Bisoprolol
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Alonso Alvarado, M.D. [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
Bisoprolol is a beta-adrenergic blocker that is FDA approved for the treatment of hypertension. Common adverse reactions include diarrhea, headache, rhinitis, upper respiratory infection, fatigue.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Condition 1
- Dosing Information
- (Dosage)
Condition 2
- Dosing Information
- (Dosage)
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
Condition 1
- Developed by: (Organisation)
- Class of Recommendation: (Class) (Link)
- Strength of Evidence: (Category A/B/C) (Link)
- Dosing Information/Recommendation
- (Dosage)
Condition 2
- Developed by: (Organisation)
- Class of Recommendation: (Class) (Link)
- Strength of Evidence: (Category A/B/C) (Link)
- Dosing Information/Recommendation
- (Dosage)
Non–Guideline-Supported Use
Condition 1
- Dosing Information
- (Dosage)
Condition 2
- Dosing Information
- (Dosage)
Condition 3
- Dosing Information
- (Dosage)
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
Condition 1
- Dosing Information
- (Dosage)
Condition 2
- Dosing Information
- (Dosage)
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
Condition 1
- Developed by: (Organisation)
- Class of Recommendation: (Class) (Link)
- Strength of Evidence: (Category A/B/C) (Link)
- Dosing Information/Recommendation
- (Dosage)
Condition 2
- Developed by: (Organisation)
- Class of Recommendation: (Class) (Link)
- Strength of Evidence: (Category A/B/C) (Link)
- Dosing Information/Recommendation
- (Dosage)
Non–Guideline-Supported Use
Condition 1
- Dosing Information
- (Dosage)
Condition 2
- Dosing Information
- (Dosage)
Condition 3
- Dosing Information
- (Dosage)
Contraindications
- Cardiogenic shock
- Overt cardiac failure
- Second degree AV block
- Third degree AV block
- Marked sinus bradycardia
Warnings
Conidition 1
(Description)
Adverse Reactions
Clinical Trials Experience
Central Nervous System
- (list/description of adverse reactions)
Cardiovascular
- (list/description of adverse reactions)
Respiratory
- (list/description of adverse reactions)
Gastrointestinal
- (list/description of adverse reactions)
Hypersensitive Reactions
- (list/description of adverse reactions)
Miscellaneous
- (list/description of adverse reactions)
Condition 2
Central Nervous System
- (list/description of adverse reactions)
Cardiovascular
- (list/description of adverse reactions)
Respiratory
- (list/description of adverse reactions)
Gastrointestinal
- (list/description of adverse reactions)
Hypersensitive Reactions
- (list/description of adverse reactions)
Miscellaneous
- (list/description of adverse reactions)
Postmarketing Experience
(Description)
Drug Interactions
- Drug 1
- Drug 2
- Drug 3
- Drug 4
- Drug 5
Drug 1
(Description)
Drug 2
(Description)
Drug 3
(Description)
Drug 4
(Description)
Drug 5
(Description)
Use in Specific Populations
Pregnancy
Pregnancy Category (FDA):
(Description)
Pregnancy Category (AUS):
(Description)
Labor and Delivery
(Description)
Nursing Mothers
(Description)
Pediatric Use
(Description)
Geriatic Use
(Description)
Gender
(Description)
Race
(Description)
Renal Impairment
(Description)
Hepatic Impairment
(Description)
Females of Reproductive Potential and Males
(Description)
Immunocompromised Patients
(Description)
Others
(Description)
Administration and Monitoring
Administration
(Oral/Intravenous/etc)
Monitoring
Condition 1
(Description regarding monitoring, from Warnings section)
Condition 2
