Mepolizumab
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Martin Nino [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
Mepolizumab is an interleukin-5 antagonist monoclonal antibody (IgG1 kappa) that is FDA approved for the treatment of patients with severe asthma aged 12 years and older, and with an eosinophilic phenotype (indicated for add-on maintenance treatment). Common adverse reactions include headache, injection site reaction, back pain, and fatigue (5%).
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Indications
Mepolizumab is indicated for the add-on maintenance treatment of patients with severe asthma aged 12 years and older, and with an eosinophilic phenotype.
- Limitations of Use
- Mepolizumab is not indicated for treatment of other eosinophilic conditions.
- Mepolizumab is not indicated for the relief of acute bronchospasm or status asthmaticus.
Dosage
- Mepolizumab is for subcutaneous use only.
- The recommended dose of Mepolizumab is 100 mg administered once every 4 weeks by subcutaneous injection into the upper arm, thigh, or abdomen.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Mepolizumab in adult patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Mepolizumab in adult patients.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
The safety and efficacy in pediatric patients younger than 12 years have not been established. Same indications and dosage in patients aged 12 years or older.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Mepolizumab in pediatric patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Mepolizumab in pediatric patients.
Contraindications
Mepolizumab should not be administered to patients with a history of hypersensitivity to mepolizumab or excipients in the formulation.
Warnings
Hypersensitivity Reactions
Hypersensitivity reactions (e.g., angioedema, bronchospasm, hypotension, urticaria, rash) have occurred following administration of Mepolizumab. These reactions generally occur within hours of administration, but in some instances can have a delayed onset (i.e., days). In the event of a hypersensitivity reaction, Mepolizumab should be discontinued.
Acute Asthma Symptoms or Deteriorating Disease
Mepolizumab should not be used to treat acute asthma symptoms or acute exacerbations. Do not use Mepolizumab to treat acute bronchospasm or status asthmaticus. Patients should seek medical advice if their asthma remains uncontrolled or worsens after initiation of treatment with Mepolizumab.
Opportunistic Infections: Herpes Zoster
In controlled clinical trials, 2 serious adverse reactions of herpes zoster occurred in subjects treated with Mepolizumab compared with none in placebo. Consider varicella vaccination if medically appropriate prior to starting therapy with Mepolizumab.
Reduction of Corticosteroid Dosage
Do not discontinue systemic or inhaled corticosteroids abruptly upon initiation of therapy with Mepolizumab. Reductions in corticosteroid dose, if appropriate, should be gradual and performed under the direct supervision of a physician. Reduction in corticosteroid dose may be associated with systemic withdrawal symptoms and/or unmask conditions previously suppressed by systemic corticosteroid therapy.
Parasitic (Helminth) Infection
Eosinophils may be involved in the immunological response to some helminth infections. Patients with known parasitic infections were excluded from participation in clinical trials. It is unknown if Mepolizumab will influence a patient’s response against parasitic infections. Treat patients with pre-existing helminth infections before initiating therapy with Mepolizumab. If patients become infected while receiving treatment with Mepolizumab and do not respond to anti-helminth treatment, discontinue treatment with Mepolizumab until infection resolves.
Adverse Reactions
Clinical Trials Experience
The following adverse reactions are described in greater detail in other sections:
- Hypersensitivity reactions
- Opportunistic infections: herpes zoster
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared with rates in the clinical trials of another drug and may not reflect the rates observed in practice.
A total of 1,327 subjects with asthma were evaluated in 3 randomized, placebo-controlled, multicenter trials of 24 to 52 weeks’ duration (Trials 1, 2, and 3). Of these, 1,192 had a history of 2 or more exacerbations in the year prior to enrollment despite regular use of high-dose inhaled corticosteroids plus an additional controller(s) (Trials 1 and 2), and 135 subjects required daily oral corticosteroids in addition to regular use of high-dose inhaled corticosteroids plus an additional controller(s) to maintain asthma control (Trial 3). All subjects had markers of eosinophilic airway inflammation. Of the subjects enrolled, 59% were female, 85% were white, and subjects ranged in age from 12 to 82 years. Mepolizumab was administered subcutaneously or intravenously once every 4 weeks; 263 subjects received Mepolizumab (mepolizumab 100 mg subcutaneous [SC]) for at least 24 weeks. Serious adverse events that occurred in more than 1 subject and in a greater percentage of subjects treated with Mepolizumab (n = 263) than placebo (n = 257) included 1 event, herpes zoster (2 subjects vs. 0 subjects, respectively). Approximately 2% of subjects receiving Mepolizumab withdrew from clinical trials due to adverse events compared with 3% of subjects receiving placebo.
