Argatroban
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Alejandro Lemor, M.D. [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
Argatroban is a direct thrombin inhibitor that is FDA approved for the {{{indicationType}}} of thrombosis in heparin-induced thrombocytopenia and prophylaxis in PCI. Common adverse reactions include dyspnea, hypotension, fever, diarrhea, chest pain, back pain, nausea, vomiting, headache, sepsis, and cardiac arrest.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Heparin-Induced Thrombocytopenia
- Before administering argatroban, discontinue heparin therapy and obtain a baseline aPTT.
- Dosing Information
- Initial dose: 2 mcg/kg/min (continuous infusion)
- After the initiation of argatroban injection, adjust the dose (not to exceed 10 mcg/kg/min) as necessary to obtain a steady-state aPTT in the target range

Prophylaxis in Percutaneous Coronary Intervention
- Initial dose: 25 mcg/kg/min , administer a bolus of 350 mcg/kg via a large bore IV line over 3 to 5 minutes.
- Check an activated clotting time (ACT) 5 to 10 minutes after the bolus dose is completed.
- The PCI procedure may proceed if the ACT is greater than 300 seconds.
- If the ACT is less than 300 seconds, an additional intravenous bolus dose of 150 mcg/kg should be administered, the infusion dose increased to 30 mcg/kg/min, and the ACT checked 5 to 10 minutes later

- If the ACT is greater than 450 seconds, decrease the infusion rate to 15 mcg/kg/min, and check the ACT 5 to 10 minutes later.

* No bolus dose is given if ACT greater than 450 seconds
- Continue titrating the dose until a therapeutic ACT (between 300 and 450 seconds) has been achieved; continue the same infusion rate for the duration of the PCI procedure.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Argatroban in adult patients.
Non–Guideline-Supported Use
Cardiovascular surgical procedure
- Dosing Information
- Continuous infusion of 0.3 to 0.96 mcg/kg/min
- There are limited studies that suggest its usefulness.[1]
Cerebral thrombosis
- Dosing Information[2]
- Initial dose: 60 mg/day as a continuous IV infusion for 2 days
- Maintenance dose: 10 mg twice daily for 5 days
Disseminated intravascular coagulation
- Dosing Information
- 0.7 mcg/kg/min[3]
Extracorporeal circulation procedure
- Dosing Information
- 2 mcg/kg/min[4]
Prophylaxis in Hemodialysis for Venous Catheter Occlusion
- As an alternative to heparin.
Myocardial Infarction
- Dosing Information[5]
- Initial dose: 100 mcg/kg IV bolus
- Maintenance dose: 3 mcg/kg IV infusion
Unstable Angina
- Dosing Information
- 0.5 to 5 mcg/kg/min over 4 hours[6]
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
Heparin-Induced Thrombocytopenia
- Dosing Information
- Initial dose: 0.75 mcg/kg/min
- Check the aPTT two hours after the initiation of the argatroban infusion and adjust the dose to achieve the target aPTT.
- Increments of 0.1 to 0.25 mcg/kg/min for pediatric patients with normal hepatic function may be considered.
- Increments of 0.05 mcg/kg/min or lower for pediatric patients with impaired hepatic function may be considered.
- Initiate the infusion at a dose of 0.2 mcg/kg/min among seriously ill pediatric patients with impaired hepatic function
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Argatroban in pediatric patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Argatroban in pediatric patients.
Contraindications
- Patients with major bleeding.
- Patients with a history of hypersensitivity to argatroban. (Airway, skin, and generalized hypersensitivity reactions have been reported)
Warnings
Risk of Hemorrhage
- Hemorrhage can occur at any site in the body in patients receiving argatroban.
- Unexplained fall in hematocrit or blood pressure may indicate hemorrhage.
- Intracranial and retroperitoneal hemorrahage have been reported.
- The risk of hemorrahage with argatroban may be increased in severe hypertension; immediately following lumbar puncture, spinal anesthesia, major surgery (especially involving the brain, spinal cord, or eye), hematologic conditions associated with increased bleeding tendencies such as congenital or acquired bleeding disorders, and gastrointestinal lesions such as ulcerations.
- Concomitant use of argatroban with antiplatelet agents, thrombolytics, and other anticoagulants may increase the risk of bleeding.
Use in Hepatic Impairment
- When administering argatroban to patients with hepatic impairment, start with a lower dose and carefully titrate until the desired level of anticoagulation is achieved.
- Achievement of steady state aPTT levels may take longer and require more argatroban dose adjustments in patients with hepatic impairment compared to patients with normal hepatic function.
- Also, upon cessation of argatroban infusion in the hepatically impaired patient, full reversal of anticoagulant effects may require longer than 4 hours due to decreased clearance and increased elimination half-life of argatroban.
- Avoid the use of high doses of argatroban in patients undergoing PCI who have clinically significant hepatic disease or AST/ALT levels ≥3 times the upper limit of normal.