(Description regarding monitoring, from Warnings section)
Condition 3
(Description regarding monitoring, from Warnings section)
IV Compatibility
Solution
Compatible
- Solution 1
- Solution 2
- Solution 3
Not Tested
- Solution 1
- Solution 2
- Solution 3
Variable
- Solution 1
- Solution 2
- Solution 3
Incompatible
- Solution 1
- Solution 2
- Solution 3
Y-Site
Compatible
- Solution 1
- Solution 2
- Solution 3
Not Tested
- Solution 1
- Solution 2
- Solution 3
Variable
- Solution 1
- Solution 2
- Solution 3
Incompatible
- Solution 1
- Solution 2
- Solution 3
Admixture
Compatible
- Solution 1
- Solution 2
- Solution 3
Not Tested
- Solution 1
- Solution 2
- Solution 3
Variable
- Solution 1
- Solution 2
- Solution 3
Incompatible
- Solution 1
- Solution 2
- Solution 3
Syringe
Compatible
- Solution 1
- Solution 2
- Solution 3
Not Tested
- Solution 1
- Solution 2
- Solution 3
Variable
- Solution 1
- Solution 2
- Solution 3
Incompatible
- Solution 1
- Solution 2
- Solution 3
TPN/TNA
Compatible
- Solution 1
- Solution 2
- Solution 3
Not Tested
- Solution 1
- Solution 2
- Solution 3
Variable
- Solution 1
- Solution 2
- Solution 3
Incompatible
- Solution 1
- Solution 2
- Solution 3
Overdosage
Acute Overdose
Signs and Symptoms
(Description)
Management
(Description)
Chronic Overdose
Signs and Symptoms
(Description)
Management
(Description)
Pharmacology
| |
1 : 1 mixture (racemate)Bisoprolol
| |
| Systematic (IUPAC) name | |
| (RS)-1-{4-[(2-isopropoxyethoxy)methyl]phenoxy}- 3-(isopropylamino)propan-2-ol | |
| Identifiers | |
| CAS number | |
| ATC code | C07 |
| PubChem | |
| DrugBank | |
| Chemical data | |
| Formula | Template:OrganicBox atomTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox |
| Mol. mass | 325.443 g/mol |
| SMILES | & |
| Pharmacokinetic data | |
| Bioavailability | >90% |
| Protein binding | 30%[1] |
| Metabolism | 50% Hepatic |
| Half life | 10–12 hours[2] |
| Excretion | ? |
| Therapeutic considerations | |
| Licence data |
|
| Pregnancy cat. | |
| Legal status |
Template:Unicode Prescription only |
| Routes | oral |
Mechanism of Action
The mechanism of action of its antihypertensive effects has not been completely established. Factors which may be involved include:
- Decreased cardiac output,
- Inhibition of renin release by the kidneys,
- Diminution of tonic sympathetic outflow from the vasomotor centers in the brain.
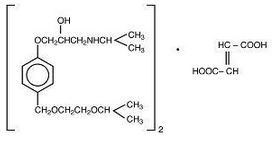
Structure
Bisoprolol fumarate is a synthetic, beta1-selective (cardioselective) adrenoceptor blocking agent. The chemical name for bisoprolol fumarate is (±)-1-[4-((2-(1-Methylethoxy)ethoxy]methyl)phenoxy)-3-[(1-methylethyl)amino]-2-propanol(E)-2-butenedioate (2:1) (salt). It possesses an asymmetric carbon atom in its structure and is provided as a racemic mixture. The S(-) enantiomer is responsible for most of the beta-blocking activity. Its molecular formula is (C18H31NO4)2•C4H4O4 and its structure is:
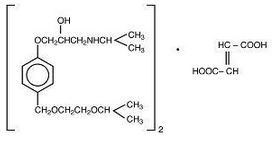
Bisoprolol fumarate has a molecular weight of 766.97. It is a white crystalline powder which is approximately equally hydrophilic and lipophilic, and is readily soluble in water, methanol, ethanol, and chloroform.
Bisoprolol fumarate is available as 5 and 10 mg tablets for oral administration.
Inactive ingredients include microcrystalline cellulose, anhydrous dibasic calcium phosphate, crospovidone, colloidal silicon dioxide, magnesium stearate, hypromellose, polyethylene glycol, polysorbate 80, and titanium dioxide. The 5 mg tablets also contain red and yellow iron oxide.
