Avulsion fracture: Difference between revisions
No edit summary |
No edit summary |
||
| Line 21: | Line 21: | ||
{{CMG}}; {{AE}}[[User:DrMars|Mohammadmain Rezazadehsaatlou[2]]]. | {{CMG}}; {{AE}}[[User:DrMars|Mohammadmain Rezazadehsaatlou[2]]]. | ||
==Overview | ==Overview== | ||
The injuries of the ball-and-socket shoulder joint considered as the Distal humerus fracture. It is more common among the elderly population following a low energy trauma such as falling. Meanwhile, A few people experience the axillary nerve damage such as reduced sensation around the middle deltoid and/or axillary artery involvement. | The injuries of the ball-and-socket shoulder joint considered as the Distal humerus fracture. It is more common among the elderly population following a low energy trauma such as falling. Meanwhile, A few people experience the axillary nerve damage such as reduced sensation around the middle deltoid and/or axillary artery involvement. | ||
| Line 27: | Line 27: | ||
There are no reliable information regarding the historical perspective of the hip bone fracture. | There are no reliable information regarding the historical perspective of the hip bone fracture. | ||
==Causes | ==Causes== | ||
The main etiology of the [[Distal humerus fracture]] is thought to be an axial loading may be placed on a hyperpronated forearm during falling onto an outstretched hand (FOOSH) with an extended wrist and hyperpronated forearm and shoulder. Because at this posture the energy from the radius fracture transmitted towards the shoulder joint cause the fracture and/or dislocation of the humerus bone. | The main etiology of the [[Distal humerus fracture]] is thought to be an axial loading may be placed on a hyperpronated forearm during falling onto an outstretched hand (FOOSH) with an extended wrist and hyperpronated forearm and shoulder. Because at this posture the energy from the radius fracture transmitted towards the shoulder joint cause the fracture and/or dislocation of the humerus bone. | ||
== Pathophysiology | == Pathophysiology == | ||
=== Mechanism === | === Mechanism === | ||
| Line 49: | Line 49: | ||
** As [[Osteocyte|osteocytes]] grow, viability of cells decrease thereby decreasing the bone mass density. | ** As [[Osteocyte|osteocytes]] grow, viability of cells decrease thereby decreasing the bone mass density. | ||
==Differentiating [[Distal humerus fracture]] from other Diseases | ==Differentiating [[Distal humerus fracture]] from other Diseases== | ||
In the orthopedic medicine its important to know that the forearm fracture should be evaluated using radiography for both confirming diagnosis and also for evaluating the surrounding tissues. Other injuries such as possible shoulder fracture-dislocation; radial head or coronoid fractures or lateral collateral ligament injury. If the mechanism of injury suggests particularly low energy then the Osteoporosis should be considered. The pathological Fractures occurring in a bone with a tumor or Paget's disease) are rare but possible[3]. | In the orthopedic medicine its important to know that the forearm fracture should be evaluated using radiography for both confirming diagnosis and also for evaluating the surrounding tissues. Other injuries such as possible shoulder fracture-dislocation; radial head or coronoid fractures or lateral collateral ligament injury. If the mechanism of injury suggests particularly low energy then the Osteoporosis should be considered. The pathological Fractures occurring in a bone with a tumor or Paget's disease) are rare but possible[3]. | ||
Also it should be noted that the both bone fractures can be complicated by acute compartment syndrome of the forearm. Signs suggesting compartment syndrome are pain on extension of digits, and marked edema[3]. | Also it should be noted that the both bone fractures can be complicated by acute compartment syndrome of the forearm. Signs suggesting compartment syndrome are pain on extension of digits, and marked edema[3]. | ||
| Line 57: | Line 57: | ||
* Elbow Dislocation | * Elbow Dislocation | ||
==Epidemiology and Demographics | ==Epidemiology and Demographics == | ||
The elbow joint fractures count for 4.3% of all fractures. Meanwhile, the distal humerus fractures account for 2% of all fractures. Also, it count as 30% the elbow fracture. both medial and lateral columns are usually involved in distal humerus fractures. Comparing to epidemiological data of the Japan and European countries, the incidence rates of humerus fractures are higher in the United states population. | The elbow joint fractures count for 4.3% of all fractures. Meanwhile, the distal humerus fractures account for 2% of all fractures. Also, it count as 30% the elbow fracture. both medial and lateral columns are usually involved in distal humerus fractures. Comparing to epidemiological data of the Japan and European countries, the incidence rates of humerus fractures are higher in the United states population. | ||
==Risk Factors | ==Risk Factors == | ||
There are different risk factors that presidpose patient for the [[Distal humerus fracture]] that include: | There are different risk factors that presidpose patient for the [[Distal humerus fracture]] that include: | ||
* High-risk contact sports | * High-risk contact sports | ||
| Line 73: | Line 73: | ||
* Road traffic accidents. | * Road traffic accidents. | ||
== Classification | == Classification == | ||
The distal humerus fracture may be classified based on the exact location of fracture: | The distal humerus fracture may be classified based on the exact location of fracture: | ||
==Screening | ==Screening== | ||
Osteoporosis is an important risk factor for human affecting human bone especially in men with the age of older than 50 years old and [[postmenopausal]] and women. | Osteoporosis is an important risk factor for human affecting human bone especially in men with the age of older than 50 years old and [[postmenopausal]] and women. | ||
| Line 102: | Line 102: | ||
· Women with advanced [[osteopenia]]: T-score of −2.00 to −2.49 - should have screening for 1 year. | · Women with advanced [[osteopenia]]: T-score of −2.00 to −2.49 - should have screening for 1 year. | ||
==Natural History, Complications and Prognosis | ==Natural History, Complications and Prognosis == | ||
=== Natural History | === Natural History === | ||
In cases with untreated [[Distal humerus fracture]] the malunion and deformity of arm can be occurred. | In cases with untreated [[Distal humerus fracture]] the malunion and deformity of arm can be occurred. | ||