Laboratory Tests
- Anticoagulation effects associated with argatroban infusion at doses up to 40 mcg/kg/min correlate with increases of the activated partial thromboplastin time (aPTT).
- Although other global clot-based tests including prothrombin time (PT), the International Normalized Ratio (INR), and thrombin time (TT) are affected by argatroban, the therapeutic ranges for these tests have not been identified for argatroban therapy.
- In clinical trials in PCI, the activated clotting time (ACT) was used for monitoring argatroban anticoagulant activity during the procedure.
- The concomitant use of argatroban and warfarin results in prolongation of the PT and INR beyond that produced by warfarin alone.
Adverse Reactions
Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse event rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Adverse Events in Patients with HIT (With or Without Thrombosis)
The following safety information is based on all 568 patients treated with argatroban in Study 1 and Study 2. The safety profile of the patients from these studies is compared with that of 193 historical controls in which the adverse events were collected retrospectively. Adverse events are separated into hemorrhagic and non-hemorrhagic events.
Major bleeding was defined as bleeding that was overt and associated with a hemoglobin decrease ≥2 g/dL, that led to a transfusion of ≥2 units, or that was intracranial, retroperitoneal, or into a major prosthetic joint. Minor bleeding was overt bleeding that did not meet the criteria for major bleeding.
Table 4 gives an overview of the most frequently observed hemorrhagic events, presented separately by major and minor bleeding, sorted by decreasing occurrence among argatroban-treated patients with HIT (with or without thrombosis).

Table 5 gives an overview of the most frequently observed non-hemorrhagic events sorted by decreasing frequency of occurrence (=2%) among argatroban-treated HIT/HITTS patients.

Adverse Events in Patients with or at Risk for HIT Patients Undergoing PCI
The following safety information is based on 91 patients initially treated with argatroban and 21 patients subsequently re-exposed to argatroban for a total of 112 PCIs with argatroban anticoagulation. Adverse events are separated into hemorrhagic (Table 6) and non-hemorrhagic (Table 7) events.
Major bleeding was defined as bleeding that was overt and associated with a hemoglobin decrease ≥5 g/dL, that led to transfusion of ≥2 units, or that was intracranial, retroperitoneal, or into a major prosthetic joint.
The rate of major bleeding events in patients treated with argatroban in the PCI trials was 1.8%.

Table 7 gives an overview of the most frequently observed non-hemorrhagic events (>2%), sorted by decreasing frequency of occurrence among argatroban-treated PCI patients.

There were 22 serious adverse events in 17 PCI patients (19.6% in 112 interventions). Table 8 lists the serious adverse events occurring in argatroban-treated-patients with or at risk for HIT undergoing PCI.

Intracranial Bleeding In Other Populations
Increased risks for intracranial bleeding have been observed in investigational studies of argatroban for other uses. In a study of patients with acute myocardial infarction receiving both argatroban and thrombolytic therapy (streptokinase or tissue plasminogen activator), the overall frequency of intracranial bleeding was 1% (8 out of 810 patients). Intracranial bleeding was not observed in 317 subjects or patients who did not receive concomitant thrombolysis.
The safety and effectiveness of argatroban for cardiac indications other than PCI in patients with HIT have not been established. Intracranial bleeding was also observed in a prospective, placebo-controlled study of argatroban in patients who had onset of acute stroke within 12 hours of study entry. Symptomatic intracranial hemorrhage was reported in 5 of 117 patients (4.3%) who received argatroban at 1 to 3 mcg/kg/min and in none of the 54 patients who received placebo. Asymptomatic intracranial hemorrhage occurred in 5 (4.3%) and 2 (3.7%) of the patients, respectively.
Allergic Reactions
One hundred fifty-six allergic reactions or suspected allergic reactions were observed in 1,127 individuals who were treated with argatroban in clinical pharmacology studies or for various clinical indications. About 95% (148/156) of these reactions occurred in patients who concomitantly received thrombolytic therapy (e.g., streptokinase) or contrast media.
Allergic reactions or suspected allergic reactions in populations other than patients with HIT (with or without thrombosis) include (in descending order or frequency):
- Airway reactions (coughing, dyspnea): 10% or more
- Skin reactions (rash, bullous eruption): 1 to <10%
- General reactions (vasodilation): 1 to 10%
Limited data are available on the potential formation of drug-related antibodies. Plasma from 12 healthy volunteers treated with argatroban over 6 days showed no evidence of neutralizing antibodies. No loss of anticoagulant activity was noted with repeated administration of argatroban to more than 40 patients.
Postmarketing Experience
There is limited information regarding Argatroban Postmarketing Experience in the drug label.
Drug Interactions
Heparin
- If argatroban is to be initiated after cessation of heparin therapy, allow sufficient time for heparin’s effect on the aPTT to decrease prior to initiation of argatroban therapy.
