Blalock-Taussig shunt: Difference between revisions
Sara Mohsin (talk | contribs) |
No edit summary |
||
| (17 intermediate revisions by 2 users not shown) | |||
| Line 8: | Line 8: | ||
==Overview== | ==Overview== | ||
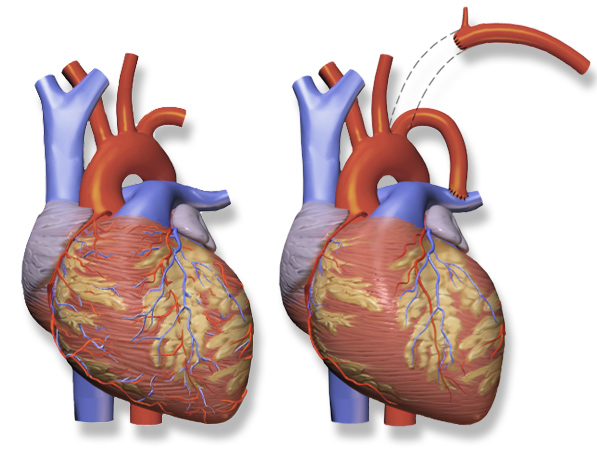
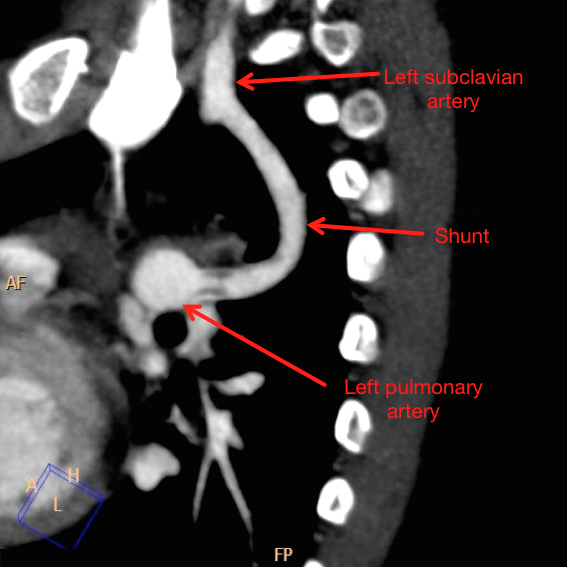
The '''Blalock-Taussig shunt''' is a [[Palliative treatment|palliative]] [[surgical procedure]] | The '''Blalock-Taussig shunt''' is a [[Palliative treatment|palliative]] [[surgical procedure]] for [[cyanotic heart defect]]s. This [[procedure]] is used to deviate [[blood flow]] to the [[lungs]] from [[systemic circulation]] to relieve [[cyanosis]] while a definitive [[corrective surgery]] can be performed at a later time. A connection is usually made between the [[subclavian artery]] and [[pulmonary artery]]. Usually, two types of [[Shunt (medical)|shunts]] are used: classic or original Blalock-Taussig shunt and modified Blalock Taussig shunt. The classic/original BT shunt has been modified into modified Blalock-Taussig Shunt (mBTS). In this modified [[procedure]], a [[graft]] from an [[innominate artery]] or [[subclavian artery]] is placed to the corresponding [[pulmonary artery]]. This type of BT shunt has superior [[Prognosis|prognostic]] value over the classical shunt leading to a greater rate of shunt patency in 3-5 years as compared to the classic or original BT Shunt. | ||
== Historical Perspective == | == Historical Perspective == | ||
| Line 49: | Line 49: | ||
*In 1962, it was first described and performed by Klinner et al. | *In 1962, it was first described and performed by Klinner et al. | ||
*It is | *It is more commonly used [[procedure]] and holds a better [[prognosis]] compared to the classic procedure. | ||
*An [[Interposition]] PTFE or Gore-Tex [[graft]] is placed between the [[subclavian artery]] and the [[pulmonary artery]]. | *An [[Interposition]] PTFE or Gore-Tex [[graft]] is placed between the [[subclavian artery]] and the [[pulmonary artery]]. As a result, there's no [[scarring]] of [[subclavian artery]].<ref name="pmid28701598">{{cite journal| author=Kiran U, Aggarwal S, Choudhary A, Uma B, Kapoor PM| title=The blalock and taussig shunt revisited. | journal=Ann Card Anaesth | year= 2017 | volume= 20 | issue= 3 | pages= 323-330 | pmid=28701598 | doi=10.4103/aca.ACA_80_17 | pmc=5535574 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28701598 }} </ref> | ||
{| class="wikitable" | {| class="wikitable" | ||
| Line 96: | Line 96: | ||
== Preparation for BT Shunt == | == Preparation for BT Shunt == | ||
*To perform a BT [[shunt]] following pre-operative preparation is done: | *To perform a BT [[shunt]] following pre-operative preparation is done: | ||
**[[Preoperative assessment|Preoperative]] psychological counseling of the patient | **[[Preoperative assessment|Preoperative]] [[psychological]] [[counseling]] of the [[patient]] | ||
**[[Preoperative assessment|Preoperative]] fasting | **[[Preoperative assessment|Preoperative]] fasting | ||
**[[Preoperative assessment|Preoperative]] [[Medication|medications]] | **[[Preoperative assessment|Preoperative]] [[Medication|medications]] | ||
*Anesthesia induction is based on the following patient and surgery-related factors: | *[[Anesthesia]] induction is based on the following [[patient]] and [[surgery]]-related factors: | ||
=== Patient-Related Factors === | === Patient-Related Factors === | ||
* Diagnosis of a relative [[Congenital Abnormalities|congenital]] cardiac anomaly | * [[Diagnosis]] of a relative [[Congenital Abnormalities|congenital]] [[cardiac]] [[anomaly]] | ||
* Age of the patient | * [[Age]] of the [[patient]] | ||
* Weight <3 kg leads to a high [[Mortality rate|mortality]] and [[morbidity]] | * [[Weight]] <3 kg leads to a high [[Mortality rate|mortality]] and [[morbidity]] | ||
*[[Premature birth|Premature infants]] | *[[Premature birth|Premature infants]] | ||
* Any non-cardiac coexisting congenital anomaly such as: | * Any non-[[cardiac]] coexisting [[congenital anomaly]] such as: | ||
**[[Tracheoesophageal fistula]] | **[[Tracheoesophageal fistula]] | ||
**[[Cleft lip and palate]] | **[[Cleft lip and palate]] | ||
**Renal anomalies | **[[Renal]] anomalies | ||
**Skeletal defects | **[[Skeletal]] defects | ||
*[[Atlanto-axial joint|Atlantoaxial instability]] or [[subluxation]] in [[Down syndrome]] should be considered while managing the airway. | *[[Atlanto-axial joint|Atlantoaxial instability]] or [[subluxation]] in [[Down syndrome]] should be considered while managing the [[airway]]. | ||
*[[Fatigue]], and/or [[dyspnea]] on feeding or any other factor showing exercise intolerance. | *[[Fatigue]], and/or [[dyspnea]] on feeding or any other factor showing [[exercise intolerance]]. | ||
* Use of medications that can lead to an increase in operative mortality such as: | * Use of [[medications]] that can lead to an increase in operative [[mortality]] such as: | ||