=== Complications | === Complications === | ||
The overall complication rate in the treatment of [[Humerus fracture]] were found in around 40% of cases: | The overall complication rate in the treatment of [[Humerus fracture]] were found in around 40% of cases: | ||
# Neurovascular compromise: such as Ulna nerve damage | # Neurovascular compromise: such as Ulna nerve damage | ||
| Line 129: | Line 129: | ||
The diagnosis of a [[Distal humerus fracture]] should be confirmed using a radiographic examination. | The diagnosis of a [[Distal humerus fracture]] should be confirmed using a radiographic examination. | ||
==History and Symptoms | ==History and Symptoms == | ||
The related signs and symptoms include: | The related signs and symptoms include: | ||
* Skin lacerations | * Skin lacerations | ||
| Line 144: | Line 144: | ||
In the physical exam the orthopedic surgeon should check the vascular status and amount of swelling in the forearm. In MULTI-trauma patients or in comatose or obtunded patients a tense compartment with neurological signs or stretch pain should be considered as the [[compartment syndrome]], and the compartment pressures should be measured and monitored. Normally the pain and soft-tissue swelling are found at the injury site (distal-third radial fracture site and at the wrist joint). This injury should be confirmed using a radiographic evaluations. Also, patients may loss the pinch mechanism between their thumb and their index finger which can be due to the paralysis of the flexor pollicis longus (FPL) and flexor digitorum profundus (FDP). | In the physical exam the orthopedic surgeon should check the vascular status and amount of swelling in the forearm. In MULTI-trauma patients or in comatose or obtunded patients a tense compartment with neurological signs or stretch pain should be considered as the [[compartment syndrome]], and the compartment pressures should be measured and monitored. Normally the pain and soft-tissue swelling are found at the injury site (distal-third radial fracture site and at the wrist joint). This injury should be confirmed using a radiographic evaluations. Also, patients may loss the pinch mechanism between their thumb and their index finger which can be due to the paralysis of the flexor pollicis longus (FPL) and flexor digitorum profundus (FDP). | ||
==Physical Examination | ==Physical Examination== | ||
The related signs and symptoms include: | The related signs and symptoms include: | ||
* Edema of the shoulder | * Edema of the shoulder | ||
| Line 197: | Line 197: | ||
* However, some patients may develop [[neuropraxia]] of the branch of the Ulnar nerve resulting in decreased sensation of thumb, index and middle finger. | * However, some patients may develop [[neuropraxia]] of the branch of the Ulnar nerve resulting in decreased sensation of thumb, index and middle finger. | ||
==Laboratory Findings | ==Laboratory Findings== | ||
There is a limited laboratory tests useful in the diagnosis of bone fractures such as the [[Distal humerus fracture]]. Meanwhile, aged men and women may have some abnormalities in their laboratory findings suggestive of osteoporosis. | There is a limited laboratory tests useful in the diagnosis of bone fractures such as the [[Distal humerus fracture]]. Meanwhile, aged men and women may have some abnormalities in their laboratory findings suggestive of osteoporosis. | ||
| Line 216: | Line 216: | ||
</gallery> | </gallery> | ||
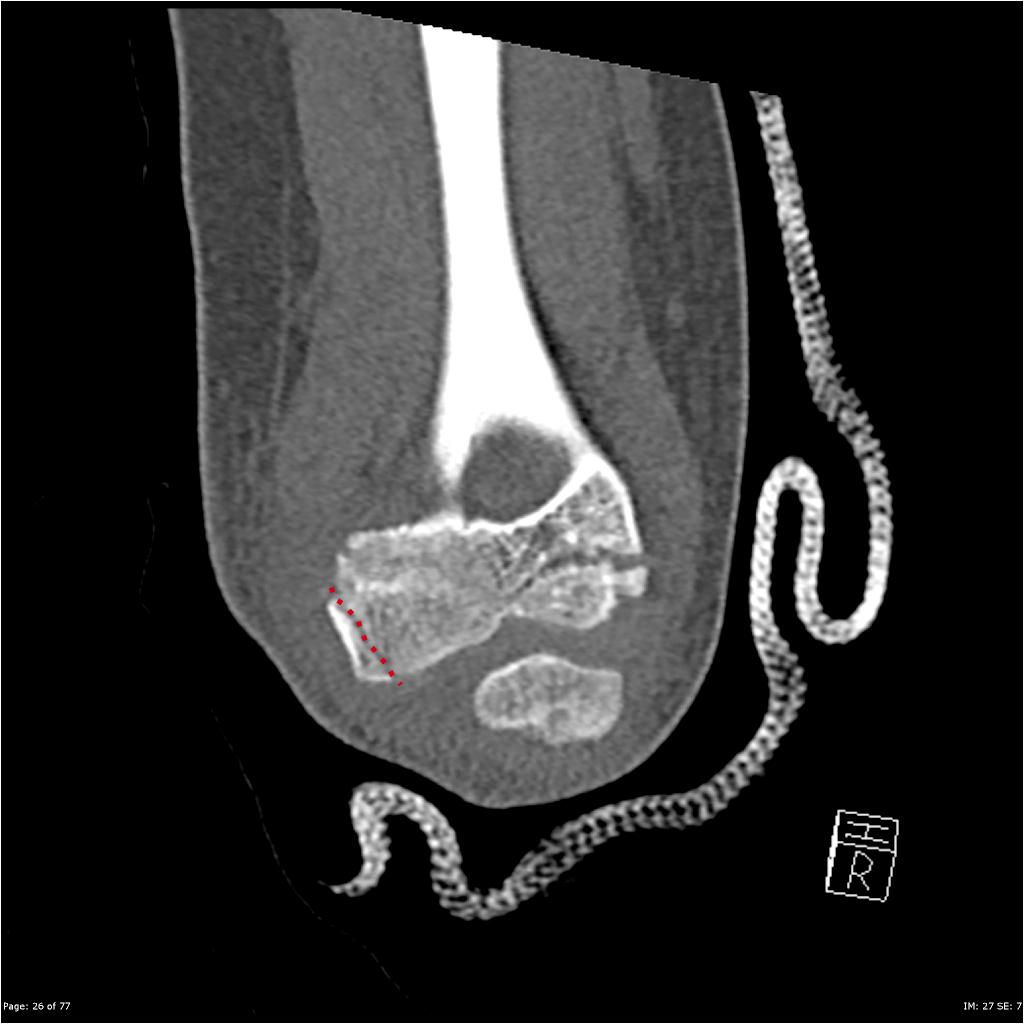
==CT | ==CT == | ||
* CT-scan in the case of the [[Humerus fracture]]is the best modality if you can not have an exclusive diagnosis by X-ray itself can not be made. | * CT-scan in the case of the [[Humerus fracture]]is the best modality if you can not have an exclusive diagnosis by X-ray itself can not be made. | ||
<gallery perrow="3"> | <gallery perrow="3"> | ||
| Line 223: | Line 223: | ||
</gallery> | </gallery> | ||
==MRI | ==MRI == | ||
* Magnetic resonance imaging (MRI) is an expensive technique that should not be used routinely. | * Magnetic resonance imaging (MRI) is an expensive technique that should not be used routinely. | ||
* MRI is a powerful diagnostic tool to assess the abnormalities of the bone, ligaments and soft tissues associated with the [[Distal humerus fracture]], but it is known as a limited utility in radioulnar injuries and is not indicated in uncomplicated forearm fractures. | * MRI is a powerful diagnostic tool to assess the abnormalities of the bone, ligaments and soft tissues associated with the [[Distal humerus fracture]], but it is known as a limited utility in radioulnar injuries and is not indicated in uncomplicated forearm fractures. | ||
| Line 239: | Line 239: | ||
There are no other Diagnostic studies associated with [[Distal humerus fracture]] | There are no other Diagnostic studies associated with [[Distal humerus fracture]] | ||
==Treatment | ==Treatment == | ||
Immediate stabilization of patients is the first step. Then the radial fracture and the DRUJ stabilization is recommended in these cases. Open forearm fractures considered as a surgical emergency. [[Humerus fracture]] occurs in younger patients who are skeletally immature; the normally they treated using a closed reduction and casting. Since closed reduction and cast application have led to unsatisfactory results. Then, Almost always the open reduction are necessary for the [[Humerus fracture]]. There are controversies regarding the indications for intramedullary nailing of forearm fractures. | Immediate stabilization of patients is the first step. Then the radial fracture and the DRUJ stabilization is recommended in these cases. Open forearm fractures considered as a surgical emergency. [[Humerus fracture]] occurs in younger patients who are skeletally immature; the normally they treated using a closed reduction and casting. Since closed reduction and cast application have led to unsatisfactory results. Then, Almost always the open reduction are necessary for the [[Humerus fracture]]. There are controversies regarding the indications for intramedullary nailing of forearm fractures. | ||
| Line 262: | Line 262: | ||
** Stiffness is universal following a prolonged period of immobilization and swelling | ** Stiffness is universal following a prolonged period of immobilization and swelling | ||
==Surgery | ==Surgery == | ||
