Astrocytoma pathophysiology
|
Astrocytoma Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Study |
|
Astrocytoma pathophysiology On the Web |
|
American Roentgen Ray Society Images of Astrocytoma pathophysiology |
|
Risk calculators and risk factors for Astrocytoma pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1];Associate Editor(s)-in-Chief: Shivali Marketkar, M.B.B.S. [2]
Pathophysiology
Overview
Well-differentiated astrocytomas constitute about 25 to 30% of cerebral gliomas. They have a predilection for the cerebrum, cerebellum, hypothalamus, pons, and optic nerve and chiasm. Although astrocytomas have many different histological characteristics, the most common type is the well-differentiated fibrillary astrocytoma. These tumors express glial fibrillary acidic protein (GFAP), which possibly functions as a tumor suppressor[1], and is a useful diagnostic marker in a tissue biopsy. [2]
Grading
Astrocytomas have great variation in their presentation. The World Health Organization acknowledges the following grading system for astrocytomas:
- Grade 1 — pilocytic astrocytoma - primarily pediatric tumor, with median age at diagnosis of 12
- Grade 2 — diffuse astrocytoma
- Grade 3 — anaplastic (malignant) astrocytoma
- Grade 4 — glioblastoma multiforme (most common)
In addition to these four tumor grades, astrocytomas may combine with oligodendrocytes to produce oligoastrocytoma. Unique astrocytoma variants have also been known to exist.
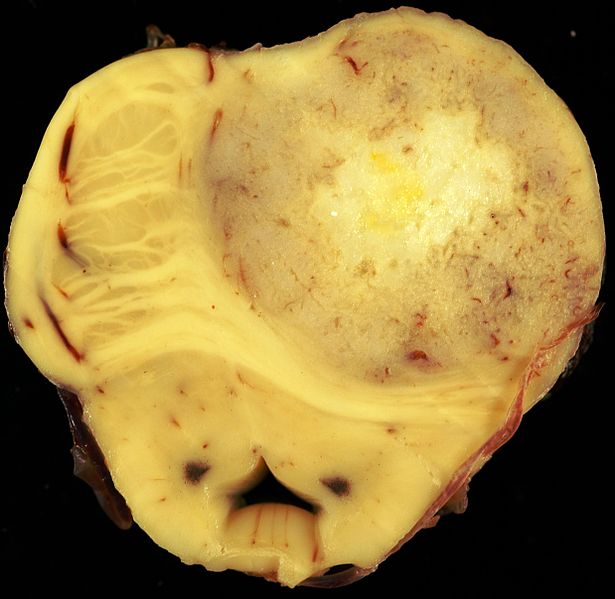
Gross Pathology
Microscopic Pathology
Histologic diagnosis with tissue biopsy will normally reveal an infiltrative character suggestive of the slow growing nature of the tumor. The tumor may be cavitating, pseudocyst-forming, or noncavitating. Appearance is usually white-gray, firm, and almost indistinguishable from normal white matter.
The WHO has given a four point scale depending on the histologic grade of the tumor (see below). This article focuses on the well-differentiated (Grade 2) astrocytoma and Anaplastic(grade 3) astrocytoma. For grade 1 and 4 astrocytomas, see respective article headings:
Video
{{#ev:youtube|O0b4zyDQcyI}}
References
- ↑ M Toda; et al. (1994). "Cell growth suppression of astrocytoma C6 cells by glial fibrillary acidic protein cDNA transfection". Journal of Neurochemistry. 63 (5): 1975–1978. PMID 7931355.
- ↑ JHN Deck; et al. (1978). "The role of glial fibrillary acidic protein in the diagnosis of central nervous system tumors". Acta Neuropathologica. Springer Berlin / Heidelberg. 42 (3): 183–190. doi:10.1007/BF00690355.