**[[Aspirin|Aspirin]] | **[[Aspirin|Aspirin]] | ||
**[[Warfarin]] | **[[Warfarin]] | ||
**[[Antidepressants|Anti-depressants]] | **[[Antidepressants|Anti-depressants]] | ||
**[[Diuretic|Diuretics]] | **[[Diuretic|Diuretics]] | ||
**[[Angiotensin converting enzyme ( | **[[Angiotensin converting enzyme inhibitors]] ([[ACEI]]) | ||
**[[Antiarrhythmics]] | **[[Antiarrhythmics]] | ||
* Congenital conditions such as [[subglottic stenosis]] that can lead to difficulty in gaining access for [[intubation]]. | * [[Congenital]] [[conditions]] such as [[subglottic stenosis]] that can lead to difficulty in gaining access for [[intubation]]. | ||
* Optimal right ventricular function | * Optimal [[right ventricular]] function | ||
=== Factors Related to Surgical Procedure === | === Factors Related to Surgical Procedure === | ||
* Complex lesions lead to high overall and in-hospital mortality. | * Complex [[lesions]] lead to high overall and in-hospital [[mortality]]. | ||
* Duration of the surgery | * Duration of the [[surgery]] | ||
* Cardiovascular anomalies that can lead to complexity of the procedure such as [[Aortic arch anomalies|aortic arch]] anomaly or presence of [[aberrant subclavian artery]]. | * [[Cardiovascular anomalies]] that can lead to complexity of the [[procedure]] such as [[Aortic arch anomalies|aortic arch]] [[anomaly]] or presence of [[aberrant subclavian artery]]. | ||
* Injury to the [[recurrent laryngeal nerve]] or [[phrenic nerve]] during the procedure. | * [[Injury]] to the [[recurrent laryngeal nerve]] or [[phrenic nerve]] during the [[procedure]]. | ||
* Nature and approach of the cardiac surgery e.g., [[cardiopulmonary bypass]], [[median sternotomy|sternotomy]] or [[thoracotomy]]. | * Nature and approach of the [[cardiac surgery]] e.g., [[cardiopulmonary bypass]], [[median sternotomy|sternotomy]] or [[thoracotomy]]. | ||
=== Approach === | === Approach === | ||
| Line 136: | Line 136: | ||
* Left lateral position is used for the right-sided modified Blalock-Taussig shunt (mBTS), and the right lateral position is used for left-sided mBTS. | * Left lateral position is used for the right-sided modified Blalock-Taussig shunt (mBTS), and the right lateral position is used for left-sided mBTS. | ||
* The approach used is usually [[thoracotomy]]. | * The approach used is usually [[thoracotomy]]. | ||
* [[Sternotomy]] is performed for the central shunts. | * [[Sternotomy]] is performed for the central [[shunts]]. | ||
== Complications == | == Complications == | ||
* The immediate [[Post operative complications|post-operative complications]] include:<ref name="pmid19040408">{{cite journal| author=Yuan SM, Shinfeld A, Raanani E| title=The Blalock-Taussig shunt. | journal=J Card Surg | year= 2009 | volume= 24 | issue= 2 | pages= 101-8 | pmid=19040408 | doi=10.1111/j.1540-8191.2008.00758.x | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19040408 }} </ref> | * The immediate [[Post operative complications|post-operative complications]] include:<ref name="pmid19040408">{{cite journal| author=Yuan SM, Shinfeld A, Raanani E| title=The Blalock-Taussig shunt. | journal=J Card Surg | year= 2009 | volume= 24 | issue= 2 | pages= 101-8 | pmid=19040408 | doi=10.1111/j.1540-8191.2008.00758.x | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19040408 }} </ref> | ||
** Development of [[chylothorax]], [[chylopericardium]] and [[Ascites|chylous ascites]] | ** Development of [[chylothorax]], [[chylopericardium]] and [[Ascites|chylous ascites]] | ||
**[[Phrenic nerve|Phrenic nerve resection]] leading to diaphragmatic paralysis | **[[Phrenic nerve|Phrenic nerve resection]] leading to [[diaphragmatic paralysis]] | ||
**[[Anemia]] | **[[Anemia]] | ||
**[[Congestive heart failure|Congestive heart failure]] resulting from excessive blood flow | **[[Congestive heart failure|Congestive heart failure]] resulting from excessive [[blood flow]] | ||
** Modified PTFE grafts can result in formation of [[seroma]] or shunt [[occlusion]] due to [[hyperplasia]] of [[neo-intima]] | ** Modified PTFE [[grafts]] can result in the formation of [[seroma]] or [[shunt]] [[occlusion]] due to [[hyperplasia]] of [[neo-intima]] | ||
**[[Stenosis]] of [[innominate artery]] | **[[Stenosis]] of [[innominate artery]] | ||
** | **[[Shunt]] [[infection]] resulting in [[sepsis]] | ||
[[File:Unilateral-pulmonary-oedema-blalock-taussig-shunt-in-pulmonary-atresia-with-ventricular-septal-defect-1.jpg|thumb|220px|none| Unilateral pulmonary edema, Blalock-Taussig shunt in pulmonary atresia with a ventricular septal defect. [https://radiopaedia.org/cases/18390 Source: Dr. Charlie Chia-Tsong.]]] | [[File:Unilateral-pulmonary-oedema-blalock-taussig-shunt-in-pulmonary-atresia-with-ventricular-septal-defect-1.jpg|thumb|220px|none| Unilateral pulmonary edema, Blalock-Taussig shunt in pulmonary atresia with a ventricular septal defect. [https://radiopaedia.org/cases/18390 Source: Dr. Charlie Chia-Tsong.]]] | ||
| Line 153: | Line 153: | ||
