Unstable angina non ST elevation myocardial infarction electrocardiogram
| Resident Survival Guide |
|
Unstable angina / NSTEMI Microchapters |
|
Differentiating Unstable Angina/Non-ST Elevation Myocardial Infarction from other Disorders |
|
Special Groups |
|
Diagnosis |
|
Laboratory Findings |
|
Treatment |
|
Antitplatelet Therapy |
|
Additional Management Considerations for Antiplatelet and Anticoagulant Therapy |
|
Risk Stratification Before Discharge for Patients With an Ischemia-Guided Strategy of NSTE-ACS |
|
Mechanical Reperfusion |
|
Discharge Care |
|
Case Studies |
|
Unstable angina non ST elevation myocardial infarction electrocardiogram On the Web |
|
FDA on Unstable angina non ST elevation myocardial infarction electrocardiogram |
|
CDC onUnstable angina non ST elevation myocardial infarction electrocardiogram |
|
Unstable angina non ST elevation myocardial infarction electrocardiogram in the news |
|
Blogs on Unstable angina non ST elevation myocardial infarction electrocardiogram |
|
to Hospitals Treating Unstable angina non ST elevation myocardial infarction electrocardiogram |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editors-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]; Varun Kumar, M.B.B.S.; Lakshmi Gopalakrishnan, M.B.B.S.; Raviteja Guddeti, M.B.B.S. [3]
Overview
The EKG in patients with unstable angina can vary. In some cases, no changes on EKG will be appreciated. In other cases, a resting EKG may show flipped or inverted T waves, ST segment depression, or non-specific ST-T changes. It is the first line of assessment in any patient suspected of having unstable angina.
Electrocardiogram in Unstable Angina/NSTEMI
The resting electrocardiogram in the patient with unstable angina / non-ST elevation MI may show any of the following:
- No changes
- Non specific ST / T wave changes
- Flipped or inverted T waves
- ST depression as shown below. ST depression carries the poorest prognosis. Greater magnitudes of down sloping ST depression are associated with a high in-hospital, 30-day and 1-year mortality. 1 year MI or death rate in patients with new ST deviation (more than 1 mm from baseline) has been shown to be 11% compared to 6.8% in patients with isolated T-wave inversion.
Wellens' syndrome is an electrocardiographic manifestation of critical proximal left anterior descending (LAD) coronary artery stenosis in patients with unstable angina. It is characterized by symmetrical, often deep >2mm, T wave inversions in the anterior precordial leads. A less common variant is biphasic T wave inversions in the same leads.[1]
EKG Examples
Shown below is an EKG from a patient with unstable angina. ST depression in V2, V3, V4 and V6 can be noted:
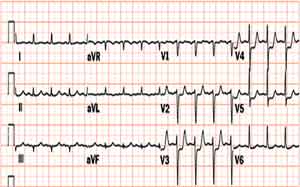
Copyleft image obtained courtesy of ECGpedia, http://en.ecgpedia.org/wiki/Main_Page
2014 AHA/ACC Guideline for the Management of Patients With Non–ST-Elevation Acute Coronary Syndromes (DO NOT EDIT) [2]
Early Risk Stratification
| Class I |
| "1. In patients with chest pain or other symptoms suggestive of ACS, a 12-lead ECG should be performed and evaluated for ischemic changes within 10 minutes of the patient’s arrival at an emergency facility. (Level of Evidence: C)" |
| "2. If the initial ECG is not diagnostic but the patient remains symptomatic and there is a high clinical suspicion for ACS, serial ECGs (e.g., 15- to 30-minute intervals during the first hour) should be performed to detect ischemic changes. (Level of Evidence: C)" |
| Class IIa |
| "1. It is reasonable to obtain supplemental electrocardiographic leads V7 to V9 in patients whose initial ECG is nondiagnostic and who are at intermediate/high risk of ACS. (Level of Evidence: B)" |
| Class IIb |
| "1. Continuous monitoring with 12-lead ECG may be a reasonable alternative in patients whose initial ECG is nondiagnostic and who are at intermediate/high risk of ACS. (Level of Evidence: B)" |
Immediate Management
Discharge From the ED or Chest Pain Unit
| Class IIa |
| "1. It is reasonable to observe patients with symptoms consistent with ACS without objective evidence of myocardial ischemia (nonischemic initial ECG and normal cardiac troponin) in a chest pain unit or telemetry unit with serial ECGs and cardiac troponin at 3- to 6-hour intervals. (Level of Evidence: B)" |
| "2. It is reasonable for patients with possible ACS who have normal serial ECGs and cardiac troponins to have a treadmill ECG before discharge or within 72 hours after discharge. (Level of Evidence: A)" |
References
- ↑ Tandy, TK (1999). "Wellens' syndrome". Annals of Emergency Medicine. 33 (3): 347–351. doi:10.1016/S0196-0644(99)70373-2. PMID 10036351. Unknown parameter
|month=ignored (help); Unknown parameter|coauthors=ignored (help) - ↑ Ezra A. Amsterdam, MD, FACC; Nanette K. Wenger, MD et al.2014 AHA/ACC Guideline for the Management of Patients With Non–ST-Elevation Acute Coronary Syndromes. A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. JACC. September 2014 (ahead of print)