The incidence of adverse reactions in the first 24 weeks of treatment in the 2 confirmatory efficacy and safety trials (Trials 2 and 3) with Mepolizumab is shown in Table 1.
- Table 1. Adverse Reactions with Mepolizumab with Greater than or Equal to 3% Incidence and More Common than Placebo in Subjects with Asthma (Trials 2 and 3)
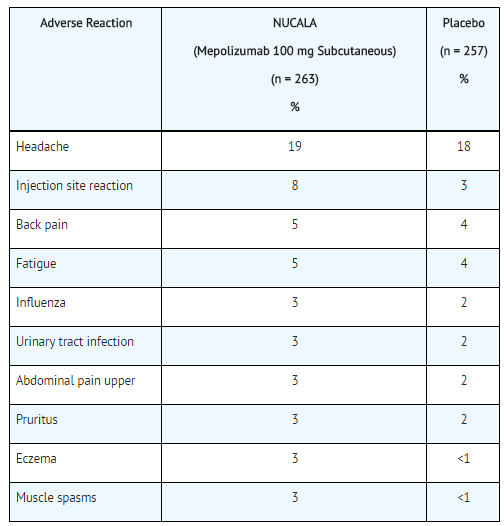
NUCALA: Mepolizumab's Brand name
- 52-Week Trial
- Adverse reactions from Trial 1 with 52 weeks of treatment with mepolizumab 75 mg intravenous (IV) (n = 153) or placebo (n = 155) and with greater than or equal to 3% incidence and more common than placebo and not shown in Table 1 were: abdominal pain, allergic rhinitis, asthenia, bronchitis, cystitis, dizziness, dyspnea, ear infection, gastroenteritis, lower respiratory tract infection, musculoskeletal pain, nasal congestion, nasopharyngitis, nausea, pharyngitis, pyrexia, rash, toothache, viral infection, viral respiratory tract infection, and vomiting. In addition, 3 cases of herpes zoster occurred in subjects treated with mepolizumab 75 mg IV, compared with 2 subjects in the placebo group.
- Systemic Reactions, including Hypersensitivity Reactions
- In Trials 1, 2, and 3 described above, the percentage of subjects who experienced systemic (allergic and non-allergic) reactions was 7% in the placebo group and 10% in the group receiving Mepolizumab. Systemic allergic/hypersensitivity reactions were reported by 2% of subjects in the placebo group and 1% of subjects in the group receiving Mepolizumab. The most commonly reported manifestations of systemic allergic/hypersensitivity reactions reported in the group receiving Mepolizumab included rash, pruritus, headache, and myalgia. Systemic non-allergic reactions were reported by 2% of subjects in the group receiving Mepolizumab and 3% of subjects in the placebo group. The most commonly reported manifestations of systemic non-allergic reactions reported in the group receiving Mepolizumab included rash, flushing, and myalgia. A majority of the systemic reactions in subjects receiving Mepolizumab (5/7) were experienced on the day of dosing.
- Injection Site Reactions
- Long-Term Safety
- Nine hundred ninety-eight (998) subjects have received Mepolizumab in ongoing open-label extension studies, during which additional cases of herpes zoster have been reported. The overall adverse event profile was similar to the asthma trials described above.
Immunogenicity
Overall, 15/260 (6%) of subjects treated with Mepolizumab developed anti-mepolizumab antibodies. The reported frequency may underestimate the actual frequency due to lower assay sensitivity in the presence of high drug concentration. Neutralizing antibodies were detected in 1 subject receiving mepolizumab. Anti-mepolizumab antibodies slightly increased (approximately 20%) the clearance of mepolizumab. There was no evidence of a correlation between anti-mepolizumab antibody titers and change in eosinophil level. The clinical relevance of the presence of anti-mepolizumab antibodies is not known.