==== Shunt failure ==== | ==== Shunt failure ==== | ||
* Failure of the shunt is the most immediate risk during the post-operative period which can lead to a drop in [[oxygen saturation]] secondary due to [[Thrombosis|shunt thrombosis]] or [[kinking]]. | * [[Failure]] of the [[shunt]] is the most immediate risk during the post-operative period which can lead to a drop in [[oxygen saturation]] secondary due to [[Thrombosis|shunt thrombosis]] or [[kinking]]. | ||
* Shunt failure is a surgical emergency and should be managed as follows: | * [[Shunt]] [[failure]] is a [[surgical emergency]] and should be managed as follows: | ||
**[[Anticoagulant|Anticoagulation]] should be started promptly with [[heparin]]. It should be administered again if there is less risk of bleeding usually 4 hours post-op (when the drainage of the chest shows <3ml/kg/h and aPTT is <60s). [[Heparin-induced thrombocytopenia|Heparin induced thrombocytopenia]] can occur and should be managed accordingly. | **[[Anticoagulant|Anticoagulation]] should be started promptly with [[heparin]]. It should be administered again if there is less risk of [[bleeding]] usually 4 hours post-op (when the drainage of the [[chest]] shows <3ml/kg/h and aPTT is <60s). [[Heparin-induced thrombocytopenia|Heparin induced thrombocytopenia]] can occur and should be managed accordingly. | ||
** Patient is put on [[aspirin]] which is usually started at 3-5 mg/kg (max. dose 75mg) OD. | ** [[Patient]] is put on [[aspirin]] which is usually started at 3-5 mg/kg (max. dose 75mg) OD. | ||
**[[Heparin]] should be continued until there is a second dose of [[aspirin]]. | **[[Heparin]] should be continued until there is a second [[dose]] of [[aspirin]]. | ||
==== Blockage of BT shunt ==== | ==== Blockage of BT shunt ==== | ||
* Blockage or shunt [[thrombosis]] is another surgical emergency with a reported incidence of 12%. | * [[Blockage]] or [[shunt]] [[thrombosis]] is another [[surgical emergency]] with a reported [[incidence]] of 12%. | ||
* If there's any recent onset [[Murmurs|murmur]] or a significant drop in [[oxygen saturation]], it must be investigated. | * If there's any recent onset [[Murmurs|murmur]] or a significant drop in [[oxygen saturation]], it must be investigated. | ||
* Operative management is usually required and the shunt is usually repaired or replaced if necessary. | * Operative management is usually required and the [[shunt]] is usually repaired or replaced if necessary. | ||
=== High pulmonary blood flow === | === High pulmonary blood flow === | ||
* The appropriate size of BT shunt is very important to prevent the long term complications regarding high [[pulmonary]] blood flow or high oxygen saturation. | * The appropriate size of BT [[shunt]] is very important to prevent the long term [[complications]] regarding high [[pulmonary]] [[blood flow]] or high [[oxygen saturation]]. | ||
* [[Chest X-ray|Chest X Ray]] usually shows edematous lungs with low mixed venous saturation, rising [[lactate]] levels or signs of [[right heart failure]], [[Diastolic pressure|systemic diastolic pressure]] may be low, persistent [[metabolic acidosis]] leading to "pink patient" and [[Pulmonary hemorrhage|pulmonary hemorrhage | * [[Chest X-ray|Chest X Ray]] usually shows [[edematous]] [[lungs]] with low mixed [[venous saturation]], rising [[lactate]] levels or signs of [[right heart failure]], [[Diastolic pressure|systemic diastolic pressure]] may be low, persistent [[metabolic acidosis]] leading to "pink [[patient]]" and [[Pulmonary hemorrhage|pulmonary hemorrhage]]. | ||
===== Causes ===== | ===== Causes ===== | ||
*High [[FiO2]] | *High [[FiO2]] | ||
*[[PDA]] still open leading to excessive blood delivery to lungs | *[[PDA]] still open leading to excessive [[blood]] delivery to the [[lungs]] | ||
*Large shunt diameter | *Large [[shunt]] [[diameter]] | ||
===== Treatment ===== | ===== Treatment ===== | ||
Following treatment is instituted: | Following treatment is instituted: | ||
* For mild to moderate symptoms, fluid resuscitation and [[diuretics]] are given. Permissive [[hypercapnia]] and lowering of [[FiO2]] is done. | * For mild to moderate [[symptoms]], [[fluid resuscitation]] and [[diuretics]] are given. Permissive [[hypercapnia]] and lowering of [[FiO2]] is done. | ||
* For severe symptoms, [[systemic vascular resistance]] and [[pulmonary vascular resistance]] is adjusted. | * For severe [[symptoms]], [[systemic vascular resistance]] and [[pulmonary vascular resistance]] is adjusted. | ||
* Cases refractory to medical management are usually treated with a surgical approach that involves [[pulmonary artery]] banding or clamping. | * Cases refractory to [[medical]] management are usually treated with a [[surgical]] approach that involves [[pulmonary artery]] banding or clamping. | ||
== Prognosis == | == Prognosis == | ||
