Wolfram syndrome
|
WikiDoc Resources for Wolfram syndrome |
|
Articles |
|---|
|
Most recent articles on Wolfram syndrome Most cited articles on Wolfram syndrome |
|
Media |
|
Powerpoint slides on Wolfram syndrome |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Wolfram syndrome at Clinical Trials.gov Trial results on Wolfram syndrome Clinical Trials on Wolfram syndrome at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Wolfram syndrome NICE Guidance on Wolfram syndrome
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Wolfram syndrome Discussion groups on Wolfram syndrome Patient Handouts on Wolfram syndrome Directions to Hospitals Treating Wolfram syndrome Risk calculators and risk factors for Wolfram syndrome
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Wolfram syndrome |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Jyostna Chouturi, M.B.B.S [2]
| Wolfram syndrome | |
| Classification and external resources | |

| |
|---|---|
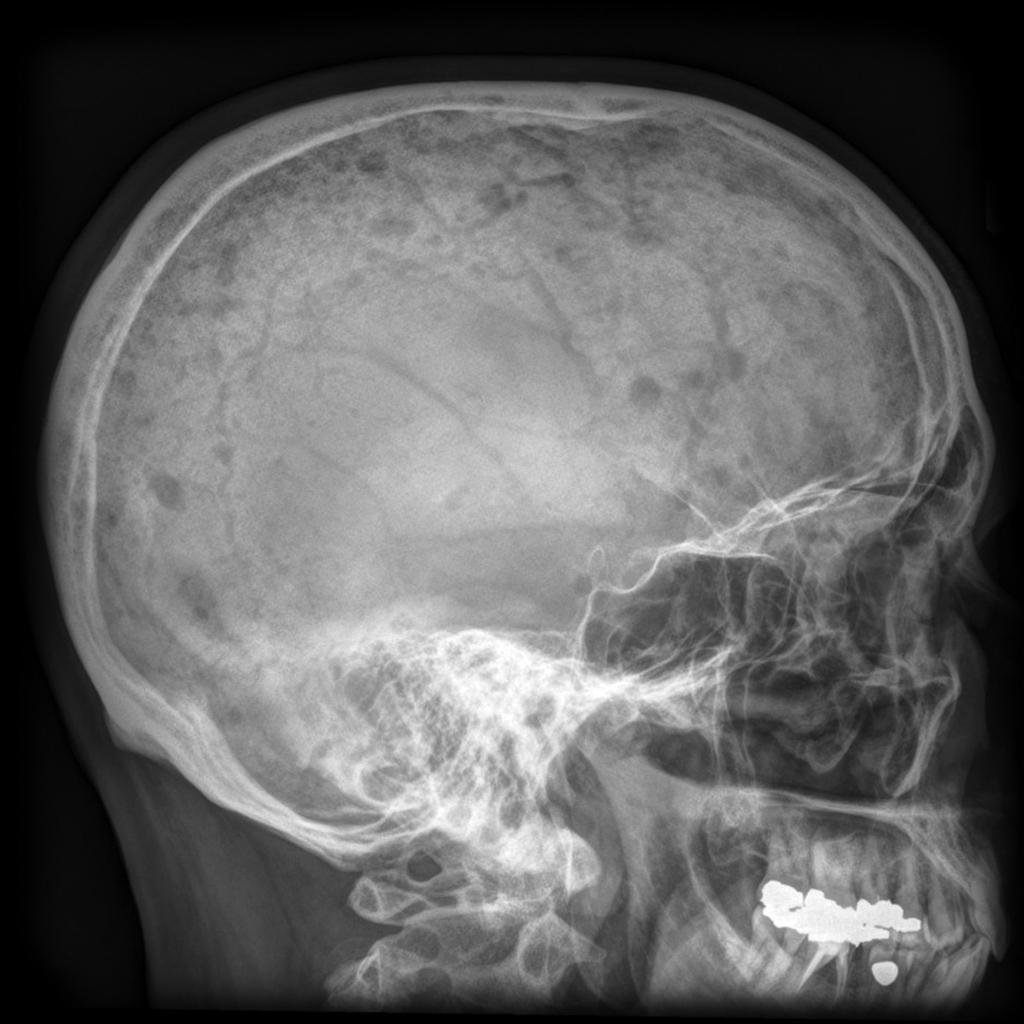
| Photographic image of the patient right eye showing optic atrophy without diabetic retinopathy Wolfram syndrome.jpg., 2009[1] |
Overview
Wolfram syndrome, also called DIDMOAD (diabetes insipidus, diabetes mellitus, optic atrophy, and deafness), is a rare genetic disorder, causing diabetes mellitus, optic atrophy, and deafness as well as various other possible disorders.