Returning to the normal physical activity after [[Distal humerus fracture]]can take weeks to months of therapy under supervision an orthopedist. Meanwhile, a physiotherapy can be helpful for patient to achieve the normal wrist and elbow function caused by the immobilisation. All adult [[Distal humerus fracture]] should be considered to be treated with open reduction and internal fixation (ORIF). | Returning to the normal physical activity after [[Distal humerus fracture]]can take weeks to months of therapy under supervision an orthopedist. Meanwhile, a physiotherapy can be helpful for patient to achieve the normal wrist and elbow function caused by the immobilisation. All adult [[Distal humerus fracture]] should be considered to be treated with open reduction and internal fixation (ORIF). | ||
| Line 314: | Line 314: | ||
=== Be aware that although opioids help relieve pain after surgery or an injury, they are a narcotic and can be addictive. It is important to use opioids only as directed by doctor. === | === Be aware that although opioids help relieve pain after surgery or an injury, they are a narcotic and can be addictive. It is important to use opioids only as directed by doctor. === | ||
=== Interventions | === Interventions === | ||
The following options can be helpful for patients to rehabilitate after their fracture : | The following options can be helpful for patients to rehabilitate after their fracture : | ||
* Joints mobilization | * Joints mobilization | ||
| Line 323: | Line 323: | ||
* Forearm bracing | * Forearm bracing | ||
== Postoperative Rehabilitation | == Postoperative Rehabilitation <ref name="pmid26778627">{{cite journal |vauthors=Ayoub MA, Khalil AE, Seleem OA |title=Distal humerus fractures nonunion with elbow stiffness in working adults: Can triple tension band technique and Lambda Plate(®) be a standby solution? |journal=J Orthop Sci |volume=21 |issue=2 |pages=147–53 |date=March 2016 |pmid=26778627 |doi=10.1016/j.jos.2015.12.014 |url=}}</ref>== | ||
* Complex [[Humerus fracture]] warrant individualized immobilization and rehabilitation strategies. | * Complex [[Humerus fracture]] warrant individualized immobilization and rehabilitation strategies. | ||
* Similarly, the addition of a thumb spica [[Orthopedic cast|cast]] or [[orthosis]] with positioning of the [[wrist]] in slight ulnar deviation for management of a [[comminuted]] radial column fracture may prevent loss of reduction. *Because most multifragmentary [[Humerus fracture]] are the result of high-energy injuries, a prolonged period of [[wrist]] immobilization and [[Soft tissue|soft-tissue]] rest may be beneficial and has not been shown to affect clinical outcomes. | * Similarly, the addition of a thumb spica [[Orthopedic cast|cast]] or [[orthosis]] with positioning of the [[wrist]] in slight ulnar deviation for management of a [[comminuted]] radial column fracture may prevent loss of reduction. *Because most multifragmentary [[Humerus fracture]] are the result of high-energy injuries, a prolonged period of [[wrist]] immobilization and [[Soft tissue|soft-tissue]] rest may be beneficial and has not been shown to affect clinical outcomes. | ||
| Line 342: | Line 342: | ||
# Healthy diet | # Healthy diet | ||
==Secondary Prevention | ==Secondary Prevention== | ||
It should be noted that the Post-menopausal women specially older than the age of 65 are at the higher risk of [[osteoporosis]] consequently these type of patients at greater risk for the pathological [[Bone fracture|fractures]] . | It should be noted that the Post-menopausal women specially older than the age of 65 are at the higher risk of [[osteoporosis]] consequently these type of patients at greater risk for the pathological [[Bone fracture|fractures]] . | ||
So the [[Calcium]] and [[vitamin D]] supplementation play important role in increasing the [[Bone mineral density|bone mineral density (BMD]]) consequently decrease the risk of fracture in these type of patients. Also, avoiding excessive [[alcohol]] and quitting [[smoking]] play important role in this regard. | So the [[Calcium]] and [[vitamin D]] supplementation play important role in increasing the [[Bone mineral density|bone mineral density (BMD]]) consequently decrease the risk of fracture in these type of patients. Also, avoiding excessive [[alcohol]] and quitting [[smoking]] play important role in this regard. | ||
=== Detecting osteoporosis | === Detecting osteoporosis=== | ||
* [[Dual energy X-ray absorptiometry|DEXA]](dual-energy x-ray absorptiometry) scan | * [[Dual energy X-ray absorptiometry|DEXA]](dual-energy x-ray absorptiometry) scan | ||
* Serum [[calcium]] and [[vitamin D]] levels | * Serum [[calcium]] and [[vitamin D]] levels | ||
* [[Medical ultrasonography|Ultrasonography]] of the [[calcaneus]] | * [[Medical ultrasonography|Ultrasonography]] of the [[calcaneus]] | ||
=== Pharmacological therapy | === Pharmacological therapy === | ||
* The primary goal for the treatment of [[osteoporosis]] is to reduce longtime [[fracture]] risk in patients. Increasing [[Bone mineral density|bone mineral density (BMD)]] in response to the treatment is far less important than improvement of clinical aspects of [[osteoporosis]], i.e., [[Osteoporosis|osteoporotic]][[Bone fracture|fracture]]. Therefore, most of the [[drugs]] efficacy is measured by the extent they improve the [[fracture]] risk instead of increasing [[Bone mineral density|BMD]]. | * The primary goal for the treatment of [[osteoporosis]] is to reduce longtime [[fracture]] risk in patients. Increasing [[Bone mineral density|bone mineral density (BMD)]] in response to the treatment is far less important than improvement of clinical aspects of [[osteoporosis]], i.e., [[Osteoporosis|osteoporotic]][[Bone fracture|fracture]]. Therefore, most of the [[drugs]] efficacy is measured by the extent they improve the [[fracture]] risk instead of increasing [[Bone mineral density|BMD]]. | ||
* During the treatment, if a single [[fracture]] happens, it does not necessarily indicate treatment failure or the need to be started on an alternative treatment or patient referral to a [[specialist]]. | * During the treatment, if a single [[fracture]] happens, it does not necessarily indicate treatment failure or the need to be started on an alternative treatment or patient referral to a [[specialist]]. | ||
