Von Hippel-Lindau disease
| Von Hippel-Lindau disease | ||
| ICD-10 | Q85.8 | |
|---|---|---|
| ICD-9 | 759.6 | |
| OMIM | 193300 | |
| DiseasesDB | 14000 | |
| eMedicine | ped/2417 oph/354 | |
| MeSH | C10.562.400 | |
Overview
Von Hippel-Lindau disease (VHL) is a rare inherited genetic condition involving the abnormal growth of tumors in parts of the body which are particularly rich in blood supply.
Features
Features of VHL are:
- angiomatosis - little knots of capillaries in the retina and various organs.
- hemangioblastomas - tumors of the central nervous system (CNS, especially the cerebellum, brain stem, and spinal cord).
- pheochromocytoma - tumors of the adrenal medulla that often produce catecholamines
- renal cell carcinoma - in some forms
- pancreas - cysts and tumors of the pancreas, which may be neuroendocrine tumors
Untreated, VHL may result in blindness and permanent brain damage; death is usually caused by complications of malignant tumors in the brain or kidney, cardiovascular disease secondary to pheochromocytoma. With early detection and appropriate treatment, there is more hope today for people with VHL than ever before.
Types
There are various subtypes:
- Type 1 (angiomatosis without pheochromocytoma)
- Type 2 (angiomatosis with pheochromocytoma)
- Type 2A (with renal cell carcinoma)
- Type 2B (without renal cell carcinoma)
- Type 2C (only pheochromocytoma and no angiomatosis or renal cell carcinoma)
Genetics
The disease is caused by mutations of the Von Hippel-Lindau tumor suppressor (VHL) gene on the short arm of third chromosome.
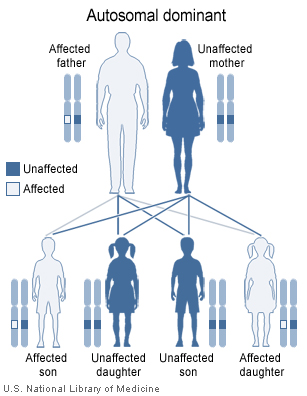
VHL is an autosomal dominant disorder, but there is a wide variation in the age of onset of the disease, the organ system affected and the severity of effect. Most people with von Hippel-Lindau syndrome inherit an altered copy of the gene from one parent. In about 20 percent of cases, however, the altered gene is the result of a new mutation that occurred during the formation of reproductive cells (eggs or sperm) or early in fetal development.
As long as one copy of the VHL gene is producing functional VHL protein in each cell, tumors do not form. If a mutation occurs in the second copy of the VHL gene during a person's lifetime, the cell will have no working copies of the gene and will produce no functional VHL protein. A lack of this protein allows tumors characteristic of von Hippel-Lindau syndrome to develop.
History
Eugen von Hippel described the angiomas in the eye in 1904.[1]. Arvid Lindau described the angiomas of the cerebellum and spine in 1927.[2]
In an article appearing in the Associated Press, it has been speculated by a Vanderbilt University endocrinologist that the hostility underlying the Hatfield-McCoy feud may have been partly due to the consequences of Von Hippel-Landau disease. The article suggests that the McCoy family was pre-disposed to bad tempers because many of them had a pheochomocytoma, which produced excess adrenaline and a tendency toward explosive tempers.[3] Pheochromocytomas produce surges of adrenaline which are more often perceived as panic attacks than rage attacks. Left untreated, they will cause serious cardiovascular disease, heart attack, and stroke. Only about 20% of people with VHL get pheochromocytomas.[4]
Nomenclature
Other names are: angiomatosis retinae, angiophakomatosis retinae et cerebelli, familial cerebello-retinal angiomatosis, cerebelloretinal hemangioblastomatosis, Hippel Disease, Hippel-Lindau syndrome, HLS, Lindau disease or retinocerebellar angiomatosis.
DIfferentiating Von Hippel-Lindau disease from other diseases
| Disease | Gene | Chromosome | Differentiating Features | Components of MEN | Diagnosis | ||
|---|---|---|---|---|---|---|---|
| Parathyroid | Pitutary | Pancreas | |||||
| von Hippel-Lindau syndrome | Von Hippel–Lindau tumor suppressor | 3p25.3 |
|
- | - | + |
|
| Carney complex | PRKAR1A | 17q23-q24 |
|
- | - | - |
|
| Neurofibromatosis type 1 | RAS | 17 | - | - | - | Prenatal
Postnatal Cardinal Clinical Features" are required for positive diagnosis.
| |
| Li-Fraumeni syndrome | TP53 | 17 | Early onset of diverse amount of cancers such as | - | - | - |
Criteria
|
| Gardner's syndrome | APC | 5q21 |
|
- | - | - |
|
| Multiple endocrine neoplasia type 2 | RET | - |
|
+ | - | - |
Criteria Two or more specific endocrine tumors
|
| Cowden syndrome | PTEN | - | Hamartomas | - | - | - |
|
| Acromegaly/gigantism | - | - |
|
- | + | - |
|
| Pituitary adenoma | - | - |
|
- | + | - |
|
| Hyperparathyroidism | - | - | - | + | - | - |
|
| Pheochromocytoma/paraganglioma |
VHL RET NF1 SDHB SDHD |
- | Characterized by | - | - | - |
|
| Adrenocortical carcinoma |
|
17p, 13q |
|
- | - | - |
|
| Adapted from Toledo SP, Lourenço DM, Toledo RA. A differential diagnosis of inherited endocrine tumors and their tumor counterparts, journal=Clinics (Sao Paulo), volume= 68, issue= 7, 07/24/2013[5] | |||||||
See also
References
- ↑ Von Hippel E. Ueber eine sehr seltene Erkrankung der Netzhaut. Albrecht von Graefes Arch Ophthal 1904;59:83-106.
- ↑ Lindau A. Zur Frage der Angiomatosis Retinae und Ihrer Hirncomplikation. Acta Ophthal 1927;4:193-226.
- ↑ "Hatfield-McCoy feud blamed on 'rage' disease". MSNBC.com. 2007-04-05. Retrieved 2007-04-05. Check date values in:
|date=(help) - ↑ "'Pheochromocytoma Information'". vhl.org. 2007-04-05. Retrieved 2007-04-05. Check date values in:
|date=(help) - ↑ Toledo SP, Lourenço DM, Toledo RA (2013). "A differential diagnosis of inherited endocrine tumors and their tumor counterparts". Clinics (Sao Paulo). 68 (7): 1039–56. doi:10.6061/clinics/2013(07)24. PMC 3715026. PMID 23917672.
External links
- Clinical Description of VHL
- The VHL Handbook
- Template:NINDS
- Von Hippel-Lindau syndrome at NLM Genetics Home Reference
- Template:Chorus
- Template:WhoNamedIt
- Online Mendelian Inheritance in Man (OMIM) 608537 (VHL gene)
Template:Phakomatoses and other congenital malformations not elsewhere classified
da:Von Hippel-Lindaus sygdom de:Morbus Hippel-Lindau nl:Ziekte van Von Hippel-Lindau fi:Von Hippel-Lindaun oireyhtymä