The data reflect the percentage of patients whose test results were positive for antibodies to mepolizumab in specific assays. The observed incidence of antibody positivity in an assay is highly dependent on several factors, including assay sensitivity and specificity, assay methodology, sample handling, timing of sample collection, concomitant medications, and underlying disease.
Postmarketing Experience
There is limited information regarding Mepolizumab Postmarketing Experience in the drug label.
Drug Interactions
Formal drug interaction trials have not been performed with Mepolizumab.
Use in Specific Populations
Pregnancy
- Pregnancy Exposure Registry
- There is a pregnancy exposure registry that monitors pregnancy outcomes in women exposed to Mepolizumab during pregnancy. Healthcare providers can enroll patients or encourage patients to enroll themselves by calling 1-877-311-8972 or visiting WWW.MOTHERTOBABY.ORG/ASTHMA.
- Risk Summary
- The data on pregnancy exposure from the clinical trials are insufficient to inform on drug-associated risk. Monoclonal antibodies, such as mepolizumab, are transported across the placenta in a linear fashion as pregnancy progresses; therefore, potential effects on a fetus are likely to be greater during the second and third trimester of pregnancy. In a prenatal and postnatal development study conducted in cynomolgus monkeys, there was no evidence of fetal harm with IV administration of mepolizumab throughout pregnancy at doses that produced exposures up to approximately 30 times the exposure at the maximum recommended human dose (MRHD) of 100 mg SC.
- In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
- Clinical Considerations
- Disease-Associated Maternal and/or Embryo-Fetal Risk: In women with poorly or moderately controlled asthma, evidence demonstrates that there is an increased risk of preeclampsia in the mother and prematurity, low birth weight, and small for gestational age in the neonate. The level of asthma control should be closely monitored in pregnant women and treatment adjusted as necessary to maintain optimal control.
- Data
- Animal Data: In a prenatal and postnatal development study, pregnant cynomolgus monkeys received mepolizumab from gestation days 20 to 140 at doses that produced exposures up to approximately 30 times that achieved with the MRHD (on an AUC basis with maternal IV doses up to 100 mg/kg once every 4 weeks). Mepolizumab did not elicit adverse effects on fetal or neonatal growth (including immune function) up to 9 months after birth. Examinations for internal or skeletal malformations were not performed. Mepolizumab crossed the placenta in cynomolgus monkeys. Concentrations of mepolizumab were approximately 2.4 times higher in infants than in mothers up to day 178 postpartum. Levels of mepolizumab in milk were less than or equal to 0.5% of maternal serum concentration.
- In a fertility, early embryonic, and embryo-fetal development study, pregnant CD-1 mice received an analogous antibody, which inhibits the activity of murine IL-5, at an IV dose of 50 mg/kg once per week throughout gestation. The analogous antibody was not teratogenic in mice. Embryo-fetal development of IL-5–deficient mice has been reported to be generally unaffected relative to wild-type mice.
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Mepolizumab in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Mepolizumab during labor and delivery.
Nursing Mothers
There is no information regarding the presence of mepolizumab in human milk, the effects on the breastfed infant, or the effects on milk production. However, mepolizumab is a humanized monoclonal antibody (IgG1 kappa), and immunoglobulin G (IgG) is present in human milk in small amounts. Mepolizumab was present in the milk of cynomolgus monkeys postpartum following dosing during pregnancy. The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for Mepolizumab and any potential adverse effects on the breastfed infant from mepolizumab or from the underlying maternal condition.
Pediatric Use
The safety and efficacy in pediatric patients younger than 12 years have not been established. A total of 28 adolescents aged 12 to 17 years with asthma were enrolled in the phase 3 studies. Of these, 25 were enrolled in the 32-week exacerbation trial (Trial 2) and had a mean age of 14.8 years. Subjects had a history of 2 or more exacerbations in the previous year despite regular use of high-dose inhaled corticosteroids plus an additional controller(s) with or without oral corticosteroids and had blood eosinophils of greater than or equal to 150 cells/mcL at screening or greater than or equal to 300 cells/mcL within 12 months prior to enrollment. Subjects had a reduction in the rate of exacerbations that trended in favor of mepolizumab. Of the 19 adolescents who received mepolizumab, 9 received Mepolizumab and the mean apparent clearance in these subjects was 35% less than that of adults. The adverse event profile in adolescents was generally similar to the overall population in the phase 3 studies.
