Erlotinib
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Sheng Shi, M.D. [2]; Sree Teja Yelamanchili, MBBS [3]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
Erlotinib is a tyrosine kinase nhibitor that is FDA approved for the treatment of non small cell lung cancer (NSCLC), pancreatic cancer. Common adverse reactions include edema,alopecia,pruritus,rash,decreased weight,abdominal pain,diarrhea,flatulence, indigestion,inflammatory disease of mucous membrane,loss of appetite,nausea,vomiting, hyperbilirubinemia, increased liver enzymes,infectious disease,bone pain,myalgia,headache,conjunctivitis, keratoconjunctivitis sicca,anxiety,depression,cough,dyspnea,fatigue, fever..
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Non-Small Cell Lung Cancer (NSCLC)
- Dosing information
- Recommended daily dosage: 150 mg PO qdtaken on an empty stomach,
- i.e., at least one hour before or two hours after the ingestion of food.
- Treatment should continue until disease progression or unacceptable toxicity occurs.
Pancreatic Cancer
- Dosing information
- Recommended daily dosage: 100 mg taken PO qd in combination with gemcitabine.
- Take Erlotinib on an empty stomach, i.e., at least one hour before or two hours after the ingestion of food. Treatment should continue until disease progression or unacceptable toxicity occurs
Dose Modifications
Discontinue Erlotinib for:
- Severe hepatotoxicity that does not improve significantly or resolve within three weeks
- Severe bullous, blistering or exfoliating skin conditions
- Corneal perforation or severe ulceration
Withhold Erlotinib:
- During diagnostic evaluation for possible ILD.
- For severe (CTCAE grade 3 to 4) renal toxicity, and consider discontinuation of Erlotinib.
- In patients without pre-existing hepatic impairment for total bilirubin levels greater than 3 times the upper limit of normal or transaminases greater than 5 times the upper limit of normal, and consider discontinuation of Erlotinib.
- In patients with pre-existing hepatic impairment or biliary obstruction for doubling of bilirubin or tripling of transaminases values over baseline and consider discontinuation of Erlotinib.
- For persistent severe diarrhea not responsive to medical management (e.g., loperamide).
- For severe rash not responsive to medical management.
- For keratitis of (NCI-CTC version 4.0) grade 3-4 or for grade 2 lasting more than 2 weeks.
- For acute/worsening ocular disorders such as eye pain, and consider discontinuation of Erlotinib
Reduce Erlotinib by 50 mg decrements:
- If severe reactions occur with concomitant use of strong CYP3A4 inhibitors such as atazanavir, clarithromycin, indinavir, itraconazole, ketoconazole, nefazodone, nelfinavir, ritonavir, saquinavir, telithromycin, troleandomycin (TAO), voriconazole, or grapefruit or grapefruit juice or when using concomitantly with an inhibitor of both CYP3A4 and CYP1A2 (e.g., ciprofloxacin). Avoid concomitant use if possible.
- When restarting therapy following withholding treatment for a dose-limiting toxicity that has resolved to baseline or grade ≤ 1.
Increase Erlotinib by 50 mg increments as tolerated for:
- Concomitant use with CYP3A4 inducers, such as rifampin, rifabutin, rifapentine, phenytoin, carbamazepine, phenobarbital, or St. John’s Wort. Increase doses by 50 mg increments at 2 week intervals to a maximum of 450 mg. Avoid concomitant use, if possible
- Concurrent cigarette smoking. Increase by 50 mg increments at 2 week intervals to a maximum of 300 mg. Immediately reduce the dose of Erlotinib to the recommended dose (150 mg or 100 mg daily) upon cessation of smoking
Drugs Affecting Gastric pH
- Avoid concomitant use of Erlotinib with proton pump inhibitors if possible. Separation of doses may not eliminate the interaction since proton pump inhibitors affect the pH of the upper GI tract for an extended period.
- If treatment with an H2-receptor antagonist such as ranitidine is required, Erlotinib must be taken 10 hours after the H2-receptor antagonist dosing and at least 2 hours before the next dose of the H2-receptor antagonist.
- Although the effect of antacids on erlotinib pharmacokinetics has not been evaluated, the antacid dose and the Erlotinib dose should be separated by several hours, if an antacid is necessary.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Erlotinib in adult patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Erlotinib in adult patients.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
The safety and effectiveness of Erlotinib in pediatric patients have not been established.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Erlotinib in pediatric patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Erlotinib in pediatric patients.
Contraindications
None
Warnings
Interstitial Lung Disease (ILD)
Cases of serious ILD, including fatal cases, can occur with Erlotinib treatment. The overall incidence of ILD in approximately 32,000 Erlotinib-treated patients in uncontrolled studies and studies with concurrent chemotherapy was approximately 1.1%. In patients with ILD, the onset of symptoms was between 5 days to more than 9 months (median 39 days) after initiating Erlotinib therapy. Withhold Erlotinib for acute onset of new or progressive unexplained pulmonary symptoms such as dyspnea, cough, and fever pending diagnostic evaluation. If ILD is confirmed, permanently discontinue Erlotinib.
Renal Failure
Hepatorenal syndrome, severe acute renal failure including fatal cases, and renal insufficiency can occur with Erlotinib treatment. Renal failure may arise from exacerbation of underlying baseline hepatic impairment or severe dehydration. The pooled incidence of severe renal impairment in the 3 monotherapy lung cancer studies was 0.5% in the Erlotinib arms and 0.8% in the control arms. The incidence of renal impairment in the pancreatic cancer study was 1.4% in the Erlotinib plus gemcitabine arm and 0.4% in the control arm. Withhold Erlotinib in patients developing severe renal impairment until renal toxicity is resolved. Perform periodic monitoring of renal function and serum electrolytes during Erlotinib treatment.
Hepatotoxicity with or without Hepatic Impairment
Hepatic failure and hepatorenal syndrome, including fatal cases, can occur with Erlotinib treatment in patients with normal hepatic function; the risk of hepatic toxicity is increased in patients with baseline hepatic impairment. In clinical studies where patients with moderate to severe hepatic impairment were excluded, the pooled incidence of hepatic failure in the 3 monotherapy lung cancer studies was 0.4% in the Erlotinib arms and 0% in the control arms. The incidence of hepatic failure in the pancreatic cancer study was 0.4% in the Erlotinib plus gemcitabine arm and 0.4% in the control arm. In a pharmacokinetic study in 15 patients with moderate hepatic impairment (Child-Pugh B) associated with significant liver tumor burden, 10 of these 15 patients died within 30 days of the last Erlotinib dose. One patient died from hepatorenal syndrome, 1 patient died from rapidly progressing liver failure and the remaining 8 patients died from progressive disease. Six out of the 10 patients who died had baseline total bilirubin > 3 x ULN. Perform periodic liver testing (transaminases, bilirubin, and alkaline phosphatase) during treatment with Erlotinib. Increased frequency of monitoring of liver function is required for patients with pre-existing hepatic impairment or biliary obstruction. Withhold Erlotinib in patients without pre-existing hepatic impairment for total bilirubin levels greater than 3 times the upper limit of normal or transaminases greater than 5 times the upper limit of normal. Withhold Erlotinib in patients with pre-existing hepatic impairment or biliary obstruction for doubling of bilirubin or tripling of transaminases values over baseline. Discontinue Erlotinib in patients whose abnormal liver tests meeting the above criteria do not improve significantly or resolve within three weeks.
Gastrointestinal Perforation
Gastrointestinal perforation, including fatal cases, can occur with Erlotinib treatment. Patients receiving concomitant anti-angiogenic agents, corticosteroids, NSAIDs, or taxane-based chemotherapy, or who have prior history of peptic ulceration or diverticular disease may be at increased risk of perforation. The pooled incidence of gastrointestinal perforation in the 3 monotherapy lung cancer studies was 0.2% in the Erlotinib arms and 0.1% in the control arms. The incidence of gastrointestinal perforation in the pancreatic cancer study was 0.4% in the Erlotinib plus gemcitabine arm and 0% in the control arm. Permanently discontinue Erlotinib in patients who develop gastrointestinal perforation.
Bullous and Exfoliative Skin Disorders
Bullous, blistering and exfoliative skin conditions, including cases suggestive of Stevens-Johnson syndrome/Toxic epidermal necrolysis, which in some cases were fatal, can occur with Erlotinib treatment . The pooled incidence of bullous and exfoliative skin disorders in the 3 monotherapy lung cancer studies was 1.2% in the Erlotinib arms and 0% in the control arms. The incidence of bullous and exfoliative skin disorders in the pancreatic cancer study was 0.4% in the Erlotinib plus gemcitabine arm and 0% in the control arm. Discontinue Erlotinib treatment if the patient develops severe bullous, blistering or exfoliating conditions .
