the flow of CSF at the cranio-cervical joint. For persons experiencing symptoms with seemingly minimal herniation, especially if the symptoms are better in the suppine position and worse upon standing/upright, an upright MRI may be useful.
Cingulate herniation
In cingulate or subfalcine herniation, the most common type, the innermost part of the frontal lobe is scraped under part of the falx cerebri, the dura mater at the top of the head between the two hemispheres of the brain.[2][5] Cingulate herniation can be caused when one hemisphere swells and pushes the cingulate gyrus by the falx cerebri.[1] This does not put as much pressure on the brainstem as the other types of herniation, but it may interfere with blood vessels in the frontal lobes that are close to the site of injury (anterior cerebral artery), or it may progress to central herniation.[2] Interference with the blood supply can cause dangerous increases in ICP that can lead to more dangerous forms of herniation.[6] Symptoms for cingulate herniation are not well defined.[6] Usually occurring in addition to uncal herniation, cingulate herniation may present with abnormal posturing and coma.[1] Cingulate herniation is frequently believed to be a precursor to other types of herniation.[6]
-
Subfalcine-herniation
Transcalvarial Herniation
In transcalvarial herniation, the brain squeezes through a fracture or a surgical site in the skull.[1]
Natural History, Complications and Prognosis
The patient may become paralyzed on the same side as the lesion causing the pressure, or damage to parts of the brain caused by herniation may cause paralysis on the side opposite the lesion.[3] Damage to the midbrain, which contains the reticular activating network that regulates consciousness will result in coma.[3] Damage to the cardio-respiratory centers in the medulla will cause respiratory and cardiac arrest.[3]
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 Orlando Regional Healthcare, Education and Development. 2004. "Overview of Adult Traumatic Brain Injuries." Retrieved on February 6, 2007
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 Shepherd S. 2004. "Head trauma." Emedicine.com. Retrieved on January 28, 2007.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 Cornell. 1998. Introduction to neuropathology. Reaction to injury: Brain histology." Cornell University Medical College.
- ↑ 4.0 4.1 McCaffrey P. 2001. "The neuroscience on the web series: CMSD 336 neuropathologies of language and cognition." California State University, Chico. Retrieved on August 7, 2007.
- ↑ Dawodu ST. 2007. Traumatic brain injury: Definition, epidemiology, pathophysiology. Emedicine.com. Retrieved on January 28, 2007.
- ↑ 6.0 6.1 6.2 Kristi Hudson. 2006. Brain Herniation Syndromes - 2 Nursing CEs. Dynamic Nursing Education. Retrieved on September 6, 2007.