Geriatic Use
Clinical trials of Mepolizumab did not include sufficient numbers of subjects aged 65 years and older that received Mepolizumab (n = 38) to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function and of concomitant disease or other drug therapy. Based on available data, no adjustment of the dosage of Mepolizumab in geriatric patients is necessary, but greater sensitivity in some older individuals cannot be ruled out.
Gender
There is no FDA guidance on the use of Mepolizumab with respect to specific gender populations.
Race
There is no FDA guidance on the use of Mepolizumab with respect to specific racial populations.
Renal Impairment
There is no FDA guidance on the use of Mepolizumab in patients with renal impairment.
Hepatic Impairment
There is no FDA guidance on the use of Mepolizumab in patients with hepatic impairment.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Mepolizumab in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Mepolizumab in patients who are immunocompromised.
Administration and Monitoring
Administration
Mepolizumab should be reconstituted and administered by a healthcare professional. In line with clinical practice, monitoring of patients after administration of biologic agents is recommended.
- Reconstitution Instructions
- 1. Reconstitute Mepolizumab in the vial with 1.2 mL Sterile Water for Injection, USP, preferably using a 2- or 3-mL syringe and a 21-G needle. The reconstituted solution will contain a concentration of 100 mg/mL mepolizumab. Do not mix with other medications.
- 2. Direct the stream of Sterile Water for Injection vertically onto the center of the lyophilized cake. Gently swirl the vial for 10 seconds with a circular motion at 15-second intervals until the powder is dissolved.
- Note: Do not shake the reconstituted solution during the procedure as this may lead to product foaming or precipitation. Reconstitution is typically complete within 5 minutes after the Sterile Water for Injection has been added, but it may take additional time.
- 3. If a mechanical reconstitution device (swirler) is used to reconstitute Mepolizumab, swirl at 450 rpm for no longer than 10 minutes. Alternatively, swirling at 1,000 rpm for no longer than 5 minutes is acceptable.
- 4. Visually inspect the reconstituted solution for particulate matter and clarity before use. The solution should be clear to opalescent and colorless to pale yellow or pale brown, essentially particle free. Small air bubbles, however, are expected and acceptable. If particulate matter remains in the solution or if the solution appears cloudy or milky, discard the solution.
- 5. If the reconstituted solution is not used immediately:
- - store below 30°C (86°F),
- - do not freeze, and
- - discard if not used within 8 hours of reconstitution.
- Administration
- 1. For subcutaneous administration, preferably using a 1-mL polypropylene syringe fitted with a disposable 21- to 27-G x 0.5-inch (13-mm) needle.
- 2. Just before administration, remove 1 mL of reconstituted Mepolizumab. Do not shake the reconstituted solution during the procedure as this could lead to product foaming or precipitation.
- 3. Administer the 1-mL injection (equivalent to 100 mg mepolizumab) subcutaneously into the upper arm, thigh, or abdomen.
Monitoring
There is limited information regarding Mepolizumab Monitoring in the drug label.
IV Compatibility
There is limited information regarding the compatibility of Mepolizumab and IV administrations.
Overdosage
Single doses of up to 1,500 mg have been administered intravenously to subjects in a clinical trial with eosinophilic disease without evidence of dose-related toxicities.
There is no specific treatment for an overdose with mepolizumab. If overdose occurs, the patient should be treated supportively with appropriate monitoring as necessary.