Pharmacodynamics
Bisoprolol fumarate is a beta1-selective (cardioselective) adrenoceptor blocking agent without significant membrane stabilizing activity or intrinsic sympathomimetic activity in its therapeutic dosage range. Cardioselectivity is not absolute, however, and at higher doses (≥20 mg) bisoprolol fumarate also inhibits beta2-adrenoceptors, chiefly located in the bronchial and vascular musculature; to retain selectivity it is therefore important to use the lowest effective dose.
The most prominent effect of bisoprolol fumarate is the negative chronotropic effect, resulting in a reduction in resting and exercise heart rate. There is a fall in resting and exercise cardiac output with little observed change in stroke volume, and only a small increase in right atrial pressure, or pulmonary capillary wedge pressure at rest or during exercise.
Findings in short-term clinical hemodynamics studies with bisoprolol fumarate are similar to those observed with other beta-blocking agents.
In normal volunteers, bisoprolol fumarate therapy resulted in a reduction of exercise- and isoproterenol-induced tachycardia. The maximal effect occurred within 1 to 4 hours post-dosing. Effects persisted for 24 hours at doses equal to or greater than 5 mg.
Electrophysiology studies in man have demonstrated that bisoprolol fumarate significantly decreases heart rate, increases sinus node recovery time, prolongs AV node refractory periods, and, with rapid atrial stimulation, prolongs AV nodal conduction.
Beta1-selectivity of bisoprolol fumarate has been demonstrated in both animal and human studies. No effects at therapeutic doses on beta2-adrenoceptor density have been observed. Pulmonary function tests have been conducted in healthy volunteers, asthmatics, and patients with chronic obstructive pulmonary disease (COPD). Doses of bisoprolol fumarate ranged from 5 to 60 mg, atenolol from 50 to 200 mg, metoprolol from 100 to 200 mg, and propranolol from 40 to 80 mg. In some studies, slight, asymptomatic increases in airways resistance (AWR) and decreases in forced expiratory volume (FEV1) were observed with doses of bisoprolol fumarate 20 mg and higher, similar to the small increases in AWR also noted with the other cardioselective beta-blockers. The changes induced by beta-blockade with all agents were reversed by bronchodilator therapy.
Bisoprolol fumarate had minimal effect on serum lipids during antihypertensive studies. In U.S. placebo-controlled trials, changes in total cholesterol averaged +0.8% for bisoprolol fumarate-treated patients, and +0.7% for placebo. Changes in triglycerides averaged +19% for bisoprolol fumarate-treated patients, and +17% for placebo.
Bisoprolol fumarate has also been given concomitantly with thiazide diuretics. Even very low doses of hydrochlorothiazide (6.25 mg) were found to be additive with bisoprolol fumarate in lowering blood pressure in patients with mild-to-moderate hypertension.
Pharmacokinetics
The absolute bioavailability after a 10 mg oral dose of bisoprolol fumarate is about 80%. Absorption is not affected by the presence of food. The first pass metabolism of bisoprolol fumarate is about 20%.
Binding to serum proteins is approximately 30%. Peak plasma concentrations occur within 2 to 4 hours of dosing with 5 to 20 mg, and mean peak values range from 16 ng/mL at 5 mg to 70 ng/mL at 20 mg. Once daily dosing with bisoprolol fumarate results in less than twofold intersubject variation in peak plasma levels. The plasma elimination half-life is 9 to 12 hours and is slightly longer in elderly patients, in part because of decreased renal function in that population. Steady state is attained within 5 days of once daily dosing. In both young and elderly populations, plasma accumulation is low; the accumulation factor ranges from 1.1 to 1.3, and is what would be expected from the first order kinetics and once daily dosing. Plasma concentrations are proportional to the administered dose in the range of 5 to 20 mg. Pharmacokinetic characteristics of the two enantiomers are similar.
Bisoprolol fumarate is eliminated equally by renal and non-renal pathways with about 50% of the dose appearing unchanged in the urine and the remainder appearing in the form of inactive metabolites. In humans, the known metabolites are labile or have no known pharmacologic activity. Less than 2% of the dose is excreted in the feces. Bisoprolol fumarate is not metabolized by cytochrome P450 II D6 (debrisoquin hydroxylase).