*Modified Blalock-Taussig | *Modified Blalock-Taussig shunt has a superior [[Prognosis|prognostic]] value over classic Blalock-Taussig Shunts. Following [[prognostic]] factors are compared between the two [[procedures]] in multiple studies:<ref name="pmid9855103">{{cite journal| author=Al Jubair KA, Al Fagih MR, Al Jarallah AS, Al Yousef S, Ali Khan MA, Ashmeg A | display-authors=etal| title=Results of 546 Blalock-Taussig shunts performed in 478 patients. | journal=Cardiol Young | year= 1998 | volume= 8 | issue= 4 | pages= 486-90 | pmid=9855103 | doi=10.1017/s1047951100007150 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=9855103 }} </ref><ref name="pmid16337132">{{cite journal| author=Kim HK, Kim WH, Kim SC, Lim C, Lee CH, Kim SJ| title=Surgical strategy for pulmonary coarctation in the univentricular heart. | journal=Eur J Cardiothorac Surg | year= 2006 | volume= 29 | issue= 1 | pages= 100-4 | pmid=16337132 | doi=10.1016/j.ejcts.2005.10.032 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16337132 }} </ref><ref name="pmid3968910">{{cite journal| author=Karpawich PP, Bush CP, Antillon JR, Amato JJ, Marbey ML, Agarwal KC| title=Modified Blalock-Taussig shunt in infants and young children. Clinical and catheterization assessment. | journal=J Thorac Cardiovasc Surg | year= 1985 | volume= 89 | issue= 2 | pages= 275-9 | pmid=3968910 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=3968910 }} </ref><ref name="pmid10707705">{{cite journal| author=Kulkarni H, Rajani R, Dalvi B, Gupta KG, Vora A, Kelkar P| title=Effect of Blalock Taussig shunt on clinical parameters, left ventricular function and pulmonary arteries. | journal=J Postgrad Med | year= 1995 | volume= 41 | issue= 2 | pages= 34-6 | pmid=10707705 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=10707705 }} </ref><ref name="pmid2441893">{{cite journal| author=Bove EL, Kohman L, Sereika S, Byrum CJ, Kavey RE, Blackman MS | display-authors=etal| title=The modified Blalock-Taussig shunt: analysis of adequacy and duration of palliation. | journal=Circulation | year= 1987 | volume= 76 | issue= 3 Pt 2 | pages= III19-23 | pmid=2441893 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=2441893 }} </ref><ref name="pmid3675059">{{cite journal| author=Ullom RL, Sade RM, Crawford FA, Ross BA, Spinale F| title=The Blalock-Taussig shunt in infants: standard versus modified. | journal=Ann Thorac Surg | year= 1987 | volume= 44 | issue= 5 | pages= 539-43 | pmid=3675059 | doi=10.1016/s0003-4975(10)62119-4 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=3675059 }} </ref> | ||
** The increase in [[Oxygen saturation|saturation of oxygen]] is greater in the modified shunt as compared to the classic shunt. | ** The increase in [[Oxygen saturation|saturation of oxygen]] is greater in the modified [[shunt]] as compared to the classic [[shunt]]. | ||
** Modified shunt has an 88.8% patency rate in 3-5 years. Whereas for the classic shunt, the patency rate is 90% in the first year, 62% in two years, and 78.0% in 3 years. | ** Modified [[shunt]] has an 88.8% patency rate in 3-5 years. Whereas for the classic [[shunt]], the patency rate is 90% in the first year, 62% in two years, and 78.0% in 3 years. | ||
** The risk of early shunt failure is 20.8% in modified and 51.7% in the classic shunt. | ** The risk of early [[shunt]] [[failure]] is 20.8% in modified and 51.7% in the classic [[shunt]]. | ||
** Post-shunt increase in [[Pulmonary artery|pulmonary arterial index]] (mm2/m2) is 158 +/- 21 versus 117 +/- 52 in classic Blalock-Taussig shunt. | ** Post-shunt increase in [[Pulmonary artery|pulmonary arterial index]] (mm2/m2) is 158 +/- 21 versus 117 +/- 52 in classic Blalock-Taussig shunt. | ||
| Line 195: | Line 195: | ||
=== Central Shunt === | === Central Shunt === | ||
* Central shunt is made by creating an [[anastomosis]] between [[ascending aorta]] and main [[Pulmonary artery|pulmonary artery]]. | * Central [[shunt]] is made by creating an [[anastomosis]] between [[ascending aorta]] and main [[Pulmonary artery|pulmonary artery]]. | ||
* A short PTFE conduit for this purpose is used. | * A short PTFE conduit for this purpose is used. | ||
* It is also known as Mee's shunt. <ref name="Eghtesady 2015 pp. 293–305">{{cite journal | last=Eghtesady | first=Pirooz | title=Potts Shunt for Children With Severe Pulmonary Hypertension | journal=Operative Techniques in Thoracic and Cardiovascular Surgery | publisher=Elsevier BV | volume=20 | issue=3 | year=2015 | issn=1522-2942 | doi=10.1053/j.optechstcvs.2016.02.003 | pages=293–305}}</ref> | * It is also known as Mee's [[shunt]]. <ref name="Eghtesady 2015 pp. 293–305">{{cite journal | last=Eghtesady | first=Pirooz | title=Potts Shunt for Children With Severe Pulmonary Hypertension | journal=Operative Techniques in Thoracic and Cardiovascular Surgery | publisher=Elsevier BV | volume=20 | issue=3 | year=2015 | issn=1522-2942 | doi=10.1053/j.optechstcvs.2016.02.003 | pages=293–305}}</ref> | ||