Myocardial Infarction/Ischemia
In the pancreatic carcinoma trial, six patients (incidence of 2.1%) in the Erlotinib/gemcitabine group developed myocardial infarction/ischemia. One of these patients died due to myocardial infarction. In comparison, 3 patients in the placebo/gemcitabine group developed myocardial infarction (incidence 1.1%), and one died due to myocardial infarction. The pooled incidence of myocardial infarction/ischemia in the 3 monotherapy lung cancer studies was 0.2% in the Erlotinib arms and 0.4% in the control arms.
Cerebrovascular Accident
In the pancreatic carcinoma trial, seven patients in the Erlotinib/gemcitabine group developed cerebrovascular accidents (incidence: 2.5%). One of these was hemorrhagic and was the only fatal event. In comparison, in the placebo/gemcitabine group there were no cerebrovascular accidents. The pooled incidence of cerebrovascular accident in the 3 monotherapy lung cancer studies was 0.6% in the Erlotinib arms and 0.9% in the control arms.
Microangiopathic Hemolytic Anemia with Thrombocytopenia
The pooled incidence of microangiopathic hemolytic anemia with thrombocytopenia in the 3 monotherapy lung cancer studies was 0% in the Erlotinib arms and 0.1% in the control arms. The incidence of microangiopathic hemolytic anemia with thrombocytopenia in the pancreatic cancer study was 1.4% in the Erlotinib plus gemcitabine arm and 0% in the control arm.
Ocular Disorders
Decreased tear production, abnormal eyelash growth, keratoconjunctivitis sicca or keratitis can occur with Erlotinib treatment and can lead to corneal perforation or ulceration. The pooled incidence of ocular disorders in the 3 monotherapy lung cancer studies was 17.8% in the Erlotinib arms and 4% in the control arms. The incidence of ocular disorders in the pancreatic cancer study was 12.8% in the Erlotinib plus gemcitabine arm and 11.4% in the control arm. Interrupt or discontinue Erlotinib therapy if patients present with acute or worsening ocular disorders such as eye pain.
Hemorrhage in Patients Taking Warfarin
Severe and fatal hemorrhage associated with International Normalized Ratio (INR) elevations can occur when Erlotinib and warfarin are administered concurrently. Regularly monitor prothrombin time and INR during Erlotinib treatment in patients taking warfarin or other coumarin-derivative anticoagulants.
Embryo-Fetal Toxicity
Based on its mechanism of action, Erlotinib can cause fetal harm when administered to a pregnant woman. When given during organogenesis, erlotinib administration resulted in embryo-fetal lethality and abortion in rabbits at doses approximately 3 times the recommended human daily dose of 150 mg. If Erlotinib is used during pregnancy, or if the patient becomes pregnant while taking this drug, the patient should be apprised of the potential hazard to a fetus. Advise females of reproductive potential to use highly effective contraception during therapy, and for at least 2 weeks after the last dose of Erlotinib. Advise patients to contact their healthcare provider if they become pregnant, or if pregnancy is suspected, while taking Erlotinib.
Adverse Reactions
Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
- Safety evaluation of Erlotinib is based on more than 1200 cancer patients who received Erlotinib as monotherapy, more than 300 patients who received Erlotinib 100 or 150 mg plus gemcitabine, and 1228 patients who received Erlotinib concurrently with other chemotherapies.
- The most common adverse reactions with Erlotinib are rash and diarrhea usually with onset during the first month of treatment.
- The incidences of rash and diarrhea from clinical studies of Erlotinib for the treatment of NSCLC and pancreatic cancer were 70% for rash and 42% for diarrhea.
Non-Small Cell Lung Cancer
First-Line Treatment of Patients with EGFR Mutations
The most frequent (≥ 30%) adverse reactions in Erlotinib-treated patients were diarrhea, asthenia, rash, cough, dyspnea and decreased appetite. In Erlotinib-treated patients the median time to onset of rash was 15 days and the median time to onset of diarrhea was 32 days. The most frequent Grade 3-4 adverse reactions in Erlotinib-treated patients were rash and diarrhea. Dose interruptions or reductions due to adverse reactions occurred in 37% of Erlotinib-treated patients, and 14.3% of Erlotinib-treated patients discontinued therapy due to adverse reactions. In Erlotinib-treated patients, the most frequently reported adverse reactions leading to dose modification were rash (13%), diarrhea (10%), and asthenia (3.6%). Selected, common adverse reactions in Study 4, occurring in at least 10% of patients who received Erlotinib or chemotherapy and an increase in ≥ 5% in the Erlotinib treated group, are summarized by NCI-CTC (version 3.0) Grade in Table 1. The median duration of Erlotinib treatment was 9.6 months in Study 4.
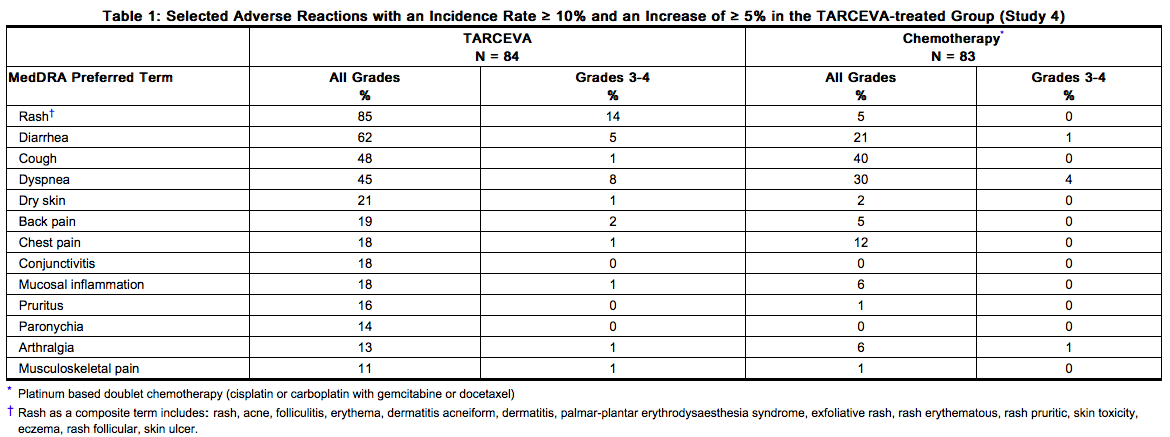
Hepatic Toxicity: One Erlotinib-treated patient experienced fatal hepatic failure and four additional patients experienced grade 3-4 liver test abnormalities in Study 4
Maintenance Treatment
Adverse reactions, regardless of causality, that occurred in at least 3% of patients treated with single-agent Erlotinib at 150 mg and at least 3% more often than in the placebo group in the randomized maintenance trial (Study 3) are summarized by NCI-CTC (version 3.0) Grade in Table 2. The most common adverse reactions in patients receiving single-agent Erlotinib 150 mg were rash and diarrhea. Grade 3-4 rash and diarrhea occurred in 9% and 2%, respectively, in Erlotinib-treated patients. rash and diarrhea resulted in study discontinuation in 1% and 0.5% of Erlotinib-treated patients, respectively. Dose reduction or interruption for rash and diarrhea was needed in 5% and 3% of patients, respectively. In Erlotinib-treated patients the median time to onset of rash was 10 days, and the median time to onset of diarrhea was 15 days.
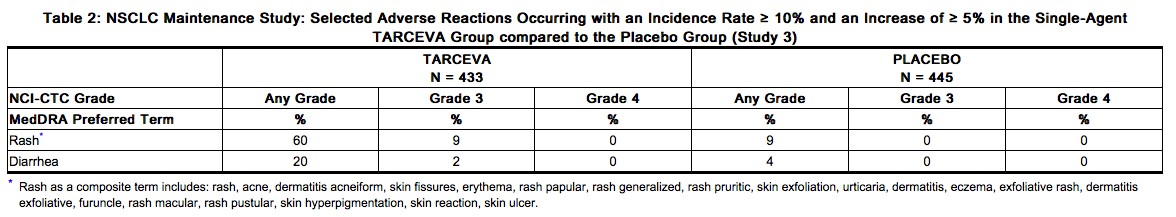
Liver test abnormalities including ALT elevations were observed at Grade 2 or greater severity in 3% of Erlotinib-treated patients and 1% of placebo-treated patients. Grade 2 and above bilirubin elevations were observed in 5% of Erlotinib-treated patients and in < 1% in the placebo group.