It was first described in four siblings in 1938 by Dr. Don J. Wolfram, M.D.[2][3] The disease affects the central nervous system (especially the brainstem).
Causes
Wolfram syndrome was initially thought to be caused by mitochondrial dysfunction due to its symptoms and several reports of mitochondrial mutations. However, it has now been established that Wolfram syndrome is caused by endoplasmic reticulum dysfunction.[4]
Two genetic forms have been described: Wolfram syndrome 1 (WFS1),[5] and Wolfram syndrome 2 (WFS2)[6]
WFS1
The WFS1 or wolframin gene[7] provides instructions for making the wolframin protein. The WFS1 gene is active in cells throughout the body, with strong activity in the heart, brain, lungs, inner ear, and pancreas. The pancreas provides enzymes that help digest food, and it also produces the hormone insulin. Insulin controls how much glucose (a type of sugar) is passed from the blood into cells for conversion to energy.
Within cells, wolframin is located in a structure called the endoplasmic reticulum. Among its many activities, the endoplasmic reticulum folds and modifies newly formed proteins so they have the correct 3-dimensional shape to function properly. The endoplasmic reticulum also helps transport proteins, fats, and other materials to specific sites within the cell or to the cell surface. The function of wolframin is unknown. Based on its location in the endoplasmic reticulum, however, it may play a role in protein folding or cellular transport. In the pancreas, wolframin may help fold a protein precursor of insulin (called proinsulin) into the mature hormone that controls blood glucose levels. Research findings also suggest that wolframin may help maintain the correct cellular level of charged calcium atoms (calcium ions) by controlling how much is stored in the endoplasmic reticulum. In the inner ear, wolframin may help maintain the proper levels of calcium ions or other charged particles that are essential for hearing.
More than 30 WFS1 mutations have been identified in individuals with a form of nonsyndromic deafness (hearing loss without related signs and symptoms affecting other parts of the body) called DFNA6. Individuals with DFNA6 deafness cannot hear low tones (low-frequency sounds), such as a tuba or the "m" in moon. DFNA6 hearing loss is unlike most forms of nonsyndromic deafness that affect high tones (high-frequency sounds), such as birds chirping, or all frequencies of sound. Most WFS1 mutations replace one of the protein building blocks (amino acids) used to make wolframin with an incorrect amino acid. One mutation deletes an amino acid from wolframin. WFS1 mutations probably alter the 3-dimensional shape of wolframin, which could affect its function. Because the function of wolframin is unknown, however, it is unclear how WFS1 mutations cause hearing loss. Some researchers suggest that altered wolframin disturbs the balance of charged particles in the inner ear, which interferes with the hearing process.
Other disorders - caused by mutations in the WFS1 gene
Mutations in the WFS1 gene cause Wolfram syndrome, which is also known by the acronym DIDMOAD. This syndrome is characterised by childhood-onset diabetes mellitus (DM), which results from the improper control of glucose due to the lack of insulin; a gradual loss of vision caused by optic atrophy (OA), in which the nerve that connects the eye to the brain wastes away; and deafness (D). This syndrome can sometimes cause diabetes insipidus (DI), a condition in which the kidneys cannot conserve water. Other complications that affect the bladder and nervous system may also occur.
Researchers have identified more than 100 WFS1 mutations that cause Wolfram syndrome. Some mutations delete or insert DNA from the WFS1 gene. As a result, little or no wolframin is present in cells. Other mutations replace one of the protein building blocks (amino acids) used to make wolframin with an incorrect amino acid. These mutations appear to reduce wolframin activity dramatically. Researchers suggest that the loss of wolframin disrupts the production of insulin, which leads to poor glucose control and diabetes mellitus. It is unclear how WFS1 mutations lead to other features of Wolfram syndrome.
WFS2
The dysfunction of the CISD2 gene can cause WFS2.[8]
Differential diagnosis
Wolfram syndrome must be differentiated from other causes of diabetes insipidus.
