Ascariasis: Difference between revisions
| Line 231: | Line 231: | ||
<br clear="left"/> | <br clear="left"/> | ||
[[Image:Ascariasis case 004.jpg|left|thumb|400px| ]] | [[Image:Ascariasis case 004.jpg|left|thumb|400px|This is a higher-power photomicrograph of another ascarid egg. ]] | ||
<br clear="left"/> | <br clear="left"/> | ||
Revision as of 05:35, 22 February 2009
Template:DiseaseDisorder infobox
|
WikiDoc Resources for Ascariasis |
|
Articles |
|---|
|
Most recent articles on Ascariasis |
|
Media |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Ascariasis at Clinical Trials.gov Clinical Trials on Ascariasis at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Ascariasis
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Ascariasis Discussion groups on Ascariasis Patient Handouts on Ascariasis Directions to Hospitals Treating Ascariasis Risk calculators and risk factors for Ascariasis
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Ascariasis |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Assistant Editor-In-Chief: Dr. Imtiaz Ahmed Wani
Please Take Over This Page and Apply to be Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [2] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Overview
Ascariasis is a human disease caused by the parasitic roundworm Ascaris lumbricoides. Perhaps as many as one quarter of the world's people are infected[3], and ascariasis is particularly prevalent in tropical regions and in areas of poor hygiene. Other species of the genus Ascaris are parasitic and can cause disease in domestic animals.
Infection occurs through ingestion of food contaminated with feces containing Ascaris eggs. The larvae hatch, burrow through the intestine, reach the lungs, and finally migrate up the respiratory tract. From there they are then reswallowed and mature in the intestine, growing up to 30 cm (12 in.) in length and anchoring themselves to the intestinal wall.
Infections are usually asymptomatic, especially if the number of worms is small. They may however be accompanied by inflammation, fever, and diarrhea, and serious problems may develop if the worms migrate to other parts of the body.
Most people have no symptoms that are noticeable, but infection may cause slower growth and slower weight gain. If heavily infected, patients may have abdominal pain. Sometimes, while the immature worms migrate through the lungs, patients may cough and have difficulty breathing. Due to very heavy worm infection, intestines may become blocked.
Prevalence
Roughly 1.5 billion individuals are infected with this worm, primarily in Africa and Asia.[4] Ascariasis is endemic in the United States including Gulf Coast; in Nigeria and in Southeast Asia. One study indicated that the prevalence of ascariasis in the United States at about 4 million (2%) [8]. In a survey of a rural Nova Scotia community, 28.1% of 431 individuals tested were positive for Ascaris, all of them being under age 20, while all 276 tested in metropolitan Halifax were negative[5].
Deposition of ova (eggs) in sewage hints at the degree of ascariasis incidence. A 1978 study showed about 75% of all sewage sludge samples sampled in United States urban catchments contained Ascaris ova, with rates as high as 5 to 100 eggs per litre. In Frankfort, Indiana, 87.5% of the sludge samples were positive with Ascaris, Toxocara, Trichuris, and hookworm. In Macon, Georgia, one of the 13 soil samples tested positive for Ascaris. Municipal wastewater in Riyadh, Saudi Arabia detected over 100 eggs per litre of wastewater [6] and in Czechoslovakia was as high as 240-1050 eggs per litre [7].
Ascariasis can often be measured by examining food for ova. In one field study in Marrakech, Morocco, where raw sewage is used to fertilize crop fields, Ascaris eggs were detected at the rate of 0.18 eggs/kg in potatoes, 0.27 eggs/kg in turnip, 4.63 eggs/kg in mint, 0.7 eggs/kg in carrots, and 1.64 eggs/kg in radish[8]. A similar study in the same area showed that 73% of children working on these farms were infected with helminths, particularly Ascaris, probably as a result of exposure to the raw sewage.
Life cycle
First appearance of eggs in stools is 60-70 days. In larval ascariasis, symptoms occur 4-16 days after infection. The final symptoms are gastrointestinal discomfort, colic and vomiting, fever; observation of live worms in stools. Some patients may have pulmonary symptoms or neurological disorders during migration of the larvae. However there are generally few or no symptoms. A bolus of worms may obstruct the intestine; migrating larvae may cause pneumonitis and eosinophilia.
Source
The source of transmission is from soil and vegetation on which fecal matter containing eggs has been deposited. Ingestion of infective eggs from soil contaminated with human feces or transmission and contaminated vegetables and water is the primary route of infection. Intimate contact with pets which have been in contact with contaminated soil may result in infection, while pets which are infested themselves by a different type of roundworm can cause infection with that type of worm (Toxocara canis, etc) as occasionally occurs with groomers.