Second/Third Line Treatment
Adverse reactions, regardless of causality, that occurred in at least 10% of patients treated with single-agent Erlotinib at 150 mg and at least 5% more often than in the placebo group in the randomized trial of patients with NSCLC are summarized by NCI-CTC (version 2.0) Grade in Table 3. The most common adverse reactions in this patient population were rash and diarrhea. Grade 3-4 rash and diarrhea occurred in 9% and 6%, respectively, in Erlotinib-treated patients. rash and diarrhea each resulted in study discontinuation in 1% of Erlotinib-treated patients. Six percent and 1% of patients needed dose reduction for rash and diarrhea, respectively. The median time to onset of rash was 8 days, and the median time to onset of diarrhea was 12 days.
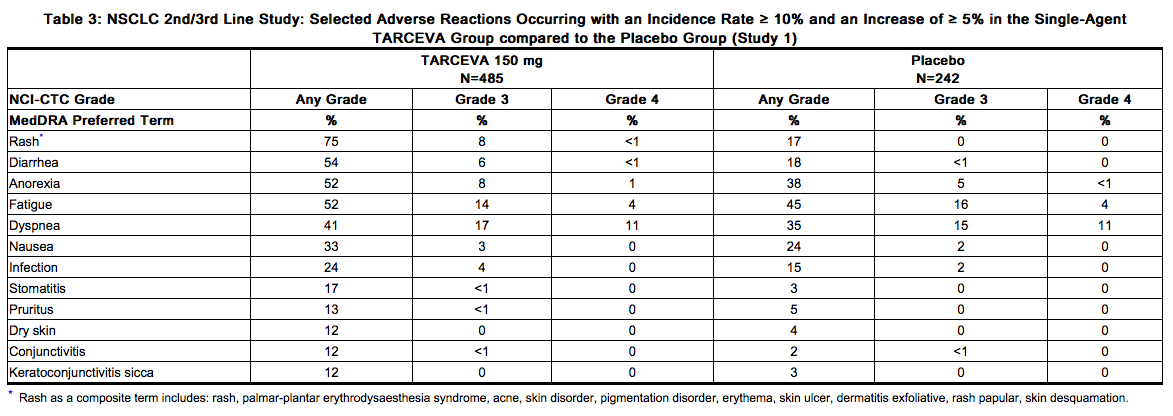
Liver function test abnormalities (including elevated alanine aminotransferase (ALT), aspartate aminotransferase (AST) and bilirubin) were observed in patients receiving single-agent Erlotinib 150 mg. These elevations were mainly transient or associated with liver metastases. Grade 2 (> 2.5 – 5.0 x ULN) ALT elevations occurred in 4% and < 1% of Erlotinib and placebo treated patients, respectively. Grade 3 (> 5.0 – 20.0 x ULN) elevations were not observed in Erlotinib-treated patients. Erlotinib dosing should be interrupted or discontinued if changes in liver function are severe
Pancreatic Cancer - Erlotinib Administered Concurrently with gemcitabine
This was a randomized, double blind placebo-controlled study of Erlotinib (150 mg or 100 mg daily) or placebo plus gemcitabine (1000 mg/m2 IV) in patients with locally advanced, unresectable or metastatic pancreatic cancer (Study 2). The safety population comprised 282 patients in the erlotinib group (259 in the 100 mg cohort and 23 in the 150 mg cohort) and 280 patients in the placebo group (256 in the 100 mg cohort and 24 in the 150 mg cohort). Adverse reactions that occurred in at least 10% of patients treated with Erlotinib 100 mg plus gemcitabine in the randomized trial of patients with pancreatic cancer (Study 2) are summarized by NCI-CTC (version 2.0) Grade in Table 4. The most common adverse reactions in pancreatic cancer patients receiving Erlotinib 100 mg plus gemcitabine were fatigue, rash, nausea, anorexia and diarrhea. In the Erlotinib plus gemcitabine arm, Grade 3-4 rash and diarrhea were each reported in 5% of patients. The median time to onset of rash and diarrhea was 10 days and 15 days, respectively. rash and diarrhea each resulted in dose reductions in 2% of patients, and resulted in study discontinuation in up to 1% of patients receiving Erlotinib plus gemcitabine. Severe adverse reactions (≥ Grade 3 NCI-CTC) in the Erlotinib plus gemcitabine group with incidences < 5% included syncope, arrhythmias, ileus, pancreatitis, hemolytic anemia including microangiopathic hemolytic anemia with thrombocytopenia, myocardial infarction/ischemia, cerebrovascular accidents including cerebral hemorrhage, and renal insufficiency The 150 mg cohort was associated with a higher rate of certain class-specific adverse reactions including rash and required more frequent dose reduction or interruption.
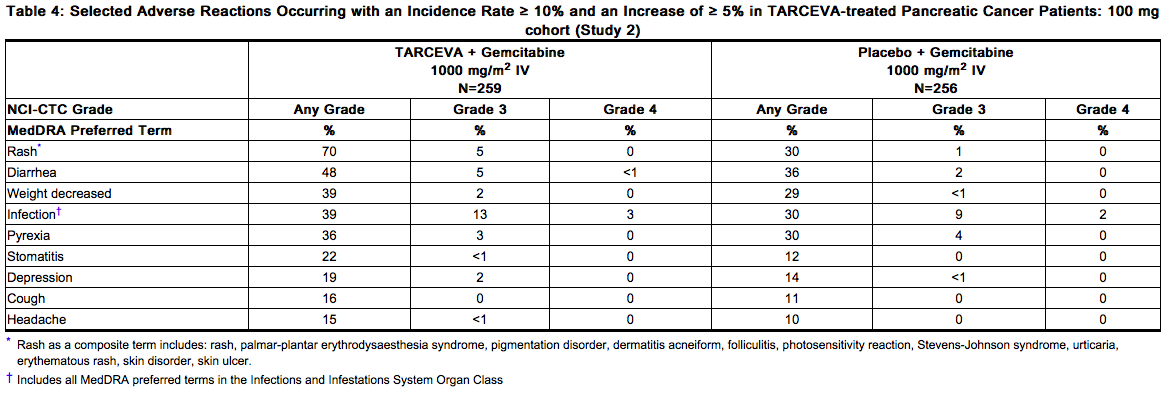
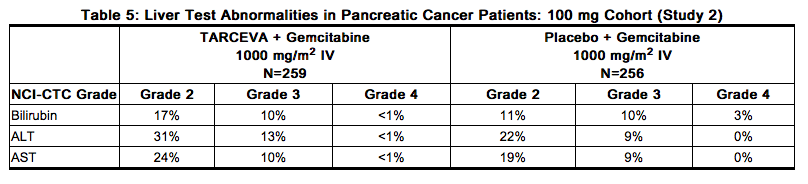
Ten patients (4%) in the Erlotinib/gemcitabine group and three patients (1%) in the placebo/gemcitabine group developed deep venous thrombosis. The overall incidence of grade 3 or 4 thrombotic events, including deep venous thrombosis was 11% for Erlotinib plus gemcitabine and 9% for placebo plus gemcitabine. The incidences of liver test abnormalities (≥ Grade 2) in Study 2 are provided in Table 5
NSCLC and Pancreatic Indications: Selected Low Frequency Adverse Reactions
Gastrointestinal Disorders
Cases of gastrointestinal bleeding (including fatalities) have been reported, some associated with concomitant warfarin or NSAID administration . These adverse reactions were reported as peptic ulcer bleeding (gastritis, gastroduodenal ulcers), hematemesis, hematochezia, melena and hemorrhage from possible colitis.
Postmarketing Experience
The following adverse reactions have been identified during post approval use of Erlotinib. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Musculoskeletal and Connective Tissue Disorders: myopathy, including rhabdomyolysis, in combination with statin therapy. Eye Disorders: ocular inflammation including uveitis.
Drug Interactions
CYP3A4 Inhibitors
Erlotinib is metabolized predominantly by CYP3A4. Co-treatment with the potent CYP3A4 inhibitor ketoconazole increased erlotinib AUC by 67%. When Erlotinib was co-administered with ciprofloxacin, an inhibitor of both CYP3A4 and CYP1A2, the erlotinib exposure [AUC] and maximum concentration [Cmax] increased by 39% and 17%, respectively. Dose modifications are recommended.