* [[Internal mammary artery]] is used for this purpose and to create a systemic to pulmonary conduit after there has been a failure of previously used BT shunt. | * [[Internal mammary artery]] is used for this purpose and to create a [[systemic]] to [[pulmonary]] conduit after there has been a [[failure]] of previously used BT [[shunt]]. | ||
* It leads to adaptation of growth, and flow, and it also reduces the risk for graft infection. | * It leads to adaptation of [[growth]], and flow, and it also reduces the risk for [[graft]] [[infection]]. | ||
{| class="wikitable" | {| class="wikitable" | ||
|+ | |+ | ||
| Line 205: | Line 205: | ||
! style="background: #4479BA; width: 200px;" |{{fontcolor|#FFF|Disadvantages}} | ! style="background: #4479BA; width: 200px;" |{{fontcolor|#FFF|Disadvantages}} | ||
|- | |- | ||
|Can be done in small children with small vessels | |Can be done in small [[children]] with small [[vessels]] | ||
|Can not be performed in patients without [[patent ductus arteriosus]] | |Can not be performed in [[patients]] without [[patent ductus arteriosus]] | ||
|- | |- | ||
|Distortion of [[pulmonary vessels]] is avoided | |Distortion of [[pulmonary vessels]] is avoided | ||
|Entry into [[pericardium]] | |Entry into [[pericardium]] | ||
|- | |- | ||
|Equal blood flow is provided to both lungs | |Equal [[blood flow]] is provided to both [[lungs]] | ||
| | | | ||
|- | |- | ||
| Line 222: | Line 222: | ||
=== Potts shunt === | === Potts shunt === | ||
* Potts shunt can be used as an alternative to the classic BT shunt. | * Potts [[shunt]] can be used as an alternative to the classic BT [[shunt]]. | ||
* To avoid the consequences of [[right heart failure]], it has been used as an alternative to offload the right ventricle. | * To avoid the consequences of [[right heart failure]], it has been used as an alternative to offload the [[right ventricle]]. | ||
* This improves the cardiac output but the oxygen saturation is lowered and there is decreased oxygen delivery to lower extremities. | * This improves the [[cardiac output]] but the [[oxygen saturation]] is lowered and there is decreased [[oxygen]] delivery to lower [[extremities]]. | ||
* Potts shunt includes a connection that is made between [[descending aorta]] and [[left pulmonary artery]].<ref name="Yuan Jing 2009 pp. 549–557">{{cite journal | last=Yuan | first=Shi-Min | last2=Jing | first2=Hua | title=Palliative procedures for congenital heart defects | journal=Archives of Cardiovascular Diseases | publisher=Elsevier BV | volume=102 | issue=6-7 | year=2009 | issn=1875-2136 | doi=10.1016/j.acvd.2009.04.011 | pages=549–557}}</ref> | * Potts [[shunt]] includes a connection that is made between [[descending aorta]] and [[left pulmonary artery]].<ref name="Yuan Jing 2009 pp. 549–557">{{cite journal | last=Yuan | first=Shi-Min | last2=Jing | first2=Hua | title=Palliative procedures for congenital heart defects | journal=Archives of Cardiovascular Diseases | publisher=Elsevier BV | volume=102 | issue=6-7 | year=2009 | issn=1875-2136 | doi=10.1016/j.acvd.2009.04.011 | pages=549–557}}</ref> | ||
{| class="wikitable" | {| class="wikitable" | ||
| Line 232: | Line 232: | ||
! style="background: #4479BA; width: 200px;" |{{fontcolor|#FFF|Disadvantages}} | ! style="background: #4479BA; width: 200px;" |{{fontcolor|#FFF|Disadvantages}} | ||
|- | |- | ||
|[[Subclavian artery]] is used which has a large diameter hence, it is easy to perform surgery. | |[[Subclavian artery]] is used which has a large [[diameter]] hence, it is easy to perform [[surgery]]. | ||
|Increased incidence of [[pulmonary hypertension]] | |Increased [[incidence]] of [[pulmonary hypertension]] | ||
|- | |- | ||
|Lower chance of occlusion than CBTS and mBTS | |Lower chance of occlusion than CBTS and mBTS | ||
|Increased blood flow to one lung while there is kinking of pulmonary artery | |Increased [[blood flow]] to one [[lung]] while there is kinking of [[pulmonary artery]] | ||
|- | |- | ||
| | | | ||
| Line 244: | Line 244: | ||
=== '''Waterston shunt''' === | === '''Waterston shunt''' === | ||
* It is made by connecting the [[ascending aorta]] and [[right pulmonary artery]]. | * It is made by connecting the [[ascending aorta]] and [[right pulmonary artery]]. | ||
* It has not been clinically performed now due to increased risk of [[congestive heart failure]], [[pulmonary hypertension]], and kinking of the pulmonary artery. | * It has not been clinically performed now due to increased risk of [[congestive heart failure]], [[pulmonary hypertension]], and kinking of the [[pulmonary artery]]. | ||
=== Cooley Shunt === | === Cooley Shunt === | ||
* It is an [[Anastomosis|intrapericardial anastomosis]] between ascending aorta and the right pulmonary artery. | * It is an [[Anastomosis|intrapericardial anastomosis]] between [[ascending aorta]] and the right [[pulmonary artery]]. | ||
* Right anterolateral [[thoracotomy]] approach is used. | * Right anterolateral [[thoracotomy]] approach is used. | ||
{| class="wikitable" | {| class="wikitable" | ||
| Line 255: | Line 255: | ||