Oral Anticoagulant Agents
- Pharmacokinetic drug-drug interactions between argatroban and warfarin (7.5 mg single oral dose) have not been demonstrated.
- However, the concomitant use of argatroban and warfarin (5 to 7.5 mg initial oral dose, followed by 2.5 to 6 mg/day orally for 6 to 10 days) results in prolongation of the prothrombin time (PT) and International Normalized Ratio (INR).
Aspirin/ Acetaminophen
- No drug-drug interactions have been demonstrated between argatroban and concomitantly administered aspirin or acetaminophen.
Thrombolytic Agents
- The safety and effectiveness of argatroban with thrombolytic agents have not been established.
Glycoprotein IIb/IIIa Antagonists
- The safety and effectiveness of argatroban with glycoprotein IIb/IIIa antagonists have not been established.
Use in Specific Populations
Pregnancy
Pregnancy Category (FDA): B
There are no adequate and well-controlled studies of argatroban use in pregnant women. Developmental studies performed in rats with argatroban at intravenous doses up to 27 mg/kg/day (0.3 times the maximum recommended human dose, based on body surface area) and in rabbits at intravenous doses up to 10.8 mg/kg/day (0.2 times the maximum recommended human dose, based on body surface area) have revealed no evidence of impaired fertility or harm to the fetus. Because animal reproduction studies are not always predictive of human response, this drug should be used during pregnancy only if clearly needed.
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Argatroban in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Argatroban during labor and delivery.
Nursing Mothers
It is not known whether argatroban is excreted in human milk. Argatroban is detected in rat milk. Because many drugs are excreted in human milk and because of the potential for serious adverse reactions in nursing infants from argatroban, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
Pediatric Use
The safety and effectiveness of argatroban, including the appropriate anticoagulation goals and duration of therapy, have not been established among pediatric patients. Argatroban was studied among 18 seriously ill pediatric patients who required an alternative to heparin anticoagulation. Most patients were diagnosed with HIT or suspected HIT. Age ranges of patients were <6 months, n = 8; six months to <8 years, n = 6; 8 to 16 years, n = 4. All patients had serious underlying conditions and were receiving multiple concomitant medications. Thirteen patients received argatroban solely as a continuous infusion (no bolus dose). Dosing was initiated in the majority of these 13 patients at 1 mcg/kg/min. Dosing was titrated as needed to achieve and maintain an aPTT of 1.5 to 3 times the baseline value. Most patients required multiple dose adjustments to maintain anticoagulation parameters within the desired range. During the 30-day study period, thrombotic events occurred during argatroban administration to two patients and following argatroban discontinuation in three other patients. Major bleeding occurred among two patients; one patient experienced an intracranial hemorrhage after 4 days of argatroban therapy in the setting of sepsis and thrombocytopenia. Another patient completed 14 days of argatroban treatment in the study, but experienced an intracranial hemorrhage while receiving argatroban following completion of the study treatment period.
Geriatic Use
Of the total number of subjects (1340) in clinical studies of argatroban, 35% were 65 and over. In the clinical studies of adult patients with HIT (with or without thrombosis), the effectiveness of argatroban was not affected by age. No trends were observed across age groups for both aPTT and the ACT. The safety analysis did suggest that older patients had increased underlying conditions, which may predispose them to events. The studies were not sized appropriately to detect differences in safety between age groups.
Gender
There are no clinically significant effects of gender on the pharmacokinetics or pharmacodynamics (e.g., aPTT) of argatroban in adults.
Race
There is no FDA guidance on the use of Argatroban with respect to specific racial populations.
Renal Impairment
No dosage adjustment is necessary in patients with renal dysfunction. The effect of renal disease on the pharmacokinetics of argatroban was studied in 6 subjects with normal renal function (mean Clcr = 95 ± 16 mL/min) and in 18 subjects with mild (mean Clcr = 64 ± 10 mL/min), moderate (mean Clcr = 41 ± 5.8 mL/min), and severe (mean Clcr = 5 ± 7 mL/min) renal impairment. The pharmacokinetics and pharmacodynamics of argatroban at dosages up to 5 mcg/kg/min were not significantly affected by renal dysfunction.
Use of argatroban was evaluated in a study of 12 patients with stable end-stage renal disease undergoing chronic intermittent hemodialysis. Argatroban was administered at a rate of 2 to 3 mcg/kg/min (begun at least 4 hours prior to dialysis) or as a bolus dose of 250 mcg/kg at the start of dialysis followed by a continuous infusion of 2 mcg/kg/min. Although these regimens did not achieve the goal of maintaining ACT values at 1.8 times the baseline value throughout most of the hemodialysis period, the hemodialysis sessions were successfully completed with both of these regimens. The mean ACTs produced in this study ranged from 1.39 to 1.82 times baseline, and the mean aPTTs ranged from 1.96 to 3.4 times the baseline. When argatroban was administered as a continuous infusion of 2 mcg/kg/min prior to and during a 4-hour hemodialysis session, approximately 20% was cleared through dialysis.