* [[Calcium]] and [[vitamin D]] supplementation have been found to be effective in reducing the long term [[Bone fracture|fracture]] risk, significantly. In order to suggest the people to use [[vitamin D]] and [[calcium]] [[supplements]], the [[physician]] needs to make sure that patient is not able to obtain the [[nutrients]] through the daily intake. The available supplemental ions of [[calcium]] include [[calcium carbonate]], [[Calcium citrate|calcium citrate,]] and [[vitamin D3]] in various [[Dosage form|dosage forms]]. | * [[Calcium]] and [[vitamin D]] supplementation have been found to be effective in reducing the long term [[Bone fracture|fracture]] risk, significantly. In order to suggest the people to use [[vitamin D]] and [[calcium]] [[supplements]], the [[physician]] needs to make sure that patient is not able to obtain the [[nutrients]] through the daily intake. The available supplemental ions of [[calcium]] include [[calcium carbonate]], [[Calcium citrate|calcium citrate,]] and [[vitamin D3]] in various [[Dosage form|dosage forms]]. | ||
=== Life style modifications | === Life style modifications<ref name="pmid18374809">{{cite journal |vauthors=Pollock JW, Faber KJ, Athwal GS |title=Distal humerus fractures |journal=Orthop. Clin. North Am. |volume=39 |issue=2 |pages=187–200, vi |date=April 2008 |pmid=18374809 |doi=10.1016/j.ocl.2007.12.002 |url=}}</ref>=== | ||
* [[Exercise]]: Exercise promotes the [[mineralization]] of [[bone]] and [[bone]] accumulation particularly during growth. High impact exercise, in particular, has been shown to prevent the development of [[osteoporosis]]. However, it can have a negative effect on bone [[mineralization]] in cases of poor [[nutrition]], such as [[anorexia nervosa]] and [[celiac disease]]. | * [[Exercise]]: Exercise promotes the [[mineralization]] of [[bone]] and [[bone]] accumulation particularly during growth. High impact exercise, in particular, has been shown to prevent the development of [[osteoporosis]]. However, it can have a negative effect on bone [[mineralization]] in cases of poor [[nutrition]], such as [[anorexia nervosa]] and [[celiac disease]]. | ||
* [[Nutrition]]: A [[diet]] high in [[calcium]] and [[vitamin D]] prevents [[bone loss]]. Patients at risk for [[osteoporosis]], such as persons with chronic [[steroid]] use are generally treated with [[vitamin D]] and [[calcium]] supplementation. In [[Kidney|renal]] disease, more active forms of [[vitamin D]], such as 1,25-dihydroxycholecalciferol or [[calcitriol]] are used; as the kidney cannot adequately generate [[calcitriol]] from [[calcidiol]] (25-hydroxycholecalciferol), which is the storage form of [[vitamin D]]. | * [[Nutrition]]: A [[diet]] high in [[calcium]] and [[vitamin D]] prevents [[bone loss]]. Patients at risk for [[osteoporosis]], such as persons with chronic [[steroid]] use are generally treated with [[vitamin D]] and [[calcium]] supplementation. In [[Kidney|renal]] disease, more active forms of [[vitamin D]], such as 1,25-dihydroxycholecalciferol or [[calcitriol]] are used; as the kidney cannot adequately generate [[calcitriol]] from [[calcidiol]] (25-hydroxycholecalciferol), which is the storage form of [[vitamin D]]. | ||
| Line 385: | Line 385: | ||
==References== | ==References== | ||
<references /> | <references /> | ||
Revision as of 21:56, 12 May 2019
| Avulsion fracture | |
| ICD-10 | S42.2-S42.4 |
|---|---|
| ICD-9 | 812 |
| eMedicine | emerg/199 orthoped/271 orthoped/199 |
|
WikiDoc Resources for Avulsion fracture |
|
Articles |
|---|
|
Most recent articles on Avulsion fracture Most cited articles on Avulsion fracture |
|
Media |
|
Powerpoint slides on Avulsion fracture |
|
Evidence Based Medicine |
|
Cochrane Collaboration on Avulsion fracture |
|
Clinical Trials |
|
Ongoing Trials on Avulsion fracture at Clinical Trials.gov Trial results on Avulsion fracture Clinical Trials on Avulsion fracture at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Avulsion fracture NICE Guidance on Avulsion fracture
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Avulsion fracture Discussion groups on Avulsion fracture Patient Handouts on Avulsion fracture Directions to Hospitals Treating Avulsion fracture Risk calculators and risk factors for Avulsion fracture
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Avulsion fracture |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Mohammadmain Rezazadehsaatlou[2].
Overview
The injuries of the ball-and-socket shoulder joint considered as the Distal humerus fracture. It is more common among the elderly population following a low energy trauma such as falling. Meanwhile, A few people experience the axillary nerve damage such as reduced sensation around the middle deltoid and/or axillary artery involvement.
Historical Perspective
There are no reliable information regarding the historical perspective of the hip bone fracture.
Causes
The main etiology of the Distal humerus fracture is thought to be an axial loading may be placed on a hyperpronated forearm during falling onto an outstretched hand (FOOSH) with an extended wrist and hyperpronated forearm and shoulder. Because at this posture the energy from the radius fracture transmitted towards the shoulder joint cause the fracture and/or dislocation of the humerus bone.
Pathophysiology
Mechanism
The Distal humerus fracture is caused by a fall on the outstretched hands. The form and severity of this fracture depends on the position of the shoulder joint at the moment of hitting the ground. The width of this mentioned angle affects the localization of the fracture. Pronation, supination and abduction positions leads the direction of the force and the compression of carpus and different appearances of injury.
Pathophysiology
Its known that the Distal humerus fracture in normal healthy adults can be caused due to the high-energy trauma (e.g., motor vehicle accidents), sport related injuries, falling from height. But it should be noted that the most important Risk factors for insufficiency fractures is chronic metabolic disease such as steoporosis, osteopenia, eating-disordered behavior, higher age, prolonged corticosteroid usage, female gender, lower BMI, history of a recent falling, and prior fracture.
- The pattern of bone fracture and severity of injury depends on variety of factors such as:
- Patients age
- Patients Weight
- Patients past medical history specifically any bone diseases affecting the quality of bone (such as osteoporosis, malignancies)
- Energy of trauma
- Bone quality
- Position of the specific organ during the trauma
- The below-mentioned processes cause decreased bone mass density:
- Autophagy is the mechanism through which osteocytes evade oxidative stress.
- The capability of autophagy in cells decreases as they age, a major factor of aging.
- As osteocytes grow, viability of cells decrease thereby decreasing the bone mass density.