! style="background: #4479BA; width: 200px;" |{{fontcolor|#FFF|Disadvantages}} | ! style="background: #4479BA; width: 200px;" |{{fontcolor|#FFF|Disadvantages}} | ||
|- | |- | ||
|Use of right anterolateral incision for all approaches - [[Mediastinal|Mediastinal dissection]] is avoided | |Use of right anterolateral [[incision]] for all approaches - [[Mediastinal|Mediastinal dissection]] is avoided | ||
|Improper size of shunt can lead to [[right heart failure]] and [[pulmonary congestion]] | |Improper size of the [[shunt]] can lead to [[right heart failure]] and [[pulmonary congestion]] | ||
|- | |- | ||
|Total repair can be done after this shunt in future | |Total repair can be done after this [[shunt]] in future | ||
|Risk of intracardiac adhesions | |Risk of [[intracardiac]] [[adhesions]] | ||
|- | |- | ||
| | | | ||
|Complexity of the procedure | |Complexity of the [[procedure]] | ||
|} | |} | ||
==References== | ==References== | ||
{{Reflist|2}} | {{Reflist|2}} | ||
[[Category:Up-To-Date]] | |||
[[Category:Cardiology]] | [[Category:Cardiology]] | ||
[[Category:Surgery]] | [[Category:Surgery]] | ||
Latest revision as of 13:45, 20 October 2020
|
Blalock-Taussig shunt Microchapters |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor-In-Chief: Usman Ali Akbar, M.B.B.S.[2]
Synonyms and keywords: Blalock Taussig Procedure, Procedure, Blalock-Taussig, Subclavian Pulmonary Artery Shunt, Blue Baby Operations, Modified Blalock-Taussig Procedure
Overview
The Blalock-Taussig shunt is a palliative surgical procedure for cyanotic heart defects. This procedure is used to deviate blood flow to the lungs from systemic circulation to relieve cyanosis while a definitive corrective surgery can be performed at a later time. A connection is usually made between the subclavian artery and pulmonary artery. Usually, two types of shunts are used: classic or original Blalock-Taussig shunt and modified Blalock Taussig shunt. The classic/original BT shunt has been modified into modified Blalock-Taussig Shunt (mBTS). In this modified procedure, a graft from an innominate artery or subclavian artery is placed to the corresponding pulmonary artery. This type of BT shunt has superior prognostic value over the classical shunt leading to a greater rate of shunt patency in 3-5 years as compared to the classic or original BT Shunt.
Historical Perspective
Classic or Original Shunt
- The classic or original BT shunt procedure was named after a surgeon in Baltimore, Alfred Blalock (1899–1964), and a cardiologist in Baltimore/Boston, Helen B. Taussig (1898–1986), who along with Blalock's African American laboratory technician Vivien Thomas (1910–1985), developed and described the procedure.
- Taussig noticed that the children with cyanosis along with congenital heart disease accompanied by patent ductus arteriosus have a longer lifetime than those without PDA.
- In 1943, Dr. Taussig approached Blalock and Thomas in their Hopkins laboratory to work on this shunt as it was hypothesized that a shunt mimicking PDA can relieve the cyanosis and improve oxygenation in congential cyanotic diseases.[1]
Modified Blalock-Taussig Shunt
- In 1962, a modified method of inserting a shunt was developed by Klinner using teflon as a prosthetic graft material between the subclavian artery and the pulmonary artery in order to prevent scarring of the subclavian artery.[2][3][4]

Classification
Classic/Original Blalock-Taussig Shunt
- For classic Blalock-Taussig shunt, an end-to-end anastomosis opposite to the aortic arch is performed between the subclavian and pulmonary arteries to minimize the kinking of subclavian artery as it crosses aortic prominence.[4]
| Advantages | Disadvantages |
|---|---|
| The relative diameter of subclavian artery prevents excessive blood flow to lungs | Thrombosis of shunt due to less diameter |
| Easily reversible | Risk of dissection |
| Increased rate of anastomosis growth | Subclavian artery is lost during the procedure |
Modified Blalock Taussig Shunt
- In 1962, it was first described and performed by Klinner et al.
- It is more commonly used procedure and holds a better prognosis compared to the classic procedure.
- An Interposition PTFE or Gore-Tex graft is placed between the subclavian artery and the pulmonary artery. As a result, there's no scarring of subclavian artery.[4]
| Advantages | Disadvantages |
|---|---|
| It can be done on the same side of the aortic arch | Thrombosis |
| More patency than Classic BT shunt i.e >90 % at 2 years | Pseudoaneurysm |
| Pulmonary artery is less distorted | Chylothorax, Chylopericardium, chylous ascites |
Goals of BT shunt
- The ultimate endpoint goals of BT shunt are as follows:
- To stabilize the preload, hence preventing hemodilution.
- To maintain the systemic vascular resistance (afterload) hence, adequate diastolic pressure to maintain coronary perfusion.
- Increase the blood flow to the pulmonary vasculature in a supervised manner.