Hepatic Impairment
Dose reduction and careful titration are required when administering argatroban to patients with hepatic impairment. Reversal of anticoagulation effect may be prolonged in this population. Patients with hepatic impairment were not studied in percutaneous coronary intervention (PCI) trials. At a dose of 2.5 mcg/kg/min, hepatic impairment is associated with decreased clearance and increased elimination half-life of argatroban (to 1.9 mL/kg/min and 181 minutes, respectively, for patients with a Child-Pugh score greater than 6).
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Argatroban in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Argatroban in patients who are immunocompromised.
Administration and Monitoring
Administration
Argatroban should not be mixed with other drugs prior to dilution. Argatroban should be diluted in 0.9% sodium chloride injection, 5% dextrose injection, or lactated Ringer's injection to a final concentration of 1 mg/mL. The contents of each 2.5-mL vial should be diluted 100-fold by mixing with 250 mL of diluent. Use 250 mg (2.5 mL) per 250 mL of diluent or 500 mg (5 mL) per 500 mL of diluent.
The constituted solution must be mixed by repeated inversion of the diluent bag for 1 minute. Upon preparation, the solution may show slight but brief haziness due to the formation of microprecipitates that rapidly dissolve upon mixing. Use of diluent at room temperature is recommended. The final solution must be clear before use. The pH of the intravenous solution prepared as recommended is 3.2 to 7.5. Prepared solutions should not be exposed to direct sunlight. No significant potency losses have been noted following simulated delivery of the solution through intravenous tubing.
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration whenever solution and container permit.
Conversion to Oral Anticoagulant Therapy
Initiating Oral Anticoagulant Therapy
- When converting patients from argatroban to oral anticoagulant therapy, consider the potential for combined effects on INR with co-administration of argatroban and warfarin.
- A loading dose of warfarin should not be used. Initiate therapy using the expected daily dose of warfarin.
- To avoid prothrombotic effects and to ensure continuous anticoagulation when initiating warfarin, it is suggested that argatroban and warfarin therapy be overlapped.
- There are insufficient data available to recommend the duration of the overlap.
Co-Administration of Warfarin and Argatroban Injection at Doses Up to 2 mcg/kg/min
- Measure INR daily while argatroban Injection and warfarin are co-administered. In general, with doses of argatroban injection up to 2 mcg/kg/min, argatroban injection can be discontinued when the INR is >4 on combined therapy.
- After argatroban injection is discontinued, repeat the INR measurement in 4 to 6 hours.
- If the repeat INR is below the desired therapeutic range, resume the infusion of argatroban injection and repeat the procedure daily until the desired therapeutic range on warfarin alone is reached.
Co-Administration of Warfarin and Argatroban Injection at Doses Greater than 2 mcg/kg/min
- For doses greater than 2 mcg/kg/min, the relationship of INR between warfarin alone to the INR on warfarin plus argatroban is less predictable.
- In this case, in order to predict the INR on warfarin alone, temporarily reduce the dose of argatroban injection to a dose of 2 mcg/kg/min.
- Repeat the INR on argatroban injection and warfarin 4 to 6 hours after reduction of the argatroban Injection dose and follow the process outlined above for administering argatroban injection at doses up to 2 mcg/kg/min.
Monitoring
Heparin-Induced Thrombocytopenia
For use in HIT, therapy with argatroban injection is monitored using the aPTT with a target range of 1.5 to 3 times the initial baseline value (not to exceed 100 seconds). Tests of anticoagulant effects (including the aPTT) typically attain steady-state levels within 1 to 3 hours following initiation of argatroban injection.
Check the aPTT 2 hours after initiation of therapy and after any dose change to confirm that the patient has attained the desired therapeutic range.
Prophylaxis in Percutaneous Coronary Intervention
For use in PCI, therapy with argatroban injection is monitored using ACT. Obtain ACTs before dosing, 5 to 10 minutes after bolus dosing, following adjustments in the infusion rate, and at the end of the PCI procedure. Obtain additional ACTs every 20 to 30 minutes during prolonged procedure.
Pediatric Patients With Heparin-Induced Thrombocytopenia
In general, therapy with argatroban is monitored using the aPTT. Tests of anticoagulant effects (including the aPTT) typically attain steady-state levels within one to three hours following initiation of argatroban in patients without hepatic impairment. Dose adjustment may be required to attain the target aPTT. Check the aPTT two hours after initiation of therapy and after any dose change to confirm that the patient has attained the desired therapeutic range.
IV Compatibility
There is limited information regarding the compatibility of Argatroban and IV administrations.
Overdosage
- Excessive anticoagulation, with or without bleeding, may be controlled by discontinuing argatroban or by decreasing the argatroban dose.
- In clinical studies, anticoagulation parameters generally returned from therapeutic levels to baseline within 2 to 4 hours after discontinuation of the drug.