Pharmacology
Mepolizumab?
| |
| Therapeutic monoclonal antibody | |
| Source | zu/o |
| Target | IL-5 |
| Identifiers | |
| CAS number | |
| ATC code | R03 |
| PubChem | ? |
| DrugBank | |
| Chemical data | |
| Formula | ? |
| Mol. mass | ~149 kg/mol |
| Pharmacokinetic data | |
| Bioavailability | 80% (estimate) |
| Protein binding | None |
| Metabolism | Proteolytic enzymes |
| Half life | 20 (16–22) days |
| Excretion | ? |
| Therapeutic considerations | |
| Pregnancy cat. |
? |
| Legal status |
[[Prescription drug|Template:Unicode-only]](US) |
| Routes | Subcutaneous injection |
Mechanism of Action
Mepolizumab is an interleukin-5 antagonist (IgG1 kappa). IL-5 is the major cytokine responsible for the growth and differentiation, recruitment, activation, and survival of eosinophils. Mepolizumab binds to IL-5 with a dissociation constant of 100 pM, inhibiting the bioactivity of IL-5 by blocking its binding to the alpha chain of the IL-5 receptor complex expressed on the eosinophil cell surface. Inflammation is an important component in the pathogenesis of asthma. Multiple cell types (e.g., mast cells, eosinophils, neutrophils, macrophages, lymphocytes) and mediators (e.g., histamine, eicosanoids, leukotrienes, cytokines) are involved in inflammation. Mepolizumab, by inhibiting IL-5 signaling, reduces the production and survival of eosinophils; however, the mechanism of mepolizumab action in asthma has not been definitively established.
Structure
Mepolizumab is a humanized IL-5 antagonist monoclonal antibody. Mepolizumab is produced by recombinant DNA technology in Chinese hamster ovary cells. Mepolizumab has a molecular weight of approximately 149 kDa.
Mepolizumab is supplied as a sterile, white to off-white, preservative-free, lyophilized powder for subcutaneous injection after reconstitution. Upon reconstitution with 1.2 mL of Sterile Water for Injection, USP, the resulting concentration is 100 mg/mL and delivers 1 mL. Each single-dose vial delivers mepolizumab 100 mg, polysorbate 80 (0.67 mg), sodium phosphate dibasic heptahydrate (7.14 mg), and sucrose (160 mg), with a pH of 7.0.
Pharmacodynamics
The pharmacodynamic response (blood eosinophil reduction) following repeat doses of mepolizumab administered subcutaneously or intravenously was evaluated in subjects with asthma and blood eosinophil levels greater than 200 cells/mcL. Subjects received 1 of 4 mepolizumab treatments (administered every 28 days for a total of 3 doses): 12.5 mg SC, 125 mg SC, 250 mg SC, or 75 mg IV. Sixty-six (66) of the 70 randomized subjects completed the trial. Compared with baseline levels, blood eosinophils decreased in a dose-dependent manner. A reduction in blood eosinophil levels was observed in all treatment groups by Day 3. On Day 84 (4 weeks post-last dose), the observed geometric mean reduction from baseline in blood eosinophils was 64%, 78%, 84%, and 90% in the 12.5-mg SC, 75-mg IV, 125-mg SC, and 250-mg SC treatment groups, respectively. The model-predicted SC doses providing 50% and 90% of maximal reduction of blood eosinophils at Day 84 were estimated to be 11 and 99 mg, respectively. These results, along with the clinical efficacy data from the dose-ranging exacerbation trial (Trial 1) supported the evaluation of mepolizumab 75 mg IV and 100 mg SC in the confirmatory trials. Following SC administration of mepolizumab 100 mg every 4 weeks for 32 weeks (Trial 2), blood eosinophils were reduced to a geometric mean count of 40 cells/mcL, which corresponds to a geometric mean reduction of 84% compared with placebo. This magnitude of reduction was observed within 4 weeks of treatment and was maintained throughout the treatment period.
Pharmacokinetics
Following SC dosing in subjects with asthma, mepolizumab exhibited approximately dose-proportional pharmacokinetics over a dose range of 12.5 to 250 mg.
- Following 100-mg SC administration in the upper arm of subjects with asthma, the bioavailability of mepolizumab was estimated to be approximately 80%.
- Following repeat SC administration once every 4 weeks, there was approximately a 2-fold accumulation at steady state.
- The population central volume of distribution of mepolizumab in patients with asthma is estimated to be 3.6 L for a 70‑kg individual.
- Mepolizumab is a humanized IgG1 monoclonal antibody that is degraded by proteolytic enzymes widely distributed in the body and not restricted to hepatic tissue.
Elimination
Specific Populations
- Race and Gender: A population pharmacokinetics analysis indicated there was no significant effect of race and gender on mepolizumab clearance.
