Secondary hyperparathyroidism
| Secondary hyperparathyroidism | |
 | |
|---|---|
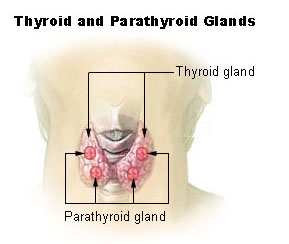
| Thyroid and parathyroid. | |
| ICD-10 | E21.1 |
| ICD-9 | 252.02, 588.81 |
| DiseasesDB | 6301 |
| MeSH | D006962 |
For patient information click here Template:Secondary hyperparathyroidism Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Phone:617-632-7753
Overview
Secondary hyperparathyroidism refers to the excessive secretion of parathyroid hormone (PTH) by the parathyroid glands in response to hypocalcemia (low blood calcium levels) and associated hypertrophy of the glands. This disorder is especially seen in patients with chronic renal failure. It is often--although not consistently--abbreviated as SHPT in medical literature.
Signs and Symptoms
Bone and joint pain are common, as are limb deformities. The elevated PTH has also pleiotropic effects on blood, immune system and neurological system.
Diagnosis
The PTH is elevated due to a low serum (ionized) calcium.
Causes
Chronic renal failure is the most common causes of secondary hyperparathyroidism. Failing kidneys do not convert enough vitamin D to its active form, and they do not adequately excrete phosphorus. When this happens, insoluble calcium phosphate forms in the body and removes calcium from the circulation. Both processes leads to hypocalcemia and hence secondary hyperparathyroidism.
Treatment
If the underlying cause of the hypocalcemia can be addressed, the hyperparathyroidism will resolve. In patients with chronic renal failure treatment consists of dietary restriction of phosphorus, supplements with the active form of vitamin D, and phosphate binders.
Prognosis
If left untreated, the disease will progress to tertiary hyperparathyroidism, where correction of the underlying cause will not stop excess PTH secretion, i.e. parathyroid gland hypertrophy becomes irreversible.