Transmission also comes through municipal recycling of wastewater into crop fields. This is quite common in emerging industrial economies, and poses serious risks for not only local crop sales but also exports of contaminated vegetables. A 1986 outbreak of ascariasis in Italy was traced to irresponsible wastewater recycling used to grow Balkan vegetable exports.
Transmission from human to human by direct contact is impossible. [9]
History and Symptoms
Patients can remain asymptomatic for very long periods of time. As larval stages travel through the body, they may cause visceral damage, peritonitis and inflammation, enlargement of the liver or spleen, toxicity, and pneumonia. A heavy worm infestation may cause nutritional deficiency; other complications, sometimes fatal, include obstruction of the bowel by a bolus of worms (observed particularly in children) and obstruction of the bile or pancreatic duct. More than 796 Ascaris lumbricoides worms weighing 550 g [19 ounces] were recovered at autopsy from a 2-year-old South African girl. The worms had caused torsion and gangrene of the ileum, which was interpreted as the cause of death[10].
Ascaris takes most of its nutrients from the partially digested host food in the intestine. There is limited evidence that it can also pierce the intestinal mucous membrane and feed on blood, but this is not its usual source of nutrition.[11] As a result, Ascaris infection does not produce the anemia associated with some other roundworm infections.
Diagnosis
The diagnosis is usually incidental when the host passes a worm in the stool or vomit. Stool samples for ova and parasites will demonstrate Ascaris eggs. Larvae may be found in gastric or respiratory secretions in pulmonary disease. Blood counts may demonstrate peripheral eosinophilia. On X-ray, 15-35 cm long filling defects, sometimes with whirled appearance (bolus of worms).
Diagnostic Findings
Microscopic identification of eggs in the stool is the most common method for diagnosing intestinal ascariasis. The recommended procedure is as follows:
- Collect a stool specimen.
- Fix the specimen in 10% formalin.
- Concentrate using the formalin–ethyl acetate sedimentation technique.
- Examine a wet mount of the sediment.
Where concentration procedures are not available, a direct wet mount examination of the specimen is adequate for detecting moderate to heavy infections. For quantitative assessments of infection, various methods such as the Kato-Katz can be used. Larvae can be identified in sputum or gastric aspirate during the pulmonary migration phase (examine formalin-fixed organisms for morphology). Adult worms are occasionally passed in the stool or through the mouth or nose and are recognizable by their macroscopic characteristics.
Ultrasound
(Images courtesy of Dr. Imtiaz Ahmed Wani)
Macroscopic Findings
(Images courtesy of Dr. Imtiaz Ahmed Wani)
-
Enterotomy for worm removal
-
Ascaris lumbricoides caused gangrene of ileum (shown worms removed from a child)
Microscopic Findings
Below are several Ascaris eggs seen in wet mounts. Diagnostic characteristics:
Fertilized eggs (A, B on the right, D, F, G, H) are rounded, have a thick shell, with an external mammillated layer that is often stained brown by bile. In some cases, the outer layer is absent (decorticated eggs: E, F on the right, G). Size: approximately 60 µm in diameter when spherical, and up to 75 µm when ovoid.
Unfertilized eggs (B on the left, C, E) are elongated and larger (up to 90 µm in length); their shell is thinner; and their mammillated layer is more variable, either with large protuberances (C) or practically none (E); these eggs contain mainly a mass of refractile granules.
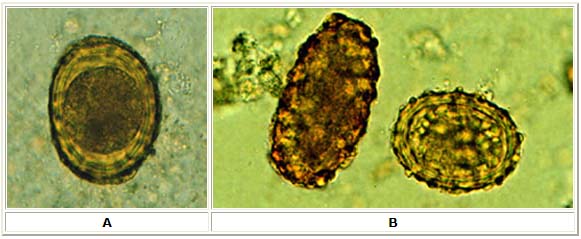
A: Fertilized Ascaris egg, still at the unicellular stage. Eggs are normally at this stage when passed in the stool. Complete development of the larva requires 18 days under favorable conditions.
B: Unfertilized and fertilized eggs (left and right, respectively).
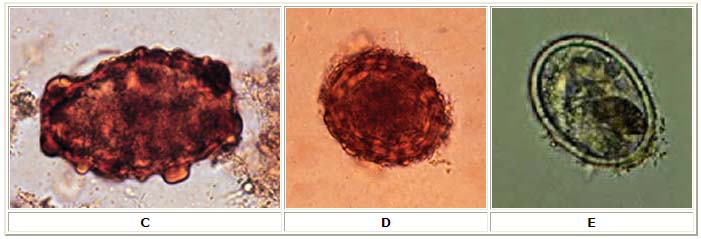
C: Unfertilized egg. Prominent mammillations of outer layer.