| Type of DI | Subclass | Disease | Defining signs and symptoms | Lab/Imaging findings |
|---|---|---|---|---|
| Central | Acquired | Histiocytosis |
|
 |
| Craniopharyngioma |
|
 | ||
| Sarcoidosis |
|
 | ||
| Congenital | Hydrocephalus |
|
Dilated ventricles on CT and MRI
 | |
| Wolfram Syndrome (DIDMOAD) |
| |||
| Nephrogenic | Acquired | Drug-induced (demeclocycline, lithium) |
| |
| Hypercalcemia |
| |||
| Hypokalemia |
| |||
| Multiple myeloma |
|
 | ||
| Sickle cell disease |
|
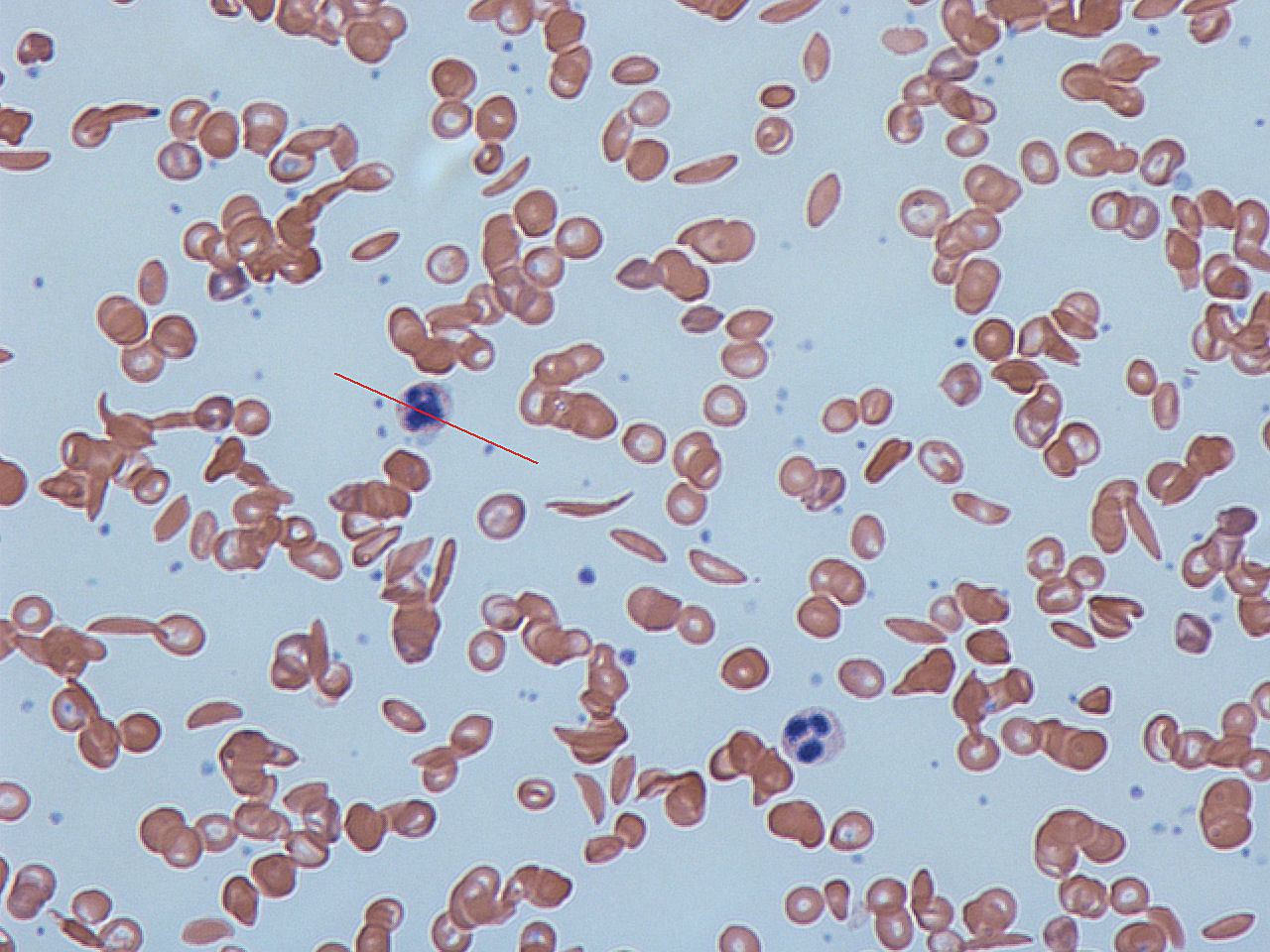 | ||
| Primary polydipsia | Psychogenic |
| ||
| Gestational diabetes insipidus |
| |||
| Diabetes mellitus |
| |||
Other differentials
Wolfram syndrome must be differentiated from other similar conditions which lead to multiple endocrine disorders such as autoimmune polyendocrine syndrome, POEMS syndrome, Hirata syndrome, Kearns–Sayre syndrome and Wolfram syndromes.[10][11][12][13][14]
| Disease | Addison's disease | Type 1 diabetes mellitus | Hypothyroidism | Other disorders present |
|---|---|---|---|---|
| APS type 1 | + | Less common | Less common | Hypoparathyroidism Candidiasis Hypogonadism |
| APS type 2 | + | + | + | Hypogonadism Malabsorption |
| APS type 3 | - | + | + | Malabsorption |
| Thymoma | + | - | + | Myasthenia gravis Cushing syndrome |
| Chromosomal abnormalities (Turner syndrome, Down's syndrome) |
- | + | + | Cardiac dysfunction |
| Kearns–Sayre syndrome | - | + | - | Myopathy Hypoparathyroidism Hypogonadism |
| Wolfram syndrome | - | + | - | Diabetes insipidus Optic atrophy Deafness |
| POEMS syndrome | - | + | - | Polyneuropathy Hypogonadism Plasma cell dyscrasias |
Treatment
There is no known direct treatment. Current treatment efforts focus on managing the complications of Wolfram syndrome, such as diabetes mellitus and diabetes insipidus.[15]
Prognosis
The first symptom is typically diabetes mellitus, which is usually diagnosed around the age of 6. The next symptom to appear is often optic atrophy, the wasting of optic nerves, around the age of 11. The first signs of this are loss of colour vision and peripheral vision. The condition worsens over time, and people with optic atrophy are usually blind within 8 years of the first symptoms.[16] Life expectancy of people suffering from this syndrome is about 30 years.