CYP3A4 Inducers
Pre-treatment with the CYP3A4 inducer rifampicin for 7-11 days prior to Erlotinib decreased erlotinib AUC by 58% to 80%. Dose modifications are recommended. Drugs Affecting Gastric pH
Co-administration of Erlotinib with omeprazole decreased erlotinib AUC by 46% and co-administration of Erlotinib with ranitidine 300 mg decreased erlotinib AUC by 33%. When Erlotinib was administered with ranitidine 150 mg twice daily (at least 10 h after the previous ranitidine evening dose and 2 h before the ranitidine morning dose), erlotinib AUC decreased by 15%. Increasing the dose of Erlotinib when co-administered with such agents is not likely to compensate for the loss of exposure. Scheduling modifications are recommended.
Cigarette Smoking
Cigarette smoking results in reductions in erlotinib AUC. Dose modifications are recommended. Anticoagulants
Interaction with coumarin-derived anticoagulants, including warfarin, leading to increased International Normalized Ratio (INR) and bleeding adverse reactions, which in some cases were fatal, have been reported in patients receiving Erlotinib. Regularly monitor prothrombin time or INR in patients taking coumarin-derived anticoagulants. Dose modifications of Erlotinib are not recommended
Use in Specific Populations
Pregnancy
Pregnancy Category (FDA): D Risk Summary
Based on its mechanism of action, Erlotinib can cause fetal harm when administered to a pregnant woman. When given during organogenesis, erlotinib administration resulted in embryo-fetal lethality and abortion in rabbits at doses approximately 3 times the recommended human daily dose of 150 mg. If Erlotinib is used during pregnancy, or if the patient becomes pregnant while taking this drug, the patient should be apprised of the potential hazard to a fetus
Animal Data
Erlotinib has been shown to cause maternal toxicity resulting in embryo-fetal lethality and abortion in rabbits when given during the period of organogenesis at doses that result in plasma drug concentrations approximately 3 times those achieved at the recommended dose in humans (AUCs at 150 mg daily dose). During the same period, there was no increase in the incidence of embryo-fetal lethality or abortion in rabbits or rats at doses resulting in exposures approximately equal to those in humans at the recommended daily dose. In an independent fertility study female rats treated with 30 mg/m2/day or 60 mg/m2/day (0.3 or 0.7 times the recommended daily dose, on a mg/m2 basis) of erlotinib had an increase in early resorptions that resulted in a decrease in the number of live fetuses.
No teratogenic effects were observed in rabbits or rats dosed with erlotinib during organogenesis at doses up to 600 mg/m2/day in the rabbit (3 times the plasma drug concentration seen in humans at 150 mg/day) and up to 60 mg/m2/day in the rat (0.7 times the recommended dose of 150 mg/day on a mg/m2 basis).
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Erlotinib in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Erlotinib during labor and delivery.
Nursing Mothers
It is not known whether erlotinib is present in human milk. Because many drugs are present in human milk and because of the potential for serious adverse reactions in nursing infants from Erlotinib, a decision should be made whether to discontinue nursing or discontinue the drug, taking into account the importance of the drug to the mother.
Pediatric Use
The safety and effectiveness of Erlotinib in pediatric patients have not been established.
Geriatic Use
Of the 1297 subjects in clinical studies of Erlotinib for the treatment of NSCLC and pancreatic cancer 40% were 65 and older while 10% were 75 and older. No overall differences in safety or efficacy were observed between subjects 65 years and older and those younger than 65.
Gender
There is no FDA guidance on the use of Erlotinib with respect to specific gender populations.
Race
There is no FDA guidance on the use of Erlotinib with respect to specific racial populations.
Renal Impairment
Less than 9% of a single dose is excreted in the urine. No clinical studies have been conducted in patients with compromised renal function.
Hepatic Impairment
Patients with hepatic impairment (total bilirubin > upper limit of normal (ULN) or Child-Pugh A, B and C) should be closely monitored during therapy with Erlotinib. Treatment with Erlotinib should be used with extra caution in patients with total bilirubin > 3 x ULN In vitro and in vivo evidence suggest that erlotinib is cleared primarily by the liver. However, erlotinib exposure was similar in patients with moderately impaired hepatic function (Child-Pugh B) compared with patients with adequate hepatic function including patients with primary liver cancer or hepatic metastases
Females of Reproductive Potential and Males
Contraception
Females
Counsel patients on pregnancy planning and prevention. Advise female patients of reproductive potential to use highly effective contraception during treatment with Erlotinib, and for at least 2 weeks after the last dose of Erlotinib. Advise patients to contact their healthcare provider if they become pregnant, or if pregnancy is suspected, while taking Erlotinib
Immunocompromised Patients
There is no FDA guidance one the use of Erlotinib in patients who are immunocompromised.
Administration and Monitoring
Administration
Oral
Monitoring
FDA Package Insert for Erlotinib contains no information regarding drug monitoring.
IV Compatibility
There is limited information about the IV Compatibility
Overdosage
Single oral doses of Erlotinib up to 1,000 mg in healthy subjects and weekly doses up to 1,600 mg in cancer patients have been tolerated. Repeated twice-daily doses of 200 mg single-agent Erlotinib in healthy subjects were poorly tolerated after only a few days of dosing. Based on the data from these studies, an unacceptable incidence of severe adverse reactions, such as diarrhea, rash, and liver transaminase elevation, may occur above the recommended dose . In case of suspected overdose, Erlotinib should be withheld and symptomatic treatment instituted.
Pharmacology
Mechanism of Action