D: Fertilized egg. The embryo can be distinguished inside the egg.
E: Unfertilized egg with no outer mammillated layer (decorticated).

F: Three fertilized eggs (one decorticated, on the right) of Ascaris lumbricoides.
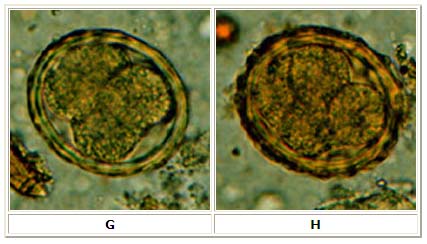
G, H: Two fertilized eggs from the same patient, where embryos have begun to develop (this happens when the stool sample is not processed for several days without refrigeration). The embryos in early stage of division (4 to 6 cells) can be clearly seen. Note that the egg in G has a very thin mammillated outer layer.

I: Egg containing a larva, which will be infective if ingested.
J: Larva hatching from an egg.
Treatment
Pharmaceutical treatments include:
- Mebendazole (Vermox) (C16H13N3O2). Causes slow immobilization and death of the worms by selectively and irreversibly blocking uptake of glucose and other nutrients in susceptible adult intestine where helminths dwell. Oral dosage is 100 mg 12 hourly for 3 days.
- Piperazine (C4H10N2.C6H10O4). A flaccid paralyzing agent that causes a blocking response of ascaris muscle to acetylcholine. The narcotizing effect immobilizes the worm, which prevents migration when treatment is accomplished with weak drugs such as thiabendazole. If used by itself it causes the worm to be passed out in the feces. Dosage is 75 mg/kg (max 3.5 g) as a single oral dose.
- Pyrantel pamoate (Antiminth, Pin-Rid, Pin-X) (C11H14N2S.C23H16O6) Depolarizes ganglionic block of nicotinic neuromuscular transmission, resulting in spastic paralysis of the worm. Spastic (tetanic) paralyzing agents, in particular pyrantel pamoate, may induce complete intestinal obstruction in a heavy worm load. Dosage is 11 mg/kg not to exceed 1 g as a single dose.
- Albendazole (C12H15N3O2S) A broad-spectrum antihelminthic agent that decreases ATP production in the worm, causing energy depletion, immobilization, and finally death. Dosage is 400 mg given as single oral dose (contraindicated during pregnancy and children under 2 years).
- Thiabendazole. This may cause migration of the worm into the esophagus, so it is usually combined with piperazine.
- Hexylresorcinol effective in single dose, mentioned in : Holt, Jr Emmett L, McIntosh Rustin: Holt's Diseases of Infancy and Childhood: A Textbook for the Use of Students and Practitioners. Appleton and Co, New York,11th edition
- Santonin, more toxic than hexylresorcinol, mentioned in : Holt, Jr Emmett L, McIntosh Rustin: Holt's Diseases of Infancy and Childhood: A Textbook for the Use of Students and Practitioners. Appleton and Co, New York,, 11th edition
- Oil of Chenopodium, more toxic than hexylresorcinol, mentioned in : Holt, Jr Emmett L, McIntosh Rustin: Holt's Diseases of Infancy and Childhood: A Textbook for the Use of Students and Practitioners. Appleton and Co, New York, 11th edition
Also, corticosteroids can treat some of the symptoms, such as inflammation.
Native Americans have traditionally used epazote (Chenopodium ambrisioides) for treatment, which was not as powerful as pharmaceutical compounds, but spontaneous passage of Ascarids provided some proof of efficacy.
Some recent studies exist in the medical literature suggesting that sun-dried papaya and watermelon seeds may reduce infections by a large factor. The adult dosage is one tablespoon of the seed powder in a glass of sugar water once a week for two weeks. The sugar makes the bitter taste palatable and acts as a laxative.
Prevention
Prevention includes; use of toilet facilities; safe excreta disposal; protection of food from dirt and soil; thorough washing of produce; and hand washing.
Food dropped on the floor should never be eaten without washing or cooking, particularly in endemic areas. Vegetables originating from third-world countries should always be washed thoroughly before consumption.
Animal models for Ascaris infestation
There are two animal models for studying Ascaris infection:
- Mouse-Ascaris suum test model. (Howes HL Jr. J Parasitol. 1971 Jun; 57(3): 487-93.)
