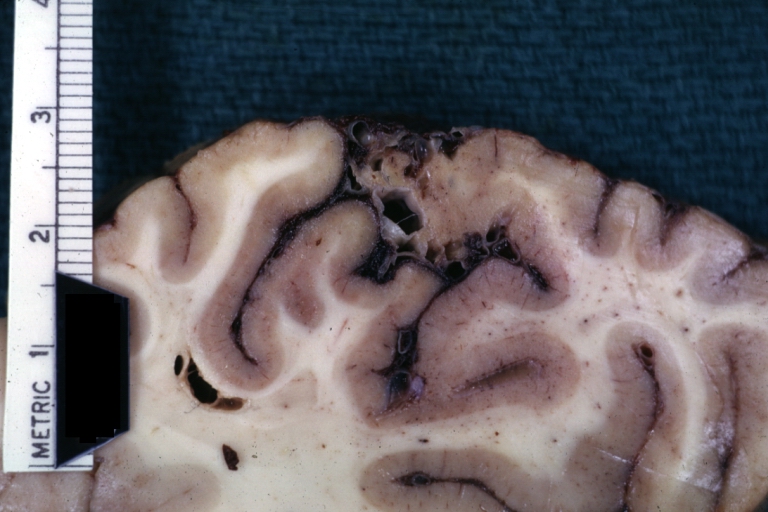
Cerebral arteriovenous malformation
| Cerebral arteriovenous malformation | |
 | |
|---|---|
| Brain: Arteriovenous Malformation: Gross fixed tissue close-up view of malformation in meninges and cerebral cortex. Image courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology |
For patient information click here
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Kalsang Dolma, M.B.B.S.[2],Seyedmahdi Pahlavani, M.D. [3]
Synonyms and keywords: Cerebral AVM, Brain AVM, Arteriovenous malformation of the brain
Overview
A cerebral arteriovenous malformation (AVM) is a congenital disorder of the blood vessels within the brain, characterized by the tangling of veins and arteries. While an arteriovenous malformation can occur elsewhere in the body, this article is concerned with malformations found in the brain.
Pathophysiology
AVMs are abnormal connections between the arteries and veins in the human brain. In a normal brain, oxygen enriched blood travels from the heart in sequence through smaller blood vessels going from arteries, to arterioles and then to the capillaries.[1] Oxygen is removed in the capillaries to be used by the brain.[1] After the oxygen is removed, blood reaches venules and then the veins which will take the blood back to the heart and lungs.[1] On the other hand when there is an AVM, blood goes directly from arteries to veins through the abnormal vessels which disrupts the normal circulation of blood.[1]
Causes
Arteriovenous malformations are most commonly prenatal in origin.[1] The cause of AVMs remains unknown.[1]
Epidemiology and Demographics
- Worldwide, the incidence of Cerebral arteriovenous malformation is approximately 1 per 100,000 patients.
- Worldwide, the prevalence of Cerebral arteriovenous malformation is 18,000 per 100,000 patients.
Gender
- AVMs are more common in males than females, although in females pregnancy may start or worsen symptoms due to the increase in blood flow and volume it usually brings.[2]
Natural History, Complications and Prognosis
- About 10% of cases in which excess bleeding occurs as the first symptom are deadly. Some patients may have permanent seizures, brain and nervous system (neurological) problems.
- The risk of hemorrhage from cerebral AVM is approximately 3% annually. This risk depends on the location, size, and presence of underlying diseases, such as hypertension or lipid disorders.
- AVMs that do not cause symptoms by the time people reach their late 40s or early 50s are more likely to remain stable and rarely cause symptoms.
- Prognosis depends on the injured region of the brain. Regions of the brain that control motor, sensory, visual, and language functions (termed eloquent areas of the cortex), deep white-matter pathways and basal ganglia structures have poor prognosis if involved in the hemorrhagic process. Also, increased intracranial pressure is associated with poor prognosis.
- Anatomical features of an AVM, may be used as a grading scale to predict treatment outcome.
- Spetzler–Martin grading scale is one of this scales. Lower grades (lower total points) indicate lower risk of treatment.
risks while taking into account the anatomical characteristics of a cerebral arteriovenous malformation. The grade is the sum of points assigned to the size of the lesion, the location (in or not in the eloquent cortex), and the presence or absence of deep venous drainage. | |||||||||||||||||||||||
Diagnosis
History and Symptoms
Clinical symptoms depends on the area of damaged area and the extent of adjacent brain tissue.
The most frequently observed problems related to an AVM are:
- Headache
- Seizure
- Symptoms of intracranial hemorrhage may be present which include:
- Loss of consciousness
- Nausea
- Vomiting
- Incontinence
- Blurred vision
- Hemiparesis
- Aphasia
- A loss of touch sensation on one side of the body
Physical Examination
HEENT
- Hydrocephalus may be present
Neurologic
- Meningeal signs may be present
- Hemiparesis may be present
- Aphasia may be present
- Hemianesthesia may be present
Laboratory findings
Lumbar puncture
Lumbar puncture can be used to examine spinal fluid for red blood cells; this condition is indicative of leakage of blood from the bleeding vessels into the subarachnoid space.