- Reversal of anticoagulant effect may take longer in patients with hepatic impairment.
- No specific antidote to argatroban is available; if life-threatening bleeding occurs and excessive plasma levels of argatroban are suspected, discontinue argatroban immediately and measure aPTT and other coagulation parameters.
- When argatroban was administered as a continuous infusion (2 mcg/kg/min) prior to and during a 4-hour hemodialysis session, approximately 20% of argatroban was cleared through dialysis.
- Single intravenous doses of argatroban at 200, 124, 150, and 200 mg/kg were lethal to mice, rats, rabbits, and dogs, respectively.
- The symptoms of acute toxicity were loss of lighting reflex, tremors, clonic convulsions, paralysis of hind limbs, and coma.
Pharmacology
| |
Argatroban
| |
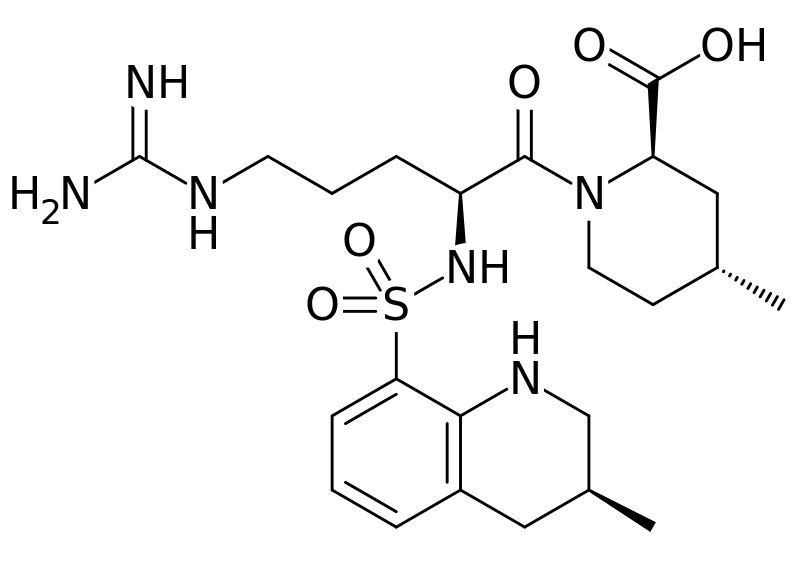
| Systematic (IUPAC) name | |
| (2R,4R)-1-[(2S)-5-(diaminomethylideneamino)-2- [[(3R)-3-methyl-1,2,3,4-tetrahydroquinolin-8-yl] sulfonylamino]pentanoyl]-4-methyl-piperidine-2- carboxylic acid | |
| Identifiers | |
| CAS number | |
| ATC code | B01 |
| PubChem | |
| DrugBank | |
| Chemical data | |
| Formula | Template:OrganicBox atomTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox |
| Mol. mass | 508.635 g/mol |
| SMILES | & |
| Pharmacokinetic data | |
| Bioavailability | 100% (intravenous) |
| Protein binding | 54% |
| Metabolism | hepatic |
| Half life | 39 and 51 minutes |
| Excretion | ? |
| Therapeutic considerations | |
| Pregnancy cat. |
? |
| Legal status | |
| Routes | intravenous |
Mechanism of Action
Argatroban is a direct thrombin inhibitor that reversibly binds to the thrombin active site. Argatroban does not require the co-factor antithrombin III for antithrombotic activity. Argatroban exerts its anticoagulant effects by inhibiting thrombin-catalyzed or -induced reactions, including fibrin formation; activation of coagulation factors V, VIII, and XIII; activation of protein C; and platelet aggregation.
Argatroban inhibits thrombin with an inhibition constant (Ki) of 0.04 μM. At therapeutic concentrations, argatroban has little or no effect on related serine proteases (trypsin, factor Xa, plasmin, and kallikrein).
Argatroban is capable of inhibiting the action of both free and clot-associated thrombin.
Structure
Argatroban is a synthetic direct thrombin inhibitor and the chemical name is 1-[5-[(aminoiminomethyl)amino]-1-oxo-2-(1,2,3,4-tetrahydro-3-methyl-8- quinolinyl)sulfonyl]amino]pentyl]-4-methyl-2-piperidinecarboxylic acid, monohydrate. Argatroban has 4 asymmetric carbons. One of the asymmetric carbons has an R configuration (stereoisomer Type I) and an S configuration (stereoisomer Type II). Argatroban consists of a mixture of R and S stereoisomers at a ratio of approximately 65:35. The molecular formula of Argatroban is C23H36N6O5S•H2O. Its molecular weight is 526.66 g/mol. The structural formula is shown below:
Argatroban is a white, odorless crystalline powder that is freely soluble in glacial acetic acid, slightly soluble in ethanol, and insoluble in acetone, ethyl acetate, and ether. Argatroban injection is a sterile clear, colorless to pale yellow, slightly viscous solution. Argatroban is available in 250-mg (in 2.5-mL) single-use amber vials, with white flip-top caps. Each mL of sterile, nonpyrogenic solution contains 100 mg Argatroban. Inert ingredients: 1300 mg Propylene glycol, 800 mg Dehydrated alcohol.