- Age: A population pharmacokinetics analysis of subjects ranging in age from 12 to 82 years indicated there was no significant effect of age on mepolizumab clearance.
- Renal Impairment: No clinical trials have been conducted to investigate the effect of renal impairment on the pharmacokinetics of mepolizumab. Based on population pharmacokinetic analyses, mepolizumab clearance was comparable between subjects with creatinine clearance values between 50 and 80 mL/min and patients with normal renal function. There are limited data available in subjects with creatinine clearance values less than 50 mL/min; however, mepolizumab is not cleared renally.
- Hepatic Impairment: No clinical trials have been conducted to investigate the effect of hepatic impairment on the pharmacokinetics of mepolizumab. Since mepolizumab is degraded by widely distributed proteolytic enzymes, not restricted to hepatic tissue, changes in hepatic function are unlikely to have any effect on the elimination of mepolizumab.
- Drug-Drug Interactions: No formal drug interaction studies have been conducted with Mepolizumab. In the population pharmacokinetics analyses of the phase 3 studies, there was no evidence of an effect of commonly coadministered small molecule drugs on mepolizumab exposure.
Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility
Long-term animal studies have not been performed to evaluate the carcinogenic potential of mepolizumab. Published literature using animal models suggests that IL-5 and eosinophils are part of an early inflammatory reaction at the site of tumorigenesis and can promote tumor rejection. However, other reports indicate that eosinophil infiltration into tumors can promote tumor growth. Therefore, the malignancy risk in humans from an antibody to IL-5 such as mepolizumab is unknown.
Male and female fertility were unaffected based upon no adverse histopathological findings in the reproductive organs from cynomolgus monkeys treated with mepolizumab for 6 months at IV doses up to 100 mg/kg once every 4 weeks (approximately 70 times the MRHD on an AUC basis). Mating and reproductive performance were unaffected in male and female CD-1 mice treated with an analogous antibody, which inhibits the activity of murine IL-5, at an IV dose of 50 mg/kg once per week.
Clinical Studies
The asthma development program for Mepolizumab included 3 double-blind, randomized, placebo-controlled trials: 1 dose-ranging and exacerbation trial (Trial 1) and 2 confirmatory trials (Trials 2 and 3). Mepolizumab was administered every 4 weeks in all 3 trials as add-on to background treatment. All subjects continued their background asthma therapy throughout the duration of the trials.
- Dose-Ranging and Exacerbation Trial
- Trial 1 was a 52-week dose-ranging and exacerbation-reduction trial in subjects with asthma with a history of 2 or more exacerbations in the previous year despite regular use of high-dose inhaled corticosteroids plus an additional controller(s) with or without oral corticosteroids. Subjects enrolled in this trial were required to have at least 1 of the following 4 pre-specified criteria in the previous 12 months: blood eosinophil count greater than or equal to 300 cells/mcL, sputum eosinophil count greater than or equal to 3%, exhaled nitric oxide concentration greater than or equal to 50 ppb, or deterioration of asthma control after less than or equal to 25% reduction in regular maintenance inhaled corticosteroids/oral corticosteroids. Three IV doses of mepolizumab (75, 250, and 750 mg) administered once every 4 weeks were evaluated compared with placebo. Results from this trial and the pharmacodynamic study supported the evaluation of mepolizumab 75 mg IV and 100 mg SC in the subsequent trials. Mepolizumab is not indicated for IV use and should only be administered by the SC route.
- Confirmatory Trials
- A total of 711 subjects with asthma were studied in the 2 confirmatory trials (Trials 2 and 3). In these 2 trials subjects were required to have blood eosinophils of greater than or equal to 150 cells/mcL at screening (within 6 weeks of dosing) or blood eosinophils of greater than or equal to 300 cells/mcL within 12 months of enrollment. The screening blood eosinophils of greater than or equal to 150 cells/mcL criterion was derived from exploratory analyses of data from Trial 1. Trial 2 was a 32-week placebo- and active-controlled trial in subjects with asthma with a history of 2 or more exacerbations in the previous year despite regular use of high-dose inhaled corticosteroids plus an additional controller(s) with or without oral corticosteroids. Subjects received mepolizumab 75 mg IV (n = 191), Mepolizumab (n = 194), or placebo (n = 191) once every 4 weeks for 32 weeks.