Indications
- Following is a list of indications for Blalock-Taussig shunt:
- Tricuspid atresia
- Tetralogy of Fallot
- Ebstein's Anomaly
- Hypoplastic Left Heart syndrome
- Pulmonary atresia
- Inadequate pulmonary arteries
Risk Factors
- Following multiple risk factors have been identified to be associated with high morbidity and mortality in neonates:[5][6]
- Sternal approach for MBTS construction
- Univentricular heart
- Complicated surgery (CABG)
- Weight <3 kg
- Pre-operative ventilation support
- Pre-operative acidosis and shock
- Use of Innominate artery-PA shunt
- Diagnosis of Ebstein's Anomaly
Preparation for BT Shunt
- To perform a BT shunt following pre-operative preparation is done:
- Preoperative psychological counseling of the patient
- Preoperative fasting
- Preoperative medications
- Anesthesia induction is based on the following patient and surgery-related factors:
Patient-Related Factors
- Diagnosis of a relative congenital cardiac anomaly
- Age of the patient
- Weight <3 kg leads to a high mortality and morbidity
- Premature infants
- Any non-cardiac coexisting congenital anomaly such as:
- Tracheoesophageal fistula
- Cleft lip and palate
- Renal anomalies
- Skeletal defects
- Atlantoaxial instability or subluxation in Down syndrome should be considered while managing the airway.
- Fatigue, and/or dyspnea on feeding or any other factor showing exercise intolerance.
- Use of medications that can lead to an increase in operative mortality such as:
- Congenital conditions such as subglottic stenosis that can lead to difficulty in gaining access for intubation.
- Optimal right ventricular function
Factors Related to Surgical Procedure
- Complex lesions lead to high overall and in-hospital mortality.
- Duration of the surgery
- Cardiovascular anomalies that can lead to complexity of the procedure such as aortic arch anomaly or presence of aberrant subclavian artery.
- Injury to the recurrent laryngeal nerve or phrenic nerve during the procedure.
- Nature and approach of the cardiac surgery e.g., cardiopulmonary bypass, sternotomy or thoracotomy.
Approach
- Left lateral position is used for the right-sided modified Blalock-Taussig shunt (mBTS), and the right lateral position is used for left-sided mBTS.
- The approach used is usually thoracotomy.
- Sternotomy is performed for the central shunts.
Complications
- The immediate post-operative complications include:[3]
- Development of chylothorax, chylopericardium and chylous ascites
- Phrenic nerve resection leading to diaphragmatic paralysis
- Anemia
- Congestive heart failure resulting from excessive blood flow
- Modified PTFE grafts can result in the formation of seroma or shunt occlusion due to hyperplasia of neo-intima
- Stenosis of innominate artery
- Shunt infection resulting in sepsis

Management of Complications
Shunt failure
- Failure of the shunt is the most immediate risk during the post-operative period which can lead to a drop in oxygen saturation secondary due to shunt thrombosis or kinking.
- Shunt failure is a surgical emergency and should be managed as follows:
- Anticoagulation should be started promptly with heparin. It should be administered again if there is less risk of bleeding usually 4 hours post-op (when the drainage of the chest shows <3ml/kg/h and aPTT is <60s). Heparin induced thrombocytopenia can occur and should be managed accordingly.
- Patient is put on aspirin which is usually started at 3-5 mg/kg (max. dose 75mg) OD.
- Heparin should be continued until there is a second dose of aspirin.
Blockage of BT shunt
- Blockage or shunt thrombosis is another surgical emergency with a reported incidence of 12%.
- If there's any recent onset murmur or a significant drop in oxygen saturation, it must be investigated.
- Operative management is usually required and the shunt is usually repaired or replaced if necessary.
High pulmonary blood flow
- The appropriate size of BT shunt is very important to prevent the long term complications regarding high pulmonary blood flow or high oxygen saturation.
- Chest X Ray usually shows edematous lungs with low mixed venous saturation, rising lactate levels or signs of right heart failure, systemic diastolic pressure may be low, persistent metabolic acidosis leading to "pink patient" and pulmonary hemorrhage.
Causes
Treatment
Following treatment is instituted:
- For mild to moderate symptoms, fluid resuscitation and diuretics are given. Permissive hypercapnia and lowering of FiO2 is done.
- For severe symptoms, systemic vascular resistance and pulmonary vascular resistance is adjusted.
- Cases refractory to medical management are usually treated with a surgical approach that involves pulmonary artery banding or clamping.
Prognosis
- Modified Blalock-Taussig shunt has a superior prognostic value over classic Blalock-Taussig Shunts. Following prognostic factors are compared between the two procedures in multiple studies:[7][8][9][10][11][12]
- The increase in saturation of oxygen is greater in the modified shunt as compared to the classic shunt.
- Modified shunt has an 88.8% patency rate in 3-5 years. Whereas for the classic shunt, the patency rate is 90% in the first year, 62% in two years, and 78.0% in 3 years.
- The risk of early shunt failure is 20.8% in modified and 51.7% in the classic shunt.
- Post-shunt increase in pulmonary arterial index (mm2/m2) is 158 +/- 21 versus 117 +/- 52 in classic Blalock-Taussig shunt.
Alternative Shunts
Central Shunt
- Central shunt is made by creating an anastomosis between ascending aorta and main pulmonary artery.
- A short PTFE conduit for this purpose is used.
- It is also known as Mee's shunt. [13]
- Internal mammary artery is used for this purpose and to create a systemic to pulmonary conduit after there has been a failure of previously used BT shunt.
- It leads to adaptation of growth, and flow, and it also reduces the risk for graft infection.
| Advantages | Disadvantages |
|---|---|
| Can be done in small children with small vessels | Can not be performed in patients without patent ductus arteriosus |
| Distortion of pulmonary vessels is avoided | Entry into pericardium |
| Equal blood flow is provided to both lungs | |
| Low chance of occlusion rate | |
| Subclavian steal syndrome is usually avoided |
Potts shunt
- Potts shunt can be used as an alternative to the classic BT shunt.