Pharmacodynamics
When argatroban is administered by continuous infusion, anticoagulant effects and plasma concentrations of argatroban follow similar, predictable temporal response profiles, with low intersubject variability. Immediately upon initiation of argatroban infusion, anticoagulant effects are produced as plasma argatroban concentrations begin to rise. Steady-state levels of both drug and anticoagulant effect are typically attained within 1 to 3 hours and are maintained until the infusion is discontinued or the dosage adjusted. Steady-state plasma argatroban concentrations increase proportionally with dose (for infusion doses up to 40 mcg/kg/min in healthy subjects) and are well correlated with steady-state anticoagulant effects. For infusion doses up to 40 mcg/kg/min, argatroban increases in a dose-dependent fashion, the activated partial thromboplastin time (aPTT), the activated clotting time (ACT), the prothrombin time (PT), the International Normalized Ratio (INR), and the thrombin time (TT) in healthy volunteers and cardiac patients. Representative steady-state plasma argatroban concentrations and anticoagulant effects are shown below for argatroban infusion doses up to 10 mcg/kg/min.

Effect on International Normalized Ratio (INR): Because argatroban is a direct thrombin inhibitor, co-administration of argatroban and warfarin produces a combined effect on the laboratory measurement of the INR. However, concurrent therapy, compared to warfarin monotherapy, exerts no additional effect on vitamin K–dependent factor Xa activity.
The relationship between INR on co-therapy and warfarin alone is dependent on both the dose of argatroban and the thromboplastin reagent used. This relationship is influenced by the International Sensitivity Index (ISI) of the thromboplastin. Data for 2 commonly utilized thromboplastins with ISI values of 0.88 (Innovin, Dade) and 1.78 (Thromboplastin C Plus, Dade) are presented in Figure 2 for an argatroban dose of 2 mcg/kg/min. Thromboplastins with higher ISI values than shown result in higher INRs on combined therapy of warfarin and argatroban. These data are based on results obtained in normal individuals.

The graph above demonstrates the relationship between INR for warfarin alone and INR for warfarin co-administered with argatroban at a dose of 2 mcg/kg/min. To calculate INR for warfarin alone (INRW), based on INR for co-therapy of warfarin and argatroban (INRWA), when the argatroban dose is 2 mcg/kg/min, use the equation next to the appropriate curve. Example: At a dose of 2 mcg/kg/min and an INR performed with Thromboplastin A, the equation 0.19 + 0.57 (INRWA) = INRW would allow a prediction of the INR on warfarin alone (INRW). Thus, using an INRWA value of 4.0 obtained on combined therapy: INRW = 0.19 + 0.57 (4) = 2.47 as the value for INR on warfarin alone. The error (confidence interval) associated with a prediction is ± 0.4 units. Similar linear relationships and prediction errors exist for argatroban at a dose of 1 mcg/kg/min. Thus, for argatroban doses of 1 or 2 mcg/kg/min, INRW can be predicted from INRWA. For argatroban doses greater than 2 mcg/kg/min, the error associated with predicting INRW from INRWA is ± 1. Thus, INRW cannot be reliably predicted from INRWA at doses greater than 2 mcg/kg/min.
Pharmacokinetics
Distribution
Argatroban distributes mainly in the extracellular fluid as evidenced by an apparent steady-state volume of distribution of 174 mL/kg (12.18 L in a 70-kg adult). Argatroban is 54% bound to human serum proteins, with binding to albumin and α1-acid glycoprotein being 20% and 34%, respectively.
Metabolism
The main route of argatroban metabolism is hydroxylation and aromatization of the 3-methyltetrahydroquinoline ring in the liver. The formation of each of the 4 known metabolites is catalyzed in vitro by the human liver microsomal cytochrome P450 enzymes CYP3A4/5. The primary metabolite (M1) exerts 3- to 5-fold weaker anticoagulant effects than argatroban. Unchanged argatroban is the major component in plasma. The plasma concentrations of M1 range between 0% and 20% of that of the parent drug. The other metabolites (M2 to M4) are found only in very low quantities in the urine and have not been detected in plasma or feces. These data, together with the lack of effect of erythromycin (a potent CYP3A4/5 inhibitor) on argatroban pharmacokinetics, suggest that CYP3A4/5-mediated metabolism is not an important elimination pathway in vivo.
Total body clearance is approximately 5.1 mL/kg/min (0.31 L/kg/hr) for infusion doses up to 40 mcg/kg/min. The terminal elimination half-life of argatroban ranges between 39 and 51 minutes.