Differentiating Distal humerus fracture from other Diseases
In the orthopedic medicine its important to know that the forearm fracture should be evaluated using radiography for both confirming diagnosis and also for evaluating the surrounding tissues. Other injuries such as possible shoulder fracture-dislocation; radial head or coronoid fractures or lateral collateral ligament injury. If the mechanism of injury suggests particularly low energy then the Osteoporosis should be considered. The pathological Fractures occurring in a bone with a tumor or Paget's disease) are rare but possible[3]. Also it should be noted that the both bone fractures can be complicated by acute compartment syndrome of the forearm. Signs suggesting compartment syndrome are pain on extension of digits, and marked edema[3]. As another important fact in orthopedic fracture is if both-bone fractures were found in pediatric which is common after accidental trauma, but it may also be the due to the of child abuse; and in these cases a careful attention and evaluation should be considered if a child abuse is suspected Differential Diagnoses for the Distal humerus fracture:
- Elbow Fracture
- Elbow Dislocation
Epidemiology and Demographics
The elbow joint fractures count for 4.3% of all fractures. Meanwhile, the distal humerus fractures account for 2% of all fractures. Also, it count as 30% the elbow fracture. both medial and lateral columns are usually involved in distal humerus fractures. Comparing to epidemiological data of the Japan and European countries, the incidence rates of humerus fractures are higher in the United states population.
Risk Factors
There are different risk factors that presidpose patient for the Distal humerus fracture that include:
- High-risk contact sports
- Higher age (elderly adults are higher prone to such fractures)
- Reduced bone density (osteoporosis)
- Direct blow
- Road / traffic accidents
- Falling on an outstretched hand with the forearm pronated
- Direct trauma to the arm/forearm
- Taking part in any rough or high-impact sport
- Street fights, gunshot wounds, and domestic violence, may also cause the Humerus fracture
- Road traffic accidents.
Classification
The distal humerus fracture may be classified based on the exact location of fracture:
Screening
Osteoporosis is an important risk factor for human affecting human bone especially in men with the age of older than 50 years old and postmenopausal and women.
Based on the US Preventive Services Task Force (USPSTF) there are three groups of patients need to be screened for the osteoporosis:
- · Men with no history of osteoporosis
- · Women with the age of 65≤ year old, with no previous history of pathological fracture due to the osteoporosis
- · Women with the age of <65 years, with 10-year fracture risk of not less than a 65-year-old white woman (who has not any other risk factor)
Accordingly women older than age of 50 are the main target for the osteoporosis screening. There is no specific recommendation to screen men for the osteoporosis.[1]
The USPSTF recommendations from 2002 included:
Meanwhile, there are two major modalities for the osteoporosis screening:
- · Dual energy x-ray absorptiometry (DXA) of the hip and lumbar spine bones
- · Quantitative ultrasonography of the calcaneus
*It should be noted of the two above mentioned modalities for screening the ultrasonograhy is preferred to the DXA due to its lower cost, lower ionizing radiation, more availability.
After the primary evaluation of the osteoporosis, the further evaluation are required in some cases such as:
· Women with normal bone density or mild osteopenia: T-score of greater than −1.50 – should have screening for 15 years.
· Women with moderate osteopenia: T-score of −1.50 to −1.99 – should have screening for 5 years.
· Women with advanced osteopenia: T-score of −2.00 to −2.49 - should have screening for 1 year.
Natural History, Complications and Prognosis
Natural History
In cases with untreated Distal humerus fracture the malunion and deformity of arm can be occurred.
Complications
The overall complication rate in the treatment of Humerus fracture were found in around 40% of cases:
- Neurovascular compromise: such as Ulna nerve damage
- Compartment syndrome
- Chronic disability of the DRUJ
- Physeal Injury
- Malunion of the radius
- Nonunion
- Infection
- Refracture following plate removal
- Posterior interosseois nerve (PIN) injury.
- Instability of the DRUJ
- Loss of Motion (Stiffness)
- Posttraumatic Arthritis
- Heterotopic Ossification
Prognosis [1]
Successful treatment of Distal humerus fracture depends on the on-time interventions such as: reduction of the radius and DRUJ and the restoration of the forearm axis. The incidence of nonunion of Humerus fracture is very low. On the other hand, the rate of successful union following the open reduction of forearm fractures was reported around 98%. Loss of terminal extension is common among cases with the distal humerus fracture and the chronic exertional pain can be found in around 25% of patients with the distal humerus fracture.
Diagnosis[2]
The diagnosis of a Distal humerus fracture should be confirmed using a radiographic examination.
History and Symptoms
The related signs and symptoms include:
- Skin lacerations
- Weak pulse
- Open fractures
- Bruising
- Swelling
- Stiffness
- Inability to move
- Pain in touch
- Loss of function of the forearm
- Difficulties in detection of pulses
- Radial nerve damage
In the physical exam the orthopedic surgeon should check the vascular status and amount of swelling in the forearm. In MULTI-trauma patients or in comatose or obtunded patients a tense compartment with neurological signs or stretch pain should be considered as the compartment syndrome, and the compartment pressures should be measured and monitored. Normally the pain and soft-tissue swelling are found at the injury site (distal-third radial fracture site and at the wrist joint). This injury should be confirmed using a radiographic evaluations. Also, patients may loss the pinch mechanism between their thumb and their index finger which can be due to the paralysis of the flexor pollicis longus (FPL) and flexor digitorum profundus (FDP).
Physical Examination
The related signs and symptoms include:
- Edema of the shoulder
- Most of the time the edema will be a non-pitting edema
- Depends on the edema extent, it may even lead to compartment syndrome in the anterior and internal compartment of shoulder
- Bruising
- As a manifestation of internal injury to the local vessels by trauma or fractures bone
- Decrease in range of motion
- Movement of the fractures limb will be painful if possible at all
- Tenderness
- Deformity
- Fractured bone deformity may be touchable in the internal side of the forearm if the fracture is displaced
In the physical exam the orthopedic surgeon should check the vascular status and amount of swelling in the forearm. In polytrauma patients or in comatose or obtunded patients a tense compartment with neurological signs or stretch pain should be considered as the compartment syndrome, and the compartment pressures should be measured and monitored.
Physical examination of patients with Distal humerus fracture is usually remarkable for swelling, tenderness, bruises, ecchymosis, deformity and restricted range of motion of the wrist.
Appearance of the Patient
- Patients with Distal humerus fracture usually appears normal unless the patients had a high energy trauma causing the open wound fracture.
Vital Signs
- Weak pulse may be seen when associated with polytrauma.
- Low blood pressure with normal pulse pressure may be present due to compound fracture with blood loss.
Skin
- Skin examination of patients with Distal humerus fracture includes:
HEENT
- HEENT examination of patients with Distal humerus fracture usually normal.
Neck
- Neck examination of patients with Distal humerus fracture is usually normal
Lungs
- Pulmonary examination of patients with Distal humerus fracture usually normal
Heart
- Cardiovascular examination of patients with Distal humerus fracture usually normal
Abdomen
- Abdominal examination of patients with Distal humerus fracture usually normal
Back
- Back examination of patients with Distal humerus fracture usually normal
Genitourinary
- Genitourinary examination of patients with Distal humerus fracture usually normal
Neuromuscular
- Neuromuscular examination of patients with Distal humerus fracture is usually normal
- However, some patients may develop neuropraxia of the branch of the Ulnar nerve resulting in decreased sensation of thumb, index and middle finger.
Laboratory Findings
There is a limited laboratory tests useful in the diagnosis of bone fractures such as the Distal humerus fracture. Meanwhile, aged men and women may have some abnormalities in their laboratory findings suggestive of osteoporosis.