Epidermal growth factor receptor (EGFR) is expressed on the cell surface of both normal and cancer cells. In some tumor cells signaling through this receptor plays a role in tumor cell survival and proliferation irrespective of EGFR mutation status. Erlotinib reversibly inhibits the kinase activity of EGFR, preventing autophosphorylation of tyrosine residues associated with the receptor and thereby inhibiting further downstream signaling. Erlotinib binding affinity for EGFR exon 19 deletion or exon 21 (L858R) mutations is higher than its affinity for the wild type receptor. Erlotinib inhibition of other tyrosine kinase receptors has not been fully characterized.
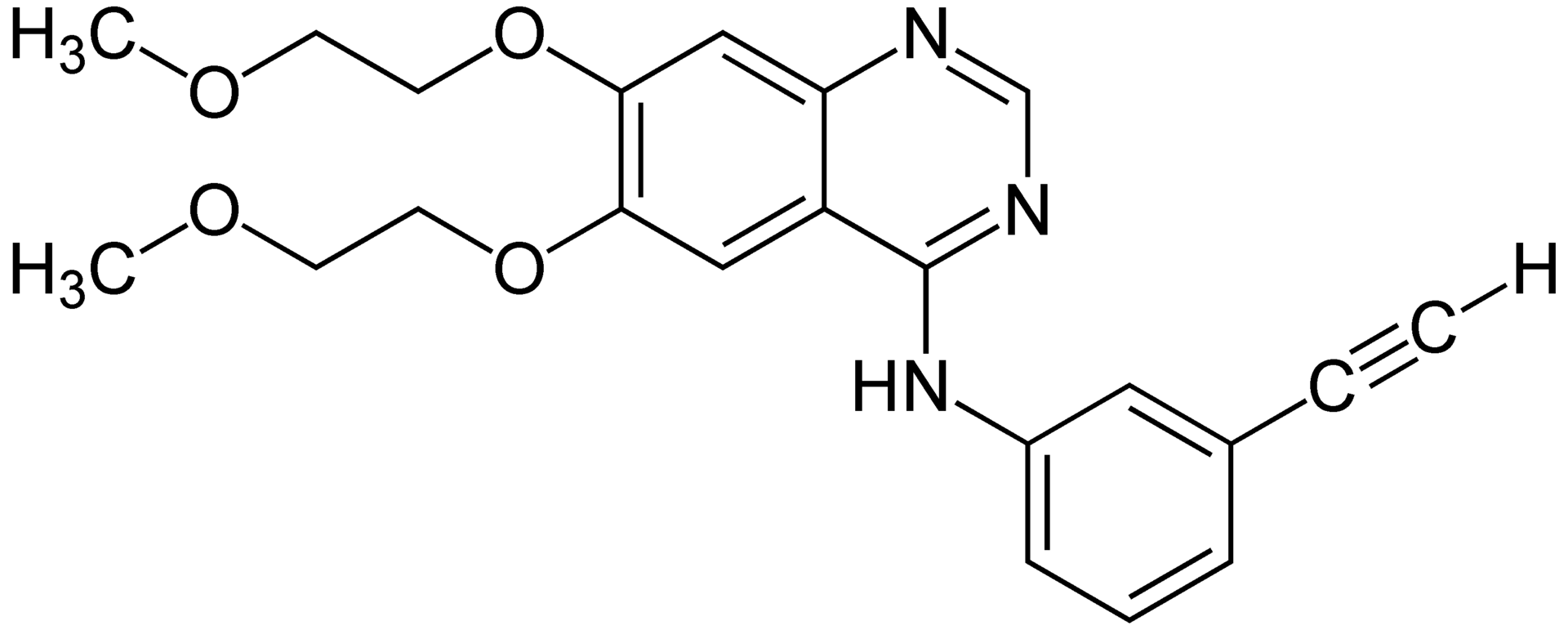
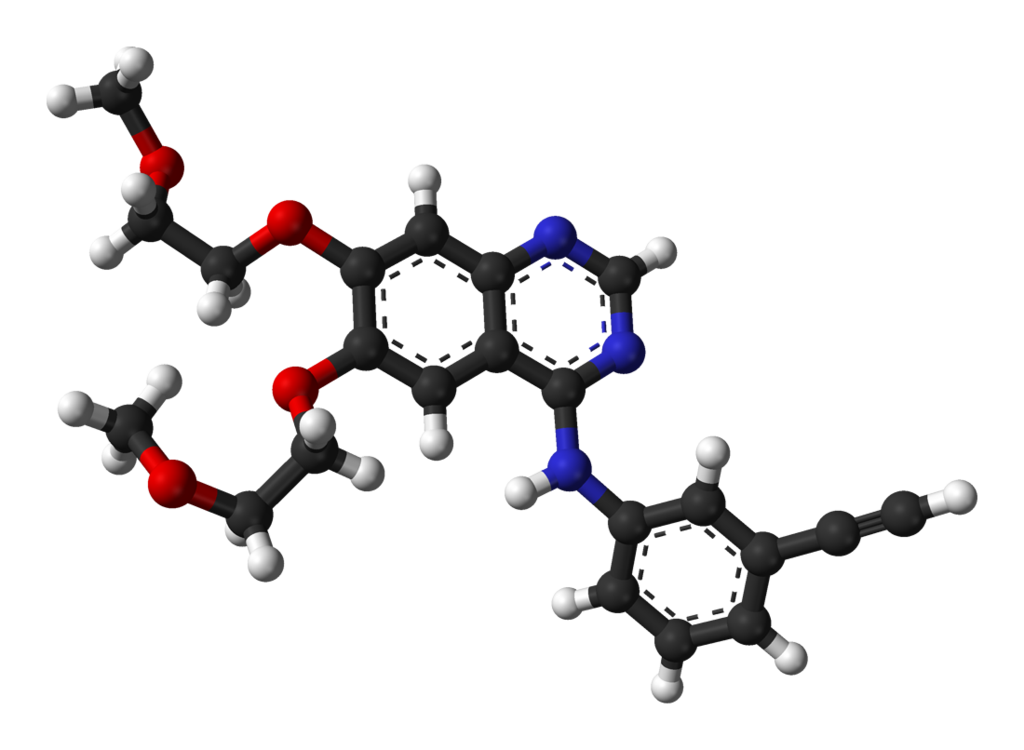
Structure
Erlotinib (erlotinib), a kinase inhibitor, is a quinazolinamine with the chemical name N-(3-ethynylphenyl)-6,7-bis(2-methoxyethoxy)-4-quinazolinamine. Erlotinib contains erlotinib as the hydrochloride salt that has the following structural formula:
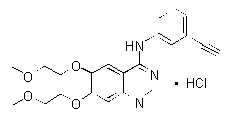
Erlotinib hydrochloride has the molecular formula C22H23N3O4.HCl and a molecular weight of 429.90. The molecule has a pKa of 5.42 at 25oC. Erlotinib hydrochloride is very slightly soluble in water, slightly soluble in methanol and practically insoluble in acetonitrile, acetone, ethyl acetate and hexane. Aqueous solubility of erlotinib hydrochloride is dependent on pH with increased solubility at a pH of less than 5 due to protonation of the secondary amine. Over the pH range of 1.4 to 9.6, maximal solubility of approximately 0.4 mg/mL occurs at a pH of approximately 2. Erlotinib tablets for oral administration are available in three dosage strengths containing erlotinib hydrochloride (27.3 mg, 109.3 mg and 163.9 mg) equivalent to 25 mg, 100 mg and 150 mg erlotinib and the following inactive ingredients: lactose monohydrate, hypromellose, hydroxypropyl cellulose, magnesium stearate, microcrystalline cellulose, sodium starch glycolate, sodium lauryl sulfate and titanium dioxide. The tablets also contain trace amounts of color additives, including FD&C Yellow #6 (25 mg only) for product identification.
Pharmacodynamics
There is limited information regarding Erlotinib Pharmacodynamics in the drug label.
Pharmacokinetics
Absorption and Distribution:
Erlotinib is about 60% absorbed after oral administration and its bioavailability is substantially increased by food to almost 100%. Peak plasma levels occur 4 hours after dosing. The solubility of erlotinib is pH dependent. Erlotinib solubility decreases as pH increases. Co-administration of Erlotinib with omeprazole, a proton pump inhibitor, decreased the erlotinib exposure [AUC] and maximum concentration [Cmax] by 46% and 61%, respectively. When Erlotinib was administered 2 hours following a 300 mg dose of ranitidine, an H2 receptor antagonist, the erlotinib AUC was reduced by 33% and Cmax by 54%. When Erlotinib was administered with ranitidine 150 mg twice daily (at least 10 h after the previous ranitidine evening dose and 2 h before the ranitidine morning dose), the erlotinib AUC and Cmax decreased by 15% and 17%, respectively. Following absorption, erlotinib is approximately 93% protein bound to plasma albumin and alpha-1 acid glycoprotein (AAG). Erlotinib has an apparent volume of distribution of 232 liters.
Metabolism and Excretion:
A population pharmacokinetic analysis in 591 patients receiving the single-agent Erlotinib 2nd/3rd line regimen showed a median half-life of 36.2 hours. Time to reach steady state plasma concentration would therefore be 7 – 8 days. No significant relationships of clearance to covariates of patient age, body weight or gender were observed. Smokers had a 24% higher rate of erlotinib clearance. An additional population pharmacokinetic analysis was conducted in 291 NSCLC patients administered single-agent erlotinib as maintenance treatment. This analysis demonstrated that covariates affecting erlotinib clearance in this patient population were similar to those seen in the prior single-agent pharmacokinetic analysis. No new covariate effects were identified. A third population pharmacokinetic analysis was conducted that incorporated erlotinib data from 204 pancreatic cancer patients who received erlotinib plus gemcitabine. Similar results were observed to those seen in the prior single-agent pharmacokinetic analysis. No new covariate effects were identified. Co-administration of gemcitabine had no effect on erlotinib plasma clearance. In vitro assays of cytochrome P450 metabolism showed that erlotinib is metabolized primarily by CYP3A4 and to a lesser extent by CYP1A2, and the extrahepatic isoform CYP1A1. Following a 100 mg oral dose, 91% of the dose was recovered: 83% in feces (1% of the dose as intact parent) and 8% in urine (0.3% of the dose as intact parent). Cigarette smoking reduces erlotinib exposure. In the Phase 3 NSCLC trial, current smokers achieved erlotinib steady-state trough plasma concentrations which were approximately 2-fold less than the former smokers or patients who had never smoked. This effect was accompanied by a 24% increase in apparent erlotinib plasma clearance. In a separate study which evaluated the single-dose pharmacokinetics of erlotinib in healthy volunteers, current smokers cleared the drug faster than former smokers or volunteers who had never smoked. The AUC0-infinity in smokers was about 1/3 to 1/2 of that in never/former smokers. In another study which was conducted in NSCLC patients (N=35) who were current smokers, pharmacokinetic analyses at steady-state indicated a dose-proportional increase in erlotinib exposure when the Erlotinib dose was increased from 150 mg to 300 mg. However, the exact dose to be recommended for patients who currently smoke is unknown.
Special Populations:
Patients with Hepatic Impairment
hepatic failure and hepatorenal syndrome, including fatal cases, can occur with Erlotinib treatment in patients with normal hepatic function; the risk of hepatic toxicity is increased in patients with baseline hepatic impairment. In vitro and in vivo evidence suggest that erlotinib is cleared primarily by the liver. However, erlotinib exposure was similar in patients with moderately impaired hepatic function (Child-Pugh B) compared with patients with adequate hepatic function including patients with primary liver cancer or hepatic metastases.
Patients with Renal Impairment
Less than 9% of a single dose is excreted in the urine. No clinical studies have been conducted in patients with compromised renal function.