There is no interconversion of the 21–(R):21–(S) diastereoisomers. The plasma ratio of these diastereoisomers is unchanged by metabolism or hepatic impairment, remaining constant at 65:35 (± 2%).
Excretion
Argatroban is excreted primarily in the feces, presumably through biliary secretion. In a study in which 14C-argatroban (5 mcg/kg/min) was infused for 4 hours into healthy subjects, approximately 65% of the radioactivity was recovered in the feces within 6 days of the start of infusion with little or no radioactivity subsequently detected. Approximately 22% of the radioactivity appeared in the urine within 12 hours of the start of infusion. Little or no additional urinary radioactivity was subsequently detected. Average percent recovery of unchanged drug, relative to total dose, was 16% in urine and at least 14% in feces.
Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenicity studies with argatroban have not been performed. Argatroban was not genotoxic in the Ames test, the Chinese hamster ovary cell (CHO/HGPRT) forward mutation test, the Chinese hamster lung fibroblast chromosome aberration test, the rat hepatocyte, and WI-38 human fetal lung cell unscheduled DNA synthesis (UDS) tests, or the mouse micronucleus test. Argatroban at intravenous doses up to 27 mg/kg/day (0.3 times the recommended maximum human dose based on body surface area) had no effect on fertility and reproductive function of male and female rats.
Clinical Studies
Heparin-Induced Thrombocytopenia
The safety and efficacy of argatroban were evaluated in a historically controlled efficacy and safety study (Study 1) and a follow-on efficacy and safety study (Study 2). These studies were comparable with regard to study design, study objectives, dosing regimens as well as study outline, conduct, and monitoring. In these studies, 568 adult patients were treated with argatroban and 193 adult patients made up the historical control group. Patients had a clinical diagnosis of heparin-induced thrombocytopenia, either without thrombosis (HIT) or with thrombosis (HITTS heparin-induced thrombocytopenia and thrombosis syndrome) and were males or non-pregnant females between the age of 18 and 80 years old. HIT/HITTS was defined by a fall in platelet count to less than 100,000/μL or a 50% decrease in platelets after the initiation of heparin therapy with no apparent explanation other than HIT. Patients with HITTS also had an arterial or venous thrombosis documented by appropriate imaging techniques or supported by clinical evidence such as acute myocardial infarction, stroke, pulmonary embolism, or other clinical indications of vascular occlusion. Patients who had documented histories of positive heparin-dependent antibody tests without current thrombocytopenia or heparin challenge (e.g., patients with latent disease) were also included if they required anticoagulation.
These studies did not include patients with documented unexplained aPTT >200% of control at baseline, documented coagulation disorder or bleeding diathesis unrelated to HIT, a lumbar puncture within the past 7 days or a history of previous aneurysm, hemorrhagic stroke, or a thrombotic stroke within the past 6 months unrelated to HIT.
The initial dose of argatroban was 2 mcg/kg/min. Two hours after the start of the argatroban infusion, an aPTT level was obtained and dose adjustments were made (up to a maximum of 10 mcg/kg/min) to achieve a steady-state aPTT value that was 1.5 to 3.0 times the baseline value, not to exceed 100 seconds. Overall the mean aPTT level for HIT and HITTS patients during the argatroban infusion increased from baseline values of 34 and 38 seconds, respectively, to 62.5 and 64.5 seconds, respectively.
The primary efficacy analysis was based on a comparison of event rates for a composite endpoint that included death (all causes), amputation (all causes) or new thrombosis during the treatment and follow-up period (study days 0 to 37). Secondary analyses included evaluation of the event rates for the components of the composite endpoint as well as time-to-event analyses.
In Study 1, a total of 304 patients were enrolled as follows: active HIT (n = 129), active HITTS (n =144), or latent disease (n = 31). Among the 193 historical controls, 139 (72%) had active HIT, 46 (24%) had active HITTS, and 8 (4%) had latent disease. Within each group, those with active HIT and those with latent disease were analyzed together. Positive laboratory confirmation of HIT/HITTS by the heparin-induced platelet aggregation test or serotonin release assay was demonstrated in 174 of 304 (57%) argatroban-treated patients (i.e., in 80 with HIT or latent disease and 94 with HITTS) and in 149 of 193 (77%) historical controls (i.e., in 119 with HIT or latent disease and 30 with HITTS). The test results for the remainder of the patients and controls were either negative or not determined.
There was a significant improvement in the composite outcome in patients with HIT and HITTS treated with argatroban versus those in the historical control group (see Table 9). The components of the composite endpoint are shown in Table 9.

b Reported as the most severe outcome among the components of composite endpoint (severity ranking: death > amputation > new thrombosis); patients may have had multiple outcomes.
Time-to-event analyses showed significant improvements in the time-to-first event in patients with HIT or HITTS treated with argatroban versus those in the historical control group. The between-group differences in the proportion of patients who remained free of death, amputation, or new thrombosis were statistically significant in favor of argatroban by these analyses.