Laboratory tests for the diagnosis of osteoporosis are:
- Complete blood count (CBC)
- Serum total calcium level
- Serum Ionized calcium level
- Serum phosphate level
- Serum alkaline phosphatase level
- Serum 25-(OH)-vitamin D level
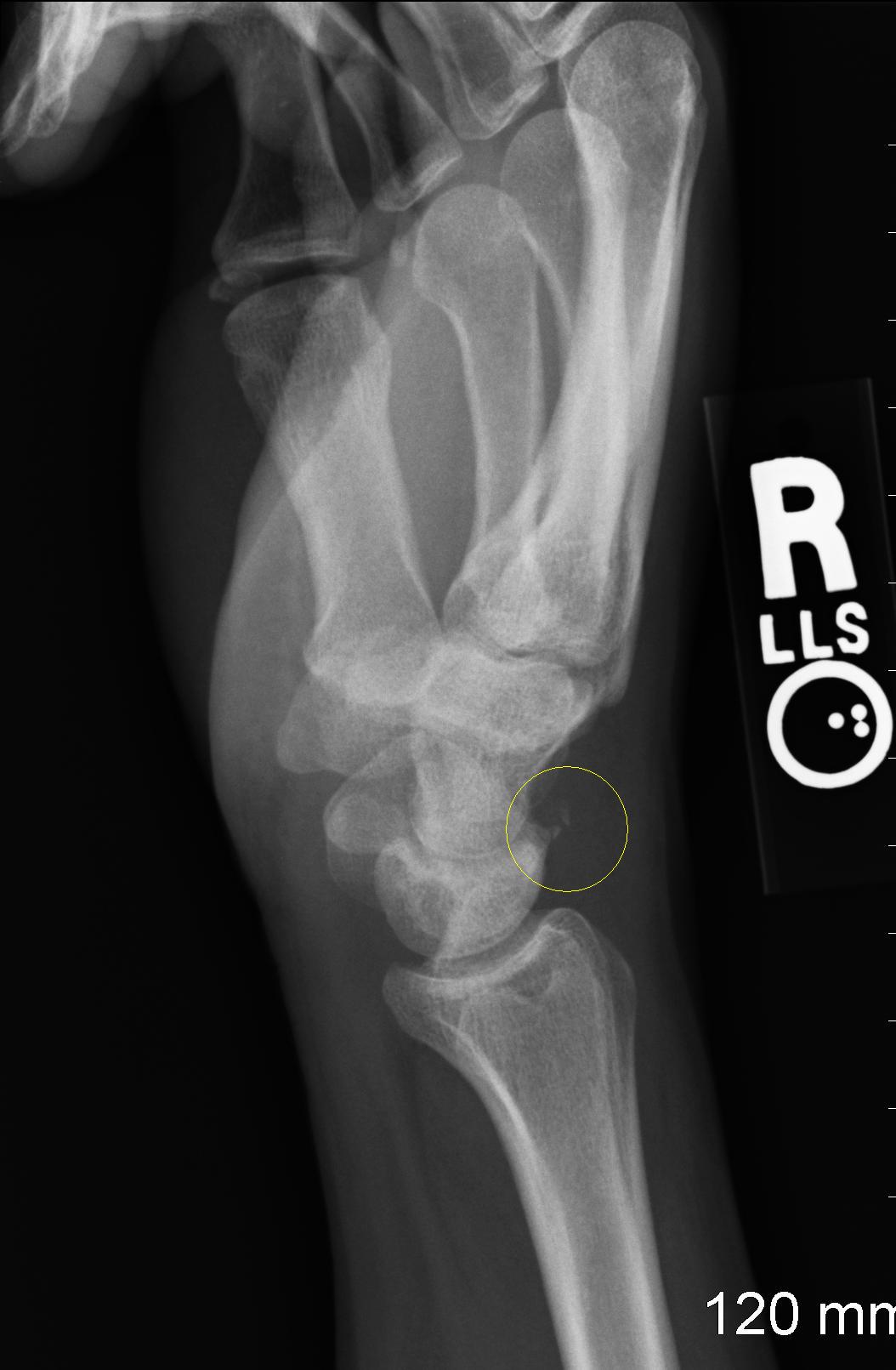
X Ray [3][4]
The orthopedic surgeon should consider to have at least two radiographic projections (ie, anteroposterior [AP] and lateral) of the forearm. These show the fracture, the extent of displacement, and the extent of comminution. The orthopedic surgeon should pay serious attention toward finding any foreign bodies in open fractures and gunshot injuries. Also imperative is to include the elbow and wrist joint in the radiographs of Humerus fracture to ensure that the distal radioulnar joint injuries are not missed.
-
There is an obvious supracondylar fracture with posterior displacement of the distal fracture fragment and no communication between the cotices.
CT
- CT-scan in the case of the Humerus fractureis the best modality if you can not have an exclusive diagnosis by X-ray itself can not be made.
-
The oblique fracture through the capitellum is clearly demonstrated on the CT.
MRI
- Magnetic resonance imaging (MRI) is an expensive technique that should not be used routinely.
- MRI is a powerful diagnostic tool to assess the abnormalities of the bone, ligaments and soft tissues associated with the Distal humerus fracture, but it is known as a limited utility in radioulnar injuries and is not indicated in uncomplicated forearm fractures.
- Meanwhile, the MRI can be useful in in following mentioned evaluations:
- Evaluation of occult fractures
- Evaluation of the post-traumatic or avascular necrosis of carpal bones
- Evaluation of tendons
- Evaluation of nerve
- Evaluation of carpal tunnel syndrome
Other Imaging Findings[5]
There are no other imaging findings associated with Distal humerus fracture
Other Diagnostic Studies[5]
There are no other Diagnostic studies associated with Distal humerus fracture
Treatment
Immediate stabilization of patients is the first step. Then the radial fracture and the DRUJ stabilization is recommended in these cases. Open forearm fractures considered as a surgical emergency. Humerus fracture occurs in younger patients who are skeletally immature; the normally they treated using a closed reduction and casting. Since closed reduction and cast application have led to unsatisfactory results. Then, Almost always the open reduction are necessary for the Humerus fracture. There are controversies regarding the indications for intramedullary nailing of forearm fractures.
Non-Operative Treatmen [6][7]
- The first step in managing a patient with a fracture is to stabilize the patient if he/she is unstable due to blood loss, etc by giving them intravenous fluids and giving them some painkillers if the pain is severe.
- In children, the usual plan is to attempt closed reduction followed by cast immobilization. In adults, treatment with immobilization in a molded long arm cast can be used in those rare occasions of a non-displaced fracture of both bones of the forearm. If the fracture shifts in position, it may require surgery to put the bones back together.
- Rigid immobilization is suggested in preference to removable splints in nonoperative treatment for the management of the Distal humerus fracture
- For all patients with Humerus fracture, a post-reduction true lateral radiograph is suggested .
- Operative fixation is suggested in preference to cast fixation for fractures with post-reduction radial shortening greater than 3 mm, dorsal tilt greater than 10º, or intra-articular displacement or step-off greater than 2 mm.