- Ascaris suum in experimentally infected pigs. (Lichtensteiger CA et al; 1999)
Trivia
- Ascariasis may result in allergies to shrimp and dustmites due to the shared antigen, tropomyosin.
- Ascaris have an aversion to some general anesthetics and may exit the body, sometimes through the mouth. [12]
| Genus and Species | Ascaris lumbricoides |
|---|---|
| Common Name | Giant Intestinal Roundworm |
| Etiologic Agent of: | Ascariasis |
| Infective stage | Embryonated Egg |
| Definitive Host | Man |
| Portal of Entry | Mouth |
| Mode of Transmission | Ingestion of Embryonated egg through contaminated food or water |
| Habitat | Small Intestine |
| Pathogenic Stage | Adult Larva |
| Mode of Attachment | Retention in the mucosal folds using pressure |
| Mode of Nutrition | Feeding of Chyme |
| Pathogenesis | Larva – pneumonitis, Loeffler’s syndrome;
Adult – Obstruction, Liver abscess, Appendicitis. With Blood-Lung Phase along with Hookworms and Strongyloides stercoralis. |
| Laboratory diagnosis | Concentration methods and Direct Fecal Smear: Kato-Katz |
| Treatment | Albendazole, Mebendazole, or Pyrantel Pamoate |
| Diagnostic Feature - Adult | Female - prominent genital girdle |
| Diagnostic Feature - Egg | Coarse mammilated albuminous coating |
Case Examples
Case #1
Clinical Summary
Shortly after arriving home after two years in Peru with the Peace Corps this 27-year-old female presented to the emergency room with a fever of 103.5°, anterior cervical lymphadenopathy, and pharyngitis. A rapid Strep test was positive and she was treated with penicillin.
Two days later she returned to the emergency room with abdominal distension, paroxysmal periumbilical pain, and repeated emesis. On examination, there was diffuse abdominal tenderness and bowel sounds were hyperactive and high-pitched. The WBC count was unremarkable except for a 12% eosinophilia. An upright film of the abdomen revealed dilated loops of small bowel with air fluid levels and the absence of colonic gas. Surgical exploration confirmed the presumptive diagnosis of small bowel obstruction and identified a tangled mass of approximately 50 adult Ascaris lumbricoides worms as the cause.
One-week post surgery, stool examination revealed the continued presence of Ascaris ova, as well as cysts of Entamoeba histolytica and Giardia lamblia. The patient was treated with appropriate anthelmintics and made a complete recovery.
Histopathological Findings







References
- ^ How much human helminthiasis is there in the world?, 1999. D. Crompton, J of Parasitology 85(3): 397-403.
- ^ Prevalence of Ascaris lumbricoides infection in a small Nova Scotian community, 1984. J. Embil, L. Pereira, F. White, J. Garner, F. Manuel, Am J Trop Med Hyg, 33, 595-8.
- ^ Risk of contamination of human and agricultural environment with parasites through reuse of treated municipal wastewater in Riyadh, Saudi Arabia, 1992. A. Bolbol. J Hyg Epidemiol Microbiol Immunol, 36, 330-7.
- ^ Helminth eggs in the sludge from three sewage treatment plants in Czechoslovakia, 1992. Horak. Folia Parasitol, 39, 153-7.
- ^ Helminthic infections associated with the use of raw wastewater for agricultural purposes in Beni Mellal, Morocco, 1999. K. Habbari, A. Tifnouti, G. Bitton and A. Mandil, Eastern Mediterranean Health Journal, Volume 5, Issue 5, 1999, Page 912-921
- ^ Fatal human ascariasis following secondary massive infection, 1986. Baird JK, Mistrey M, Pimsler M, Connor DH. Am J Trop Med Hyg 1986 Mar;35(2):314-8, PMID 3953945, UI: 86156463
- ^ Ascariasis and sewage in Europe, 1986. Pawlowski ZS, Schultzberg K., in: Block JC, ed. Epidemiological studies of risks associated with agricultural use of sewage sludge: knowledge and needs. London, Elsevier, 1986:83-93.
- ^ http://en.wikipedia.org/w/index.php?title=Ascariasis&action=edit§ion=10
See also
External links
- Video of removal of Ascari lumbricoides with an endoscope
- Images (warning, very graphic): [13], [14]
- CDC DPDx Parasitology Diagnostic Web Site
Template:Helminthiases
Template:SIB
de:Spulwurm hu:Orsóférgek io:Askaridiko id:Askariasis it:Ascaridiasi nl:Spoelworm ps:اسکاريس لومبريکويډېس sk:Hlísta detská