Nonclinical Toxicology
]Carcinogenesis, Mutagenesis, Impairment of Fertility
Two-year carcinogenicity studies were conducted in mice and rats with erlotinib at oral doses of up to 60 mg/kg/day in mice, 5 mg/kg/day in female rats, and 10 mg/kg/day in male rats. The studies were negative for carcinogenic findings. Exposure in mice at the highest dose tested was approximately 10 times the exposure in humans at the erlotinib dose of 150 mg/day. The highest dose evaluated in male rats resulted in exposures that were twice those in humans and exposures at the highest tested dose in female rats were slightly lower than those in humans. Erlotinib did not cause genetic damage in a series of in vitro assays (bacterial mutation, human lymphocyte chromosome aberration and mammalian cell mutation) and in the in vivo mouse bone marrow micronucleus test. Erlotinib did not impair fertility in either male or female rats.
Clinical Studies
Non-Small Cell Lung Cancer (NSCLC) – First-Line Treatment of Patients with EGFR Mutations
The safety and efficacy of Erlotinib as monotherapy for the first-line treatment of patients with metastatic NSCLC containing EGFR exon 19 deletions or exon 21 (L858R) substitution mutations was demonstrated in a randomized, open-label, clinical trial conducted in Europe (Study 4). One hundred seventy-four (174) White patients were randomized 1:1 to receive erlotinib 150 mg once daily until disease progression (n=86) or four cycles of a standard platinum-based doublet chemotherapy (n=88); standard chemotherapy regimens were cisplatin plus gemcitabine, cisplatin plus docetaxel, carboplatin plus gemcitabine, and carboplatin plus docetaxel. The main efficacy outcome measure was progression-free survival (PFS) as assessed by the investigator. Randomization was stratified by EGFR mutation (exon 19 deletion or exon 21 (L858R) substitution) and ECOG PS (0 vs. 1 vs. 2). EGFR mutation status for screening and enrollment of patients was determined by a clinical trials assay (CTA). Tumor samples from 134 patients (69 patients from the erlotinib arm and 65 patients from the chemotherapy arm) were tested retrospectively by the FDA-approved companion diagnostic, the cobas® EGFR Mutation Test. The baseline demographics of the overall study population were as follows: female (72%), white (99%), age ≥ 65 years (51%), ECOG PS 1 (53%), with ECOG PS 0 (33%), and ECOG PS 2 (14%), current smoker (11%), past-smoker (20%), and never smoker (69%). The disease characteristics were 93% stage IV and 7% Stage IIIb with pleural effusion as classified by the American Joint Commission on Cancer (AJCC, 6th edition), 93% adenocarcinoma histology, 66% exon 19 mutation deletions and 34% exon 21 (L858R) point mutation by a CTA. A statistically significant improvement in investigator-determined PFS was demonstrated for patients randomized to erlotinib compared to those randomized chemotherapy. Similar results for PFS were observed for the subgroup evaluated by an independent-review committee (approximately 75% of patients in Study 4 evaluated) and in the subgroup of 134 patients (77% of the Study 4 population) with EGFR mutations confirmed by the cobas® EGFR Mutation Test. A protocol-specified analysis of overall survival conducted at the time of the final analysis of PFS showed no statistically significant difference between the Erlotinib and chemotherapy arms. At the time of the data cut-off, 84% of patients in the chemotherapy arm had received at least one subsequent treatment, of whom 97% received an EGFR tyrosine kinase inhibitor. In the Erlotinib arm, 66% of patients had received at least one subsequent treatment.
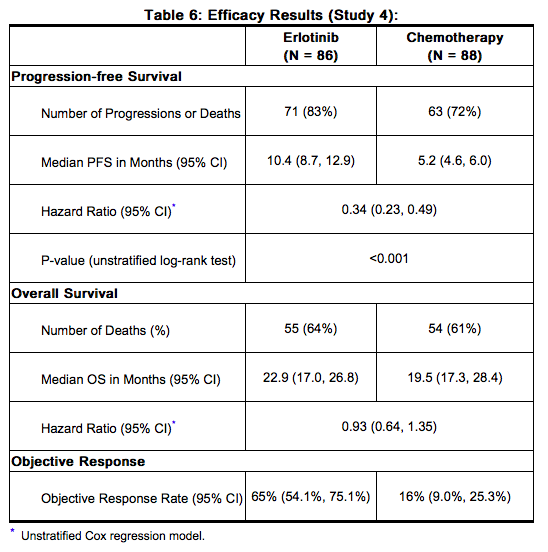
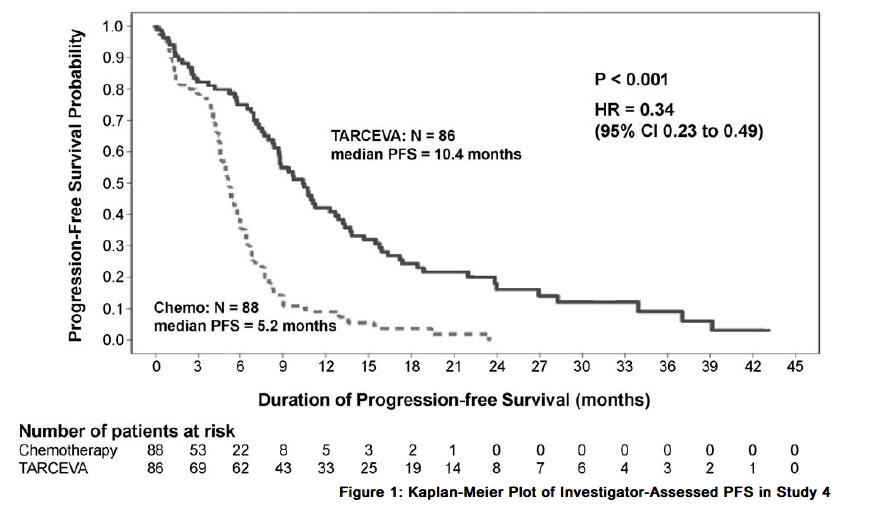
In exploratory subgroup analyses based on EGFR mutation subtype, the hazard ratio (HR) for PFS was 0.27 (95% CI 0.17 to 0.43) in patients with exon 19 deletions and 0.52 (95% CI 0.29 to 0.95) in patients with exon 21 (L858R) substitution. The HR for OS was 0.94 (95% CI 0.57 to 1.54) in the exon 19 deletion subgroup and 0.99 (95% CI 0.56 to 1.76) in the exon 21 (L858R) substitution subgroup.
NSCLC - Maintenance Treatment
The efficacy and safety of Erlotinib as maintenance treatment of NSCLC were demonstrated in a randomized, double-blind, placebo-controlled trial conducted in 26 countries, in 889 patients with locally advanced or metastatic NSCLC whose disease did not progress during first-line platinum-based chemotherapy (Study 3). Patients were randomized 1:1 to receive Erlotinib 150 mg or placebo orally once daily (438 Erlotinib, 451 placebo) until disease progression or unacceptable toxicity. The primary objective of the study was to determine if the administration of Erlotinib after standard platinum-based chemotherapy in the treatment of NSCLC resulted in improved progression free survival (PFS) when compared with placebo, in all patients or in patients with EGFR immunohistochemistry (IHC) positive tumors. Demographic characteristics were balanced between the two treatment groups. Baseline demographics of the overall study population were as follows: male (74%), age < 65 years (66%), ECOG PS 1 (69%), ECOG PS 0 (31%), white (84%), Asian (15%), current smoker (55%), past-smoker (27%), and never smoker (17%). Disease characteristics were as follows: Stage IV (75%), Stage IIIb with effusion (25%) as classified by AJCC (6th edition) with histologic subtypes of adenocarcinoma including bronchioalveolar (45%), squamous (40%) and large cell (5%); and EGFR IHC positive (70%), negative (14%), indeterminate (4%), and missing (12%).

Figure 2 depicts the Kaplan-Meier Curves for Overall Survival (ITT Population).