- Patients probably do not need to begin early wrist motion routinely after stable fracture fixation.
- Adjuvant treatment of Distal humerus fracture with vitamin C is suggested for the prevention of disproportionate pain
- The medial epicondylar fractures should be immobilized for 7 days with patients elbow flexed at 90º, with the pronated forearm , and the flexed wrist at 30º for relaxing the common flexor-pronator muscle group. If more than 3 mm of displacement is present or the fragment is trapped in the medial joint, attempts at closed reduction often fail, and ORIF is necessary.
- Lateral epicondylar fractures should be immobilized for 7 days with patients elbow flexed at 90º, with the supinated forearm , and the extended wrist for relaxing the extensor muscles.
Complications of Non-surgical therapy
Failure of non-surgical therapy is common:
- Re-displacement to its original position even in a cast
- Stiffness
- Post traumatic osteoarthritis leading to wrist pain and loss of function
- Other risks specific to cast treatment include:
- Compression of the swollen arm causing compartment syndrome
- Reflex sympathetic dystrophy is a serious complication
- Stiffness is universal following a prolonged period of immobilization and swelling
Surgery
Returning to the normal physical activity after Distal humerus fracturecan take weeks to months of therapy under supervision an orthopedist. Meanwhile, a physiotherapy can be helpful for patient to achieve the normal wrist and elbow function caused by the immobilisation. All adult Distal humerus fracture should be considered to be treated with open reduction and internal fixation (ORIF).
External fixation: For severe open fractures Open reduction and internal fixation: For distal humerus fractures which depending on each patients condition the following may be needed:
Ulnar nerve placement Bone grafting Osteotomy Arthrodesis
-
Internal fixation using two Kirschner wires laterally.
Operation [8]
- There are a variety of methods and implants useful to stabilize the Distal humerus fracture, ranging from closed reduction and percutaneous pin fixation to the use of intra-medullary devices.
- However, the most common fixation methods to treat complex Distal humerus fracture include external fixation, and open reduction and internal fixation.
External Fixation With or Without Percutaneous Pin Fixation
- Wrist spanning external fixation employs ligamentotaxis to restore and maintain length, alignment, and rotation of ulnar bone.
- Reduction is typically obtained through closed or minimally open methods and preserves the fracture biology.
- The addition of percutaneous pins enhances the ability to reduce and stabilize fracture fragments.
Complications of External Fixation
- Pin tract infection
- Injury to the superficial branch of the nerve
- Complex regional pain syndrome
Open reduction and internal fixation with plates and screws
- This is the most common type of surgical repair for Distal humerusfracture
- During this type of procedure, the bone fragments are first repositioned (reduced) into their normal alignment.
- The bones held together with special screws and metal plates attached to the outer surface of the bone.
Complications of open reduction and internal fixation with plates and screws =
- Infection
- Damage to nerves and blood vessels
- Synostosis
- Nonunion
Pain Management
Pain after an injury or surgery is a natural part of the healing process.
Medications are often prescribed for short-term pain relief after surgery or an injurysuch as:
- opioids
- non-steroidal anti-inflammatory drugs (NSAIDs)
- local anesthetics
Be aware that although opioids help relieve pain after surgery or an injury, they are a narcotic and can be addictive. It is important to use opioids only as directed by doctor.
Interventions
The following options can be helpful for patients to rehabilitate after their fracture :
- Joints mobilization
- compression bandage
- Soft tissue massage
- Exercises and Activity modification
- Forearm taping
- Forearm bracing
Postoperative Rehabilitation [9]
- Complex Humerus fracture warrant individualized immobilization and rehabilitation strategies.
- Similarly, the addition of a thumb spica cast or orthosis with positioning of the wrist in slight ulnar deviation for management of a comminuted radial column fracture may prevent loss of reduction. *Because most multifragmentary Humerus fracture are the result of high-energy injuries, a prolonged period of wrist immobilization and soft-tissue rest may be beneficial and has not been shown to affect clinical outcomes.
- The wrist is typically immobilized for 2 weeks post-operatively in a sugar tong splint with neutral forearm rotation.
- At 6 weeks post-operatively, the wrist is placed into a removable orthosis, and active and passive range of motion (ROM) is initiated.
- Full weight bearing commences at approximately 3 months post-operatively after consolidation of the fracture is noted on radiographs.
- The presence of varying degrees of hand, wrist, and elbow stiffness is inevitable and may result from poor pain control, lack of effort in controlled mobilization, edema, concomitant ipsilateral upper extremity fractures, or peripheral nerve injuries.
- Early stretching and mobilization of the intrinsic and extrinsic tendons of the hand is important to prevent finger stiffness.
- Edema control can be initiated with compression gloves, digital massage, and active and passive ROM of the hand.
- A home exercise program or outpatient occupational therapy is started immediately post-operatively to maintain full range of motion of the hand and limit the development of intrinsic muscle tightness
Primary Prevention[10]
There are various preventive options to reduce the incidence of the Humerus fracture
- Using forearm and wrist guards during practicing sports (skating, biking)
- Using forearm and wrist guards during driving motorbikes
- Avoid falls in elderly individuals
- Prevention and/or treatment of osteoporosis
- Healthy diet
Secondary Prevention
It should be noted that the Post-menopausal women specially older than the age of 65 are at the higher risk of osteoporosis consequently these type of patients at greater risk for the pathological fractures .
So the Calcium and vitamin D supplementation play important role in increasing the bone mineral density (BMD) consequently decrease the risk of fracture in these type of patients. Also, avoiding excessive alcohol and quitting smoking play important role in this regard.
Detecting osteoporosis
- DEXA(dual-energy x-ray absorptiometry) scan
- Serum calcium and vitamin D levels
- Ultrasonography of the calcaneus
Pharmacological therapy
- The primary goal for the treatment of osteoporosis is to reduce longtime fracture risk in patients. Increasing bone mineral density (BMD) in response to the treatment is far less important than improvement of clinical aspects of osteoporosis, i.e., osteoporoticfracture. Therefore, most of the drugs efficacy is measured by the extent they improve the fracture risk instead of increasing BMD.
- During the treatment, if a single fracture happens, it does not necessarily indicate treatment failure or the need to be started on an alternative treatment or patient referral to a specialist.
- Calcium and vitamin D supplementation have been found to be effective in reducing the long term fracture risk, significantly. In order to suggest the people to use vitamin D and calcium supplements, the physician needs to make sure that patient is not able to obtain the nutrients through the daily intake. The available supplemental ions of calcium include calcium carbonate, calcium citrate, and vitamin D3 in various dosage forms.
Life style modifications[2]
- Exercise: Exercise promotes the mineralization of bone and bone accumulation particularly during growth. High impact exercise, in particular, has been shown to prevent the development of osteoporosis. However, it can have a negative effect on bone mineralization in cases of poor nutrition, such as anorexia nervosa and celiac disease.