Research
Research for designing therapeutic trials is ongoing via the Washington University Wolfram Study Group, supported by The Jack and J.T. Snow Scientific Research Foundation for Wolfram research.
See also
References
- ↑ Manaviat MR, Rashidi M, Mohammadi SM (2009). "Wolfram Syndrome presenting with optic atrophy and diabetes mellitus: two case reports". Cases J. 2: 9355. doi:10.1186/1757-1626-2-9355. PMC 2804005. PMID 20062605.
- ↑ Wolfram, D. J.; Wagener, H. P. : Diabetes mellitus and simple optic atrophy among siblings: report of four cases. Mayo Clin. Proc. 13: 715-718, 1938.
- ↑ Woolling KR (July 1989). "Wolfram syndrome: a tribute to Don J. Wolfram, M.D.". Indiana Medicine. 82 (7): 548–9. PMID 2666507.
- ↑ Urano, F. Diabetes. 2014 Mar;63(3):844-6.
- ↑ OMIM 222300 (WFS1)
- ↑ OMIM 604928 (WFS2)
- ↑ OMIM 606201 (WFS1 gene)
- ↑ Role for CISD2 gene in human disease and lifespan control
- ↑ Ghosh KN, Bhattacharya A (1992). "Gonotrophic nature of Phlebotomus argentipes (Diptera: Psychodidae) in the laboratory". Rev Inst Med Trop Sao Paulo. 34 (2): 181–2. PMID 1340034.
- ↑ Sherer Y, Bardayan Y, Shoenfeld Y (1997). "Thymoma, thymic hyperplasia, thymectomy and autoimmune diseases (Review)". Int. J. Oncol. 10 (5): 939–43. PMID 21533467.
- ↑ Nozza, Andrea (2017). "POEMS SYNDROME: AN UPDATE". Mediterranean Journal of Hematology and Infectious Diseases. 9 (1): e2017051. doi:10.4084/mjhid.2017.051. ISSN 2035-3006.
- ↑ Maceluch JA, Niedziela M (2006). "The clinical diagnosis and molecular genetics of kearns-sayre syndrome: a complex mitochondrial encephalomyopathy". Pediatr Endocrinol Rev. 4 (2): 117–37. PMID 17342029.
- ↑ Rigoli L, Di Bella C (2012). "Wolfram syndrome 1 and Wolfram syndrome 2". Curr. Opin. Pediatr. 24 (4): 512–7. doi:10.1097/MOP.0b013e328354ccdf. PMID 22790102.
- ↑ Husebye, Eystein S.; Anderson, Mark S. (2010). "Autoimmune Polyendocrine Syndromes: Clues to Type 1 Diabetes Pathogenesis". Immunity. 32 (4): 479–487. doi:10.1016/j.immuni.2010.03.016. ISSN 1074-7613.
- ↑ Wolfram Syndrome
- ↑ http://ghr.nlm.nih.gov/condition/wolfram-syndrome. Missing or empty
|title=(help)
External links
- Ellie White Foundation for Rare Genetic Disorders
- The Jack and J.T. Snow Scientific Research Foundation
- Washington University in St. Louis Wolfram Study Group
- Combating Wolfram syndrome
| Wikimedia Commons has media related to Wolfram syndrome. |
- OMIM DIDMOAD search
- Genetics Home Reference WFS1
- [3] A child in the online comic Sandra and Woo discusses her life under Wolfram Syndrome