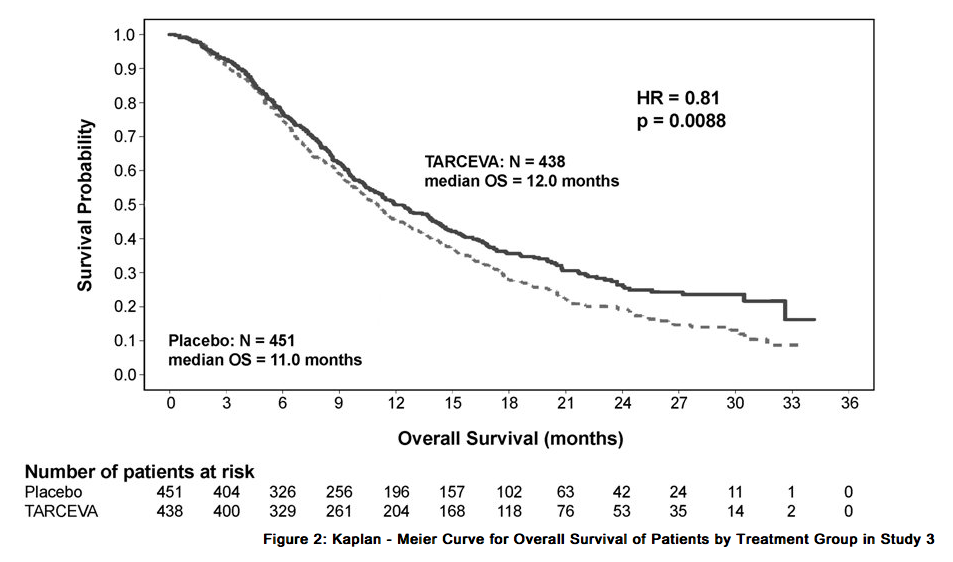
Note: HR is from a univariate Cox regression model. The PFS and OS Hazard Ratios, respectively, in patients with EGFR IHC-positive tumors were 0.69 (95% CI: 0.58, 0.82) and 0.77 (95% CI: 0.64, 0.93). The PFS and OS Hazard Ratios in patients with IHC-negative tumors were 0.77 (95% CI: 0.51, 1.14) and 0.91 (95% CI: 0.59, 1.38), respectively. Patients with adenocarcinoma had an OS Hazard Ratio of 0.77 (95% CI: 0.61, 0.97) and patients with squamous histology had an OS Hazard Ratio of 0.86 (95% CI: 0.68, 1.10).
NSCLC –Second/Third Line Treatment
The efficacy and safety of single-agent Erlotinib was assessed in a randomized, double blind, placebo-controlled trial in 731 patients with locally advanced or metastatic NSCLC after failure of at least one chemotherapy regimen (Study 1). Patients were randomized 2:1 to receive Erlotinib 150 mg or placebo (488 Erlotinib, 243 placebo) orally once daily until disease progression or unacceptable toxicity. Study endpoints included overall survival, response rate, and progression-free survival (PFS). Duration of response was also examined. The primary endpoint was survival. The study was conducted in 17 countries. Baseline demographics of the overall study population were as follows: male (65%), white (78%), Asian (12%), black (4%), age < 65 years (62%), ECOG PS 1 (53%), ECOG PS 0 (13%), ECOG PS 2 (25%), ECOG PS 3 (9%), current or ex-smoker (75%), never smoker (20%), and exposure to prior platinum therapy (93%). Tumor characteristics were as follows: adenocarcinoma (50%), squamous (30%), undifferentiated large cell (9%), and mixed non-small cell (2%). The results of the study are shown in Table 8.
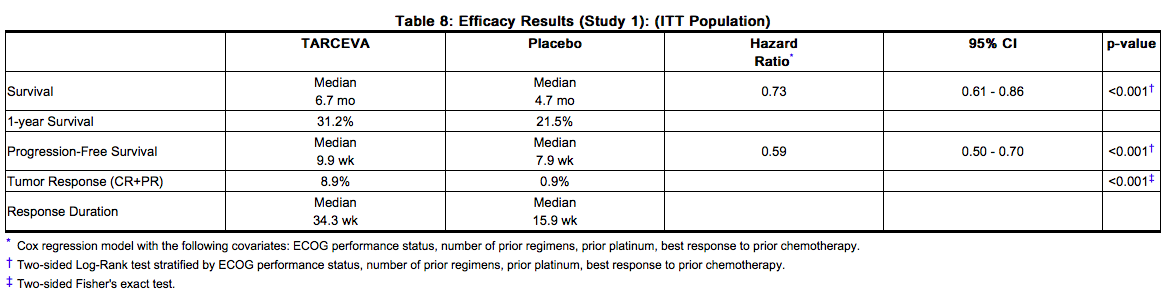
Survival was evaluated in the intent-to-treat population. Figure 3 depicts the Kaplan-Meier curves for overall survival. The primary survival and PFS analyses were two-sided Log-Rank tests stratified by ECOG performance status, number of prior regimens, prior platinum, best response to prior chemotherapy.
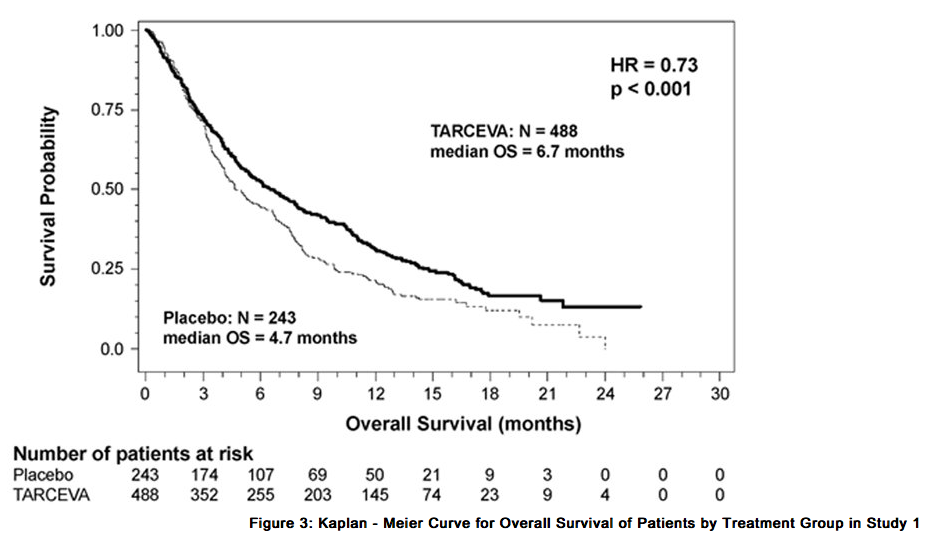
Note: HR is from Cox regression model with the following covariates: ECOG performance status, number of prior regimens, prior platinum, best response to prior chemotherapy. P-value is from two-sided Log-Rank test stratified by ECOG performance status, number of prior regimens, prior platinum, best response to prior chemotherapy.
NSCLC – Lack of Efficacy of Erlotinib Administered Concurrently with Chemotherapy
Results from two, multicenter, placebo-controlled, randomized, trials in over 1000 patients conducted in first-line patients with locally advanced or metastatic NSCLC showed no clinical benefit with the concurrent administration of Erlotinib with platinum-based chemotherapy [carboplatin and paclitaxel (Erlotinib, N = 526) or gemcitabine and cisplatin (Erlotinib, N = 580)].
Pancreatic Cancer - Erlotinib Administered Concurrently with gemcitabine
The efficacy and safety of Erlotinib in combination with gemcitabine as a first-line treatment was assessed in a randomized, double blind, placebo-controlled trial in 569 patients with locally advanced, unresectable or metastatic pancreatic cancer (Study 2). Patients were randomized 1:1 to receive Erlotinib (100 mg or 150 mg) or placebo once daily on a continuous schedule plus gemcitabine IV (1000 mg/m2, Cycle 1 - Days 1, 8, 15, 22, 29, 36 and 43 of an 8 week cycle; Cycle 2 and subsequent cycles - Days 1, 8 and 15 of a 4-week cycle. Erlotinib or placebo was taken orally once daily until disease progression or unacceptable toxicity. The primary endpoint was survival. Secondary endpoints included response rate, and progression-free survival (PFS). Duration of response was also examined. The study was conducted in 18 countries. A total of 285 patients were randomized to receive gemcitabine plus Erlotinib (261 patients in the 100 mg cohort and 24 patients in the 150 mg cohort) and 284 patients were randomized to receive gemcitabine plus placebo (260 patients in the 100 mg cohort and 24 patients in the 150 mg cohort). Too few patients were treated in the 150 mg cohort to draw conclusions. In the 100 mg cohort, baseline demographics of the overall study population were as follows: male (52%), white (88%), Asian (7%), black (2%), age < 65 years (53%), ECOG PS 1 (51%), ECOG PS 0 (32%), and ECOG PS 2 (17%). There was a slightly larger proportion of females in the Erlotinib arm (51%) compared with the placebo arm (44%). The median time from initial diagnosis to randomization was approximately 1.0 month. The majority of the patients (76%) had distant metastases at baseline and 24% had locally advanced disease. The results of the study are shown in Table 9.