A time-to-event analysis for the composite endpoint is shown in Figure 3 for patients with HIT and Figure 4 for patients with HITTS.

* Censored indicates no clinical endpoint (defined as death, amputation, or new thrombosis) was observed during the follow-up period (maximum period of follow-up was 37 days).

* Censored indicates no clinical endpoint (defined as death, amputation, or new thrombosis) was observed during the follow-up period (maximum period of follow-up was 37 days).
In Study 2, a total of 264 patients were enrolled as follows: HIT (n = 125) or HITTS (n = 139). There was a significant improvement in the composite efficacy outcome for argatroban-treated patients, versus the same historical control group from Study 1, among patients having HIT (25.6% vs. 38.8%), patients having HITTS (41.0% vs. 56.5%), and patients having either HIT or HITTS (33.7% vs. 43.0%). Time-to-event analyses showed significant improvements in the time-to-first event in patients with HIT or HITTS treated with argatroban versus those in the historical control group. The between-group differences in the proportion of patients who remained free of death, amputation, or new thrombosis were statistically significant in favor of argatroban.
Anticoagulant Effect
In Study 1, the mean (± SE) dose of argatroban administered was 2.0 ± 0.1 mcg/kg/min in the HIT arm and 1.9 ± 0.1 mcg/kg/min in the HITTS arm. Seventy-six percent of patients with HIT and 81% of patients with HITTS achieved a target aPTT at least 1.5-fold greater than the baseline aPTT at the first assessment occurring on average at 4.6 hours (HIT) and 3.9 hours (HITTS) following initiation of argatroban therapy.
No enhancement of aPTT response was observed in subjects receiving repeated administration of argatroban.
Platelet Count Recovery
In Study 1, 53% of patients with HIT and 58% of patients with HITTS, had a recovery of platelet count by Day 3. Platelet Count Recovery was defined as an increase in platelet count to >100,000/μL or to at least 1.5-fold greater than the baseline count (platelet count at study initiation) by Day 3 of the study.
Percutaneous Coronary Intervention (PCI) Patients with or at Risk for HIT
In 3 similarly designed trials, argatroban was administered to 91 patients with current or previous clinical diagnosis of HIT or heparin-dependent antibodies, who underwent a total of 112 percutaneous coronary interventions (PCIs) including percutaneous transluminal coronary angioplasty (PTCA), coronary stent placement, or atherectomy. Among the 91 patients undergoing their first PCI with argatroban, notable ongoing or recent medical history included myocardial infarction (n = 35), unstable angina (n = 23), and chronic angina (n = 34). There were 33 females and 58 males. The average age was 67.6 years (median 70.7, range 44 to 86), and the average weight was 82.5 kg (median 81.0 kg, range 49 to 141).
Twenty-one of the 91 patients had a repeat PCI using argatroban an average of 150 days after their initial PCI. Seven of 91 patients received glycoprotein IIb/IIIa inhibitors. Safety and efficacy were assessed against historical control populations who had been anticoagulated with heparin.
All patients received oral aspirin (325 mg) 2 to 24 hours prior to the interventional procedure. After venous or arterial sheaths were in place, anticoagulation was initiated with a bolus of argatroban of 350 mcg/kg via a large-bore intravenous line or through the venous sheath over 3 to 5 minutes. Simultaneously, a maintenance infusion of 25 mcg/kg/min was initiated to achieve a therapeutic activated clotting time (ACT) of 300 to 450 seconds. If necessary to achieve this therapeutic range, the maintenance infusion dose was titrated (15 to 40 mcg/kg/min) and/or an additional bolus dose of 150 mcg/kg could be given. Each patient’s ACT was checked 5 to 10 minutes following the bolus dose. The ACT was checked as clinically indicated. Arterial and venous sheaths were removed no sooner than 2 hours after discontinuation of argatroban and when the ACT was less than 160 seconds.
If a patient required anticoagulation after the procedure, argatroban could be continued, but at a lower infusion dose between 2.5 and 5 mcg/kg/min. An aPTT was drawn 2 hours after this dose reduction and the dose of argatroban then was adjusted as clinically indicated (not to exceed 10 mcg/kg/min), to reach an aPTT between 1.5 and 3 times baseline value (not to exceed 100 seconds).
In 92 of the 112 interventions (82%), the patient received the initial bolus of 350 mcg/kg and an initial infusion dose of 25 mcg/kg/min. The majority of patients did not require additional bolus dosing during the PCI procedure. The mean value for the initial ACT measurement after the start of dosing for all interventions was 379 sec (median 338 sec; 5th percentile-95th percentile 238 to 675 sec). The mean ACT value per intervention over all measurements taken during the procedure was 416 sec (median 390 sec; 5th percentile-95th percentile 261 to 698 sec). About 65% of patients had ACTs within the recommended range of 300 to 450 seconds throughout the procedure. The investigators did not achieve anticoagulation within the recommended range