In subjects with creatinine clearance less than 40 mL/min, the plasma half-life is increased approximately threefold compared to healthy subjects.
In patients with cirrhosis of the liver, the elimination of bisoprolol fumarate is more variable in rate and significantly slower than that in healthy subjects, with plasma half-life ranging from 8.3 to 21.7 hours.
Nonclinical Toxicology
Long-term studies were conducted with oral bisoprolol fumarate administered in the feed of mice (20 and 24 months) and rats (26 months). No evidence of carcinogenic potential was seen in mice dosed up to 250 mg/kg/day or rats dosed up to 125 mg/kg/day. On a body weight basis, these doses are 625 and 312 times, respectively, the maximum recommended human dose (MRHD) of 20 mg, (or 0.4 mg/kg/day based on a 50 kg individual); on a body surface area basis, these doses are 59 times (mice) and 64 times (rats) the MRHD. The mutagenic potential of bisoprolol fumarate was evaluated in the microbial mutagenicity (Ames) test, the point mutation and chromosome aberration assays in Chinese hamster V79 cells, the unscheduled DNA synthesis test, the micronucleus test in mice, and the cytogenetics assay in rats. There was no evidence of mutagenic potential in these in vitro and in vivo assays.
Reproduction studies in rats did not show any impairment of fertility at doses up to 150 mg/kg/day of bisoprolol fumarate, or 375 and 77 times the MRHD on the basis of body weight and body surface area, respectively.
Clinical Studies
In two randomized double-blind placebo-controlled trials conducted in the U.S., reductions in systolic blood pressure and diastolic blood pressure and heart rate 24 hours after dosing in patients with mild-to-moderate hypertension are shown below. In both studies, mean systolic blood pressures/diastolic blood pressures at baseline were approximately 150/100 mm Hg, and mean heart rate was 76 bpm. Drug effect is calculated by subtracting the placebo effect from the overall change in blood pressure and heart rate.
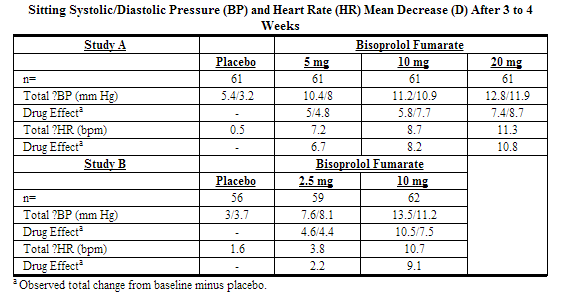
Blood pressure responses were seen within one week of treatment and changed little thereafter. They were sustained for 12 weeks and for over a year in studies of longer duration. Blood pressure returned to baseline when bisoprolol fumarate was tapered over two weeks in a long-term study.
Overall, significantly greater blood pressure reductions were observed on bisoprolol fumarate than on placebo regardless of race, age, or gender. There were no significant differences in response between black and nonblack patients.
How Supplied
(Description)
Storage
There is limited information regarding Bisoprolol Storage in the drug label.
Images
Drug Images
{{#ask: Page Name::Bisoprolol |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
{{#ask: Label Page::Bisoprolol |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
(Patient Counseling Information)
Precautions with Alcohol
Alcohol-Bisoprolol interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
There is limited information regarding Bisoprolol Brand Names in the drug label.
Look-Alike Drug Names
- (Paired Confused Name 1a) — (Paired Confused Name 1b)
- (Paired Confused Name 2a) — (Paired Confused Name 2b)
- (Paired Confused Name 3a) — (Paired Confused Name 3b)
Drug Shortage Status
Drug Shortage
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
- ↑ Bühring KU, Sailer H, Faro HP, Leopold G, Pabst J, Garbe A (1986). "Pharmacokinetics and metabolism of bisoprolol-14C in three animal species and in humans". J. Cardiovasc. Pharmacol. 8 Suppl 11: S21–8. PMID 2439794.
- ↑ Leopold G (1986). "Balanced pharmacokinetics and metabolism of bisoprolol". J. Cardiovasc. Pharmacol. 8 Suppl 11: S16–20. PMID 2439789.