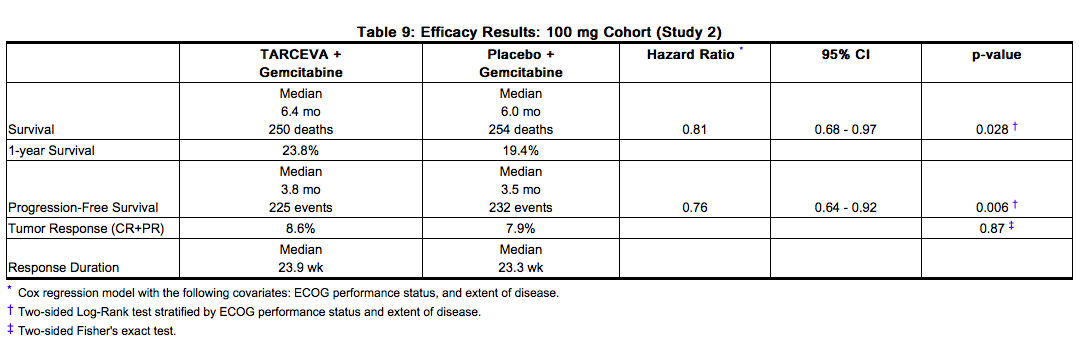
Survival was evaluated in the intent-to-treat population. Figure 4 depicts the Kaplan-Meier curves for overall survival in the 100 mg cohort. The primary survival and PFS analyses were two-sided Log-Rank tests stratified by ECOG performance status and extent of disease.
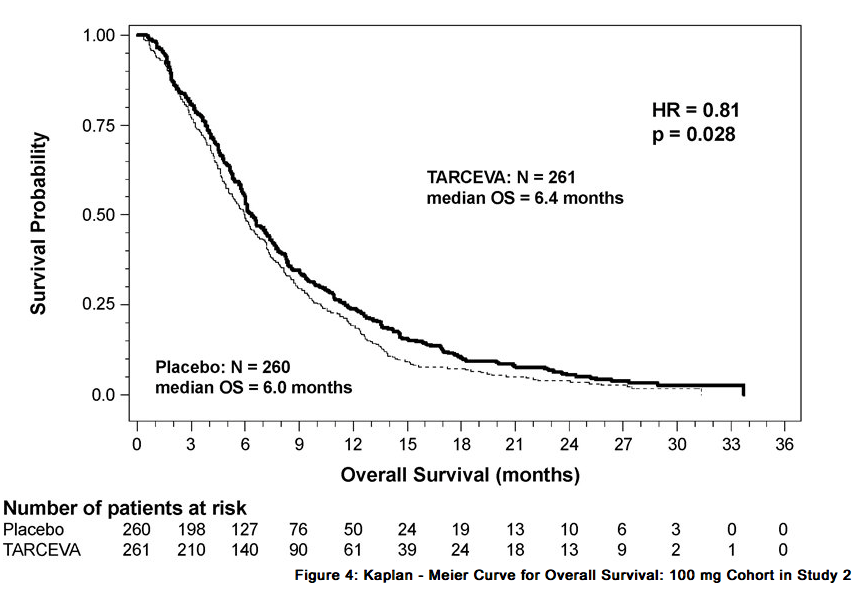
Note: HR is from Cox regression model with the following covariates: ECOG performance status and extent of disease. The p-value is from two-sided Log-Rank test stratified by ECOG performance status and extent of disease.
How Supplied
25 mg Tablets Round, biconvex face and straight sides, white film-coated, printed in orange with a “T” and “25” on one side and plain on the other side; supplied in: Bottles of 30: NDC 50242-062-01 100 mg Tablets Round, biconvex face and straight sides, white film-coated, printed in gray with “T” and “100” on one side and plain on the other side; supplied in: Bottles of 30: NDC 50242-063-01 150 mg Tablets Round, biconvex face and straight sides, white film-coated, printed in maroon with “T” and “150” on one side and plain on the other side; supplied in: Bottles of 30: NDC 50242-064-01
Storage
Store at 25°C (77°F); excursions permitted to 15°C - 30°C (59°F - 86°F). See USP Controlled Room Temperature.
Images
Drug Images
{{#ask: Page Name::Erlotinib |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
{{#ask: Label Page::Erlotinib |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
Advise patients to contact their health care provider for:
- Onset or worsening of unexplained shortness of breath or cough
- Eye irritation
- Onset or worsening of skin rash or development of bullous lesions or desquamation.
- Any changes in smoking status
Advise patients on the presentation of skin, hair and nail disorders.
- In patients who develop skin rash, the appearance of the rash is typically erythematous and maculopapular and it may resemble acne with follicular pustules, but is histopathologically different. This skin reaction commonly occurs on the face, upper chest and back, but may be more generalized or severe (NCI-CTC Grade 3 or 4) with desquamation. Skin reactions may occur or worsen in sun exposed areas. Symptoms associated with rash may include itching, tenderness and/or burning.
- Hyperpigmentation or dry skin, with or without digital skin fissures, have been reported and in the majority of cases were associated with rash.
- Hair and nail disorders, including hirsutism and brittle and loose nails, have been reported.
Instruct patients on initial management of rash or diarrhea.
- Given that skin reactions are anticipated when taking Erlotinib, proactive intervention may include alcohol-free emollient cream and use of sunscreen or avoidance of sun exposure
- Management of rash may include topical corticosteroids or antibiotics with anti-inflammatory properties. These approaches were used in the NSCLC and pancreatic pivotal clinical trials. Acne preparations with drying properties may aggravate the dry skin and erythema. Treatment of rash has not been formally studied and should be based on rash severity.
- Diarrhea can usually be managed with loperamide.
Counsel patients on pregnancy planning and prevention.
- Advise females of reproductive potential to use highly effective contraception during treatment with Erlotinib, and for at least 2 weeks after the last dose of Erlotinib.
- Advise patients to contact their healthcare provider if they become pregnant, or if pregnancy is suspected, during treatment with Erlotinib.
- Advise breast-feeding mothers to discontinue nursing while receiving Erlotinib .
Advise patients to stop smoking. Advise patients that the dose of Erlotinib may need to be adjusted if they smoke.
Precautions with Alcohol
Alcohol-Erlotinib interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
- Tarceva
Look-Alike Drug Names
There is limited information regarding Erlotinib Look-Alike Drug Names in the drug label.
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
{{#subobject:
|Page Name=Erlotinib |Pill Name=Erlotinib_25 mg_NDC 50242-062.jpg |Drug Name=Tarceva 25 MG Oral Tablet |Pill Ingred=ERLOTINIB HYDROCHLORIDE|+sep=; |Pill Imprint=T;25 |Pill Dosage=25 mg |Pill Color=White|+sep=; |Pill Shape=Round |Pill Size (mm)=6.00 |Pill Scoring=1 |Pill Image= |Drug Author=Genentech, Inc. |NDC=50242-062
}}
{{#subobject:
|Page Name=Erlotinib |Pill Name=Erlotinib_100 mg_NDC 50242-063.jpg |Drug Name=Tarceva 100 MG Oral Tablet |Pill Ingred=ERLOTINIB HYDROCHLORIDE|+sep=; |Pill Imprint=T;100 |Pill Dosage=100 mg |Pill Color=White|+sep=; |Pill Shape=Round |Pill Size (mm)=9.00 |Pill Scoring=1 |Pill Image= |Drug Author=Genentech, Inc. |NDC=50242-063
}}
{{#subobject:
|Page Name=Erlotinib |Pill Name=Erlotinib_100 mg_NDC 50242-064.jpg |Drug Name=Tarceva 150 MG Oral Tablet |Pill Ingred=ERLOTINIB HYDROCHLORIDE|+sep=; |Pill Imprint=T;150 |Pill Dosage=150 mg |Pill Color=White|+sep=; |Pill Shape=Round |Pill Size (mm)=10.00 |Pill Scoring=1 |Pill Image= |Drug Author=Genentech, Inc. |NDC=50242-064
}}
{{#subobject:
|Label Page=Erlotinib |Label Name=Erlotinib_label_01.jpg
}}
{{#subobject:
|Label Page=Erlotinib |Label Name=Erlotinib_label_02.jpg
}}
{{#subobject:
|Label Page=Erlotinib |Label Name=Erlotinib_label_03.jpg
}}
{{#subobject:
|Label Page=Erlotinib |Label Name=Erlotinib_panel_01.png
}}
{{#subobject:
|Label Page=Erlotinib |Label Name=Erlotinib_panel_02.png
}}
{{#subobject:
|Label Page=Erlotinib |Label Name=Erlotinib_panel_03.png
}}