- Trial 3 was a 24-week oral corticosteroid-reduction trial in subjects with asthma who required daily oral corticosteroids in addition to regular use of high-dose inhaled corticosteroids plus an additional controller(s) to maintain asthma control. Subjects in Trial 3 were not required to have a history of exacerbations in the prior year. Subjects received Mepolizumab (n = 69) or placebo (n = 66) once every 4 weeks for 24 weeks. The baseline mean oral corticosteroid use was similar in the 2 treatment groups: 13.2 mg in the placebo group and 12.4 mg in the group receiving Mepolizumab.
- The demographics and baseline characteristics of these 3 trials are provided in Table 2.
- Table 2. Demographics and Baseline Characteristics of Asthma Trials

- Exacerbations
- The primary endpoint for Trials 1 and 2 was the frequency of exacerbations defined as worsening of asthma requiring use of oral/systemic corticosteroids and/or hospitalization and/or emergency department visits. For subjects on maintenance oral corticosteroids, an exacerbation requiring oral corticosteroids was defined as the use of oral/systemic corticosteroids at least double the existing dose for at least 3 days. Compared with placebo, subjects receiving Mepolizumab or mepolizumab 75 mg IV experienced significantly fewer exacerbations. Additionally, compared with placebo, there were fewer exacerbations requiring hospitalization and/or emergency department visits and exacerbations requiring only in-patient hospitalization with Mepolizumab (Table 3).
- Table 3. Rate of Exacerbations in Trials 1 and 2 (Intent-to-Treat Population)

NUCALA: Mepolizumab's Brand name
- The time to first exacerbation was longer for the groups receiving Mepolizumab and mepolizumab 75 mg IV compared with placebo in Trial 2 (Figure 1).
- Figure 1. Kaplan-Meier Cumulative Incidence Curve for Time to First Exacerbation (Trial 2)

NUCALA: Mepolizumab's Brand name
- Trial 1 data were explored to determine criteria that could identify subjects likely to benefit from treatment with Mepolizumab. The exploratory analysis suggested that baseline blood eosinophil count of 150 cells/mcL or greater was a potential predictor of treatment benefit. Exploratory analysis of Trial 2 data also suggested that baseline blood eosinophil count (obtained within 6 weeks of initiation of dosing) of 150 cells/mcL or greater was a potential predictor of efficacy and showed a trend of greater exacerbation benefit with increasing blood eosinophil count. In Trial 2, subjects enrolled solely on the basis of the historical blood eosinophil count of 300 cells/mcL or greater in the past 12 months, but who had a baseline blood eosinophil count less than 150 cells/mcL, had virtually no exacerbation benefit following treatment with Mepolizumab compared with placebo.
- The Asthma Control Questionnaire-5 (ACQ-5) was assessed in Trials 1 and 2, and the St. Georges Respiratory Questionnaire (SGRQ) was assessed in Trial 2. In Trial 1, the ACQ-5 responder rate (defined as a change in score of 0.5 or more as threshold) for the 75-mg IV mepolizumab arm was 47% compared with 50% for placebo with odds ratio of 1.1 (95% CI: 0.7, 1.7). In Trial 2, the ACQ-5 responder rate for the treatment arm for Mepolizumab was 57% compared with 45% for placebo with odds ratio of 1.8 (95% CI: 1.2, 2.8). In Trial 2, the SGRQ responder rate (defined as a change in score of 4 or more as threshold) for the treatment arm for Mepolizumab was 71% compared with 55% for placebo with odds ratio of 2.1 (95% CI: 1.3, 3.2).