- To avoid the consequences of right heart failure, it has been used as an alternative to offload the right ventricle.
- This improves the cardiac output but the oxygen saturation is lowered and there is decreased oxygen delivery to lower extremities.
- Potts shunt includes a connection that is made between descending aorta and left pulmonary artery.[14]
| Advantages | Disadvantages |
|---|---|
| Subclavian artery is used which has a large diameter hence, it is easy to perform surgery. | Increased incidence of pulmonary hypertension |
| Lower chance of occlusion than CBTS and mBTS | Increased blood flow to one lung while there is kinking of pulmonary artery |
| Increased risk of congestive heart failure [15] |
Waterston shunt
- It is made by connecting the ascending aorta and right pulmonary artery.
- It has not been clinically performed now due to increased risk of congestive heart failure, pulmonary hypertension, and kinking of the pulmonary artery.
Cooley Shunt
- It is an intrapericardial anastomosis between ascending aorta and the right pulmonary artery.
- Right anterolateral thoracotomy approach is used.
| Advantages | Disadvantages |
|---|---|
| Use of right anterolateral incision for all approaches - Mediastinal dissection is avoided | Improper size of the shunt can lead to right heart failure and pulmonary congestion |
| Total repair can be done after this shunt in future | Risk of intracardiac adhesions |
| Complexity of the procedure |
References
- ↑ https://www.upenn.edu/pennpress/book/1904.html
- ↑ KLINNER W, PASINI M, SCHAUDIG A (1962). "[Anastomosis between systemic and pulmonary arteries with the aid of plastic prostheses in cyanotic heart diseases]". Thoraxchirurgie. 10: 68–75. doi:10.1055/s-0028-1096482. PMID 14457041.
- ↑ 3.0 3.1 Yuan SM, Shinfeld A, Raanani E (2009). "The Blalock-Taussig shunt". J Card Surg. 24 (2): 101–8. doi:10.1111/j.1540-8191.2008.00758.x. PMID 19040408.
- ↑ 4.0 4.1 4.2 Kiran U, Aggarwal S, Choudhary A, Uma B, Kapoor PM (2017). "The blalock and taussig shunt revisited". Ann Card Anaesth. 20 (3): 323–330. doi:10.4103/aca.ACA_80_17. PMC 5535574. PMID 28701598.
- ↑ Schmoldt A, Benthe HF, Haberland G (1975). "Digitoxin metabolism by rat liver microsomes". Biochem Pharmacol. 24 (17): 1639–41. PMID https://doi.org/10.1016/j.jamcollsurg.2012.12.027 Check
|pmid=value (help). - ↑ Schmoldt A, Benthe HF, Haberland G (1975). "Digitoxin metabolism by rat liver microsomes". Biochem Pharmacol. 24 (17): 1639–41. PMID https://doi.org/10.1016/j.athoracsur.2011.02.030 Check
|pmid=value (help). - ↑ Al Jubair KA, Al Fagih MR, Al Jarallah AS, Al Yousef S, Ali Khan MA, Ashmeg A; et al. (1998). "Results of 546 Blalock-Taussig shunts performed in 478 patients". Cardiol Young. 8 (4): 486–90. doi:10.1017/s1047951100007150. PMID 9855103.
- ↑ Kim HK, Kim WH, Kim SC, Lim C, Lee CH, Kim SJ (2006). "Surgical strategy for pulmonary coarctation in the univentricular heart". Eur J Cardiothorac Surg. 29 (1): 100–4. doi:10.1016/j.ejcts.2005.10.032. PMID 16337132.
- ↑ Karpawich PP, Bush CP, Antillon JR, Amato JJ, Marbey ML, Agarwal KC (1985). "Modified Blalock-Taussig shunt in infants and young children. Clinical and catheterization assessment". J Thorac Cardiovasc Surg. 89 (2): 275–9. PMID 3968910.
- ↑ Kulkarni H, Rajani R, Dalvi B, Gupta KG, Vora A, Kelkar P (1995). "Effect of Blalock Taussig shunt on clinical parameters, left ventricular function and pulmonary arteries". J Postgrad Med. 41 (2): 34–6. PMID 10707705.
- ↑ Bove EL, Kohman L, Sereika S, Byrum CJ, Kavey RE, Blackman MS; et al. (1987). "The modified Blalock-Taussig shunt: analysis of adequacy and duration of palliation". Circulation. 76 (3 Pt 2): III19–23. PMID 2441893.
- ↑ Ullom RL, Sade RM, Crawford FA, Ross BA, Spinale F (1987). "The Blalock-Taussig shunt in infants: standard versus modified". Ann Thorac Surg. 44 (5): 539–43. doi:10.1016/s0003-4975(10)62119-4. PMID 3675059.
- ↑ Eghtesady, Pirooz (2015). "Potts Shunt for Children With Severe Pulmonary Hypertension". Operative Techniques in Thoracic and Cardiovascular Surgery. Elsevier BV. 20 (3): 293–305. doi:10.1053/j.optechstcvs.2016.02.003. ISSN 1522-2942.
- ↑ Yuan, Shi-Min; Jing, Hua (2009). "Palliative procedures for congenital heart defects". Archives of Cardiovascular Diseases. Elsevier BV. 102 (6–7): 549–557. doi:10.1016/j.acvd.2009.04.011. ISSN 1875-2136.
- ↑ TRUCCONE, NESTOR J.; BOWMAN, FREDERICK O.; MALM, JAMES R.; GERSONY, WELTON M. (1974). "Systemic-Pulmonary Arterial Shunts in the First Year of Life". Circulation. Ovid Technologies (Wolters Kluwer Health). 49 (3): 508–511. doi:10.1161/01.cir.49.3.508. ISSN 0009-7322.