- Nutrition: A diet high in calcium and vitamin D prevents bone loss. Patients at risk for osteoporosis, such as persons with chronic steroid use are generally treated with vitamin D and calcium supplementation. In renal disease, more active forms of vitamin D, such as 1,25-dihydroxycholecalciferol or calcitriol are used; as the kidney cannot adequately generate calcitriol from calcidiol (25-hydroxycholecalciferol), which is the storage form of vitamin D.
- By quitting smoking, osteoporosis as well as other diseases can be prevented.
- Avoiding excessive alcohol intake or drinking only in moderation.
See also
- Proximal humerus fracture
- Jupiter and Mehne Classification
- Riseborough_and_Radin_classification
- Gartland_classification
- Distal humerus fracture
- Humeral_shaft_fracture
- Humerus fracture
References
- ↑ Eglseder WA, Paryavi E (Summer 2017). "Intercondylar Fractures of the Distal Humerus in Patients Younger Than 20 Years: Capsulectomy Results". J Surg Orthop Adv. 26 (2): 98–101. PMID 28644121.
- ↑ 2.0 2.1 Pollock JW, Faber KJ, Athwal GS (April 2008). "Distal humerus fractures". Orthop. Clin. North Am. 39 (2): 187–200, vi. doi:10.1016/j.ocl.2007.12.002. PMID 18374809.
- ↑ Beeres FJ, Oehme F, Babst R (April 2017). "[Distal humerus fracture-extensile approaches]". Oper Orthop Traumatol (in German). 29 (2): 115–124. doi:10.1007/s00064-016-0474-4. PMID 27921119.
- ↑ Abzug J, Ho CA, Ritzman TF, Brighton B (2016). "Transphyseal Distal Humerus Fracture". Instr Course Lect. 65: 379–84. PMID 27049206.
- ↑ 5.0 5.1 Atalar AC, Tunalı O, Erşen A, Kapıcıoğlu M, Sağlam Y, Demirhan MS (January 2017). "Biomechanical comparison of orthogonal versus parallel double plating systems in intraarticular distal humerus fractures". Acta Orthop Traumatol Turc. 51 (1): 23–28. doi:10.1016/j.aott.2016.11.001. PMC 6197297. PMID 27965047.
- ↑ Pidhorz L, Alligand-Perrin P, De Keating E, Fabre T, Mansat P (December 2013). "Distal humerus fracture in the elderly: does conservative treatment still have a role?". Orthop Traumatol Surg Res. 99 (8): 903–7. doi:10.1016/j.otsr.2013.10.001. PMID 24184203.
- ↑ Ring D, Jawa A, Cannada L (February 2016). "Clinical Faceoff: Are Distal-third Diaphyseal Humerus Fractures Best Treated Nonoperatively?". Clin. Orthop. Relat. Res. 474 (2): 310–4. doi:10.1007/s11999-015-4636-8. PMC 4709285. PMID 26584799.
- ↑ Kozánek M, Bartoníček J, Chase SM, Jupiter JB (December 2014). "Treatment of distal humerus fractures in adults: a historical perspective". J Hand Surg Am. 39 (12): 2481–5. doi:10.1016/j.jhsa.2014.08.003. PMID 25442772.
- ↑ Ayoub MA, Khalil AE, Seleem OA (March 2016). "Distal humerus fractures nonunion with elbow stiffness in working adults: Can triple tension band technique and Lambda Plate(®) be a standby solution?". J Orthop Sci. 21 (2): 147–53. doi:10.1016/j.jos.2015.12.014. PMID 26778627.
- ↑ Sela Y, Baratz ME (March 2015). "Distal humerus fractures in the elderly population". J Hand Surg Am. 40 (3): 599–601. doi:10.1016/j.jhsa.2014.12.011. PMID 25661293.
|
WikiDoc Resources for Avulsion fracture |
|
Articles |
|---|
|
Most recent articles on Avulsion fracture Most cited articles on Avulsion fracture |
|
Media |
|
Powerpoint slides on Avulsion fracture |
|
Evidence Based Medicine |
|
Cochrane Collaboration on Avulsion fracture |
|
Clinical Trials |
|
Ongoing Trials on Avulsion fracture at Clinical Trials.gov Trial results on Avulsion fracture Clinical Trials on Avulsion fracture at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Avulsion fracture NICE Guidance on Avulsion fracture
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Avulsion fracture Discussion groups on Avulsion fracture Patient Handouts on Avulsion fracture Directions to Hospitals Treating Avulsion fracture Risk calculators and risk factors for Avulsion fracture
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Avulsion fracture |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [2]
Overview
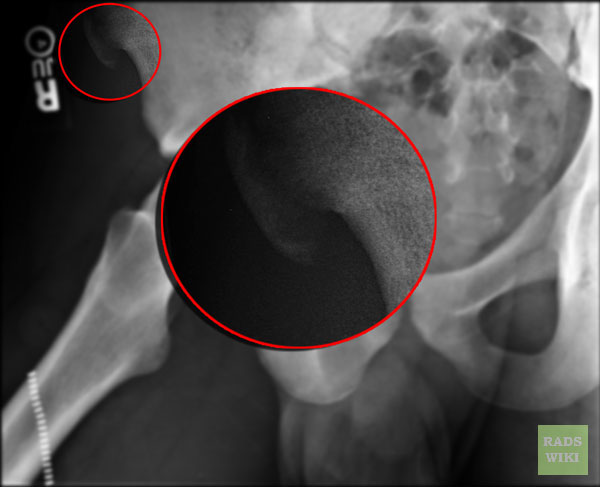
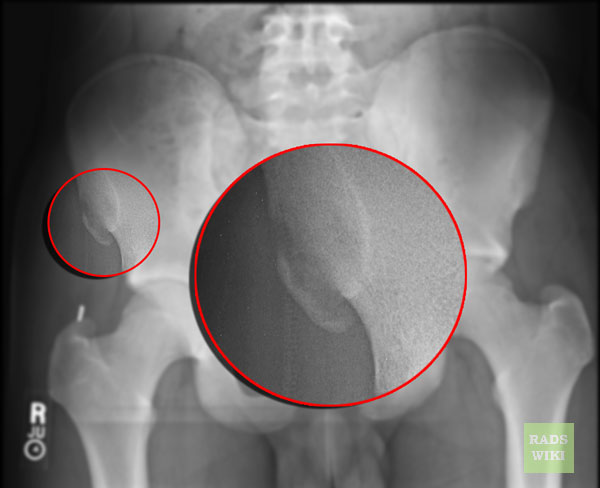
An avulsion fracture is a bone fracture which occurs when a fragment of bone tears away from the main mass of bone as a result of physical trauma. This can occur at the ligament due to the application forces external to the body (such as a fall or pull) or at the tendon due to a muscular contraction that is stronger than the forces holding the bone together. Generally muscular avulsion is prevented due to the neurological limitations placed on muscle contractions. Highly trained athletes can overcome this neurological inhibition of strength and produce a much greater force output capable of breaking or avulsing a bone.
If the fracture is small, it is usually sufficient to treat with rest and support bandage, but in more severe cases surgery may be required. Ice may be used to relieve swelling.
-
Schematic diagram of an avulsion fracture
-
Avulsion fracture off lunate bone
Avulsion fracture of anterior superior iliac spine