CT
A CT head scan can reveal the site of the bleed in the brain.
MRI
More detailed pictures of the tangle of blood vessels that compose an AVM can be obtained by taking an MRI of the head.
Images shown below are courtesy of RadsWiki
Cerebral angiography
This procedure involves using a catheter, threaded through an artery up to the head, to deliver a contrast agent into the AVM. As the contrast agent flows through the AVM structure, a sequence of X-ray images can be obtained to ascertain the size, shape and extent of that structure. This provides the best images of the AVM.
Treatment
The treatment in the case of sudden bleeding is focused on restoration of vital function. The risks associated with treatment of cerebral arteriovenous malformations must be balanced against the risks associated with no treatment.
Medical therapy
Chronic Pharmacotherapies
- Anticonvulsant medications such as phenytoin are often used to control seizures.
- Medications or procedures may be employed to relieve intracranial pressure.
- Eventually, curative treatment may be required to prevent recurrent hemorrhage.
Surgery
Stereotactic radiosurgery
Successful obliteration of the AVM is estimated on basis of size of the lesion and radiation delivered to the lesion. Small lesions (grade 1 or 2) responds well with the radiation dose of 18 Gy or more.
The most important limitation of the radiosurgery is the substantial delay in the radiographic obliteration of the lesion, which takes 2 to 4 years on average. Radiosurgery has been widely used on smaller AVMs with considerable success. The Gamma Knife, developed by Swedish physician Lars Leksell, is one apparatus used in radiosurgery to precisely apply a controlled radiation dosage to the volume of the brain occupied by the AVM. While this treatment is non-invasive, two to three years may pass before the complete effects are known. Complete occlusion of the AVM may or may not occur, and 8%-10% of patients develop long term neurological symptoms after radiation.[3]
Surgery and device based therapy
In the U.S., surgical removal of the blood vessels involved (craniotomy) is the preferred curative treatment for most types of AVM. While this surgery results in an immediate, complete removal of the AVM, risks exist depending on the size and the location of the malformation.[4] Microsurgical cauterization of feeding arteries and of draining veins allows for complete removal of the arteriovenous malformation as a single specimen but necessarily poses some risk to contiguous brain tissue, since the dissection plane is outside the boundary of the malformation. Outcomes for unruptured malformations are generally better than outcomes for lesions that have bled and caused neurologic deficits before surgery. The Spetzler–Martin grading scale has been used to determine the possible risk of procedure.
Endovascular embolization therapy
Occlusion of blood vessels with coils or particles, introduced by a radiographically guided catheter, is frequently used as an adjunct to either surgery or radiation treatment. Endovascular treatment of arteriovenous malformations is achieved by microcatheter delivery of agents such as N-butyl-2-cyanoacrylate or a nonadhesive ethylene vinyl alcohol copolymer. However, embolization alone is rarely successful in completely blocking blood flow through the AVM.[5]
Embolization before radiosurgery has also been proposed to reduce large arteriovenous malformations to a size that permits delivery of a more therapeutic marginal dose. The drawback of embolization before stereotactic radiosurgery is that embolic material in the malformation can shield the nidus from ionizing radiation and may obscure the outlines of the malformation, making targeting with radiotherapy difficult.[6]
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 Mayo Clinic staff (2009). "Brain AVM (arteriovenous malformation)-Causes". Mayo Foundation for Medical Education and Research. Retrieved 2010-05-30. Unknown parameter
|month=ignored (help) - ↑ Mayo Clinic staff (2009). "Brain AVM (arteriovenous malformation)-Risk factors". Mayo Foundation for Medical Education and Research. Retrieved 2010-05-30. Unknown parameter
|month=ignored (help) - ↑ Schaller C, Urbach H, Schramm J, Meyer B (2002). "Role of venous drainage in cerebral arteriovenous malformation surgery, as related to the development of postoperative hyperperfusion injury". Neurosurgery. 51 (4): 921–7, discussion 927–9. PMID 12234398.
- ↑ Morgan MK, Sundt TM (1989). "The case against staged operative resection of cerebral arteriovenous malformations". Neurosurgery. 25 (3): 429–35, discussion 435–6. PMID 2771013.
- ↑ Lee CC, Chen CJ, Ball B, Schlesinger D, Xu Z, Yen CP, Sheehan J (2015). "Stereotactic radiosurgery for arteriovenous malformations after Onyx embolization: a case-control study". J. Neurosurg. 123 (1): 126–35. doi:10.3171/2014.12.JNS141437. PMID 25658780.
- ↑ Ding D, Starke RM, Kano H, Lee JY, Mathieu D, Pierce J, Huang PP, Feliciano C, Rodriguez-Mercado R, Almodovar L, Grills IS, Silva D, Abbassy M, Missios S, Kondziolka D, Barnett GH, Lunsford LD, Sheehan JP (2017). "Stereotactic radiosurgery for Spetzler-Martin Grade III arteriovenous malformations: an international multicenter study". J. Neurosurg. 126 (3): 859–871. doi:10.3171/2016.1.JNS152564. PMID 27081906.