- Oral Corticosteroid Reduction
- Trial 3 evaluated the effect of Mepolizumab on reducing the use of maintenance oral corticosteroids. The primary endpoint was the percent reduction of oral corticosteroid dose during Weeks 20 to 24 compared with baseline dose, while maintaining asthma control. Subjects were classified according to their change in oral corticosteroid use during the trial with the following categories: 90% to 100% decrease, 75% to <90% decrease, 50% to <75% decrease, >0% to <50% decrease, and no improvement (i.e., no change or any increase or lack of asthma control or withdrawal of treatment). Compared with placebo, subjects receiving Mepolizumab achieved greater reductions in daily maintenance oral corticosteroid dose, while maintaining asthma control. Sixteen (23%) subjects in the group receiving Mepolizumab versus 7 (11%) in the placebo group had a 90%to 100% reduction in their oral corticosteroid dose. Twenty-five (36%) subjects in the group receiving Mepolizumab versus 37 (56%) in the placebo group were classified as having no improvement for oral corticosteroid dose. Additionally, 54% of subjects treated with Mepolizumab achieved at least a 50% reduction in the daily prednisone dose compared with 33% of subjects treated with placebo (95% CI for difference: 4%, 37%). An exploratory analysis was also performed on the subgroup of 29 subjects in Trial 3 who had an average baseline and screening blood eosinophil count less than 150 cells/mcL. Five (29%) subjects in the group receiving Mepolizumab versus 0 (0%) in the placebo group had a 90% to 100% reduction in their dose. Four (24%) subjects in the group receiving Mepolizumab versus eight (67%) in the placebo group were classified as having no improvement for oral corticosteroid dose. The ACQ and SGRQ were also assessed in Trial 3 and showed results similar to those in Trial 2.
- Change from baseline in mean forced expiratory volume in 1 second (FEV1) was measured in all 3 trials and is presented in Table 4. Compared with placebo, Mepolizumab did not provide consistent improvements in mean change from baseline in FEV1.
- Table 4. Change from Baseline in FEV1 (mL)

- The effect of mepolizumab on lung function was also studied in a 12-week, placebo-controlled trial enrolling patients with asthma on a moderate dose of inhaled corticosteroid with evidence of symptoms and lung function impairment. Enrollment was not dependent on a history of exacerbations or a pre-specified eosinophil count. Change from baseline in FEV1 at Week 12 was numerically lower in the mepolizumab treatment groups than the placebo group.
How Supplied
Mepolizumab is supplied as a sterile, preservative-free, lyophilized powder for reconstitution and subcutaneous injection in cartons of 1 single-dose glass vial and a flip-off seal. The vial stopper is not made with natural rubber latex. Mepolizumab is available as:
- 100-mg single-dose vial (NDC 0173-0881-01).
Storage
Store below 25°C (77°F). Do not freeze. Store in the original package to protect from light.
Images
Drug Images
{{#ask: Page Name::Mepolizumab |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel

{{#ask: Label Page::Mepolizumab |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
Advise the patient to read the FDA-approved patient labeling (Patient Information).
- Hypersensitivity Reactions
- Inform patients that hypersensitivity reactions (e.g., angioedema, bronchospasm, hypotension, urticaria, rash) have occurred after administration of Mepolizumab. Instruct patients to contact their physicians if such reactions occur.
- Not for Acute Symptoms or Deteriorating Disease
- Inform patients that Mepolizumab does not treat acute asthma symptoms or acute exacerbations. Inform patients to seek medical advice if their asthma remains uncontrolled or worsens after initiation of treatment with Mepolizumab.
- Opportunistic Infections: Herpes Zoster
- Inform patients that herpes zoster infections have occurred in patients receiving Mepolizumab and where medically appropriate, inform patients varicella vaccination should be considered before starting treatment with Mepolizumab.
- Reduction of Corticosteroid Dosage
- Inform patients to not discontinue systemic or inhaled corticosteroids except under the direct supervision of a physician. Inform patients that reduction in corticosteroid dose may be associated with systemic withdrawal symptoms and/or unmask conditions previously suppressed by systemic corticosteroid therapy.
- Pregnancy Exposure Registry
- Inform women there is a pregnancy exposure registry that monitors pregnancy outcomes in women exposed to Mepolizumab during pregnancy and that they can enroll in the Pregnancy Exposure Registry by calling 1-877-311-8972 or by visiting WWW.MOTHERTOBABY.ORG/ASTHMA.

Precautions with Alcohol
Alcohol-Mepolizumab interaction has not been established. Talk to your doctor regarding the effects of taking alcohol with this medication.
Brand Names
NUCALA®
Look-Alike Drug Names
There is limited information regarding Mepolizumab Look-Alike Drug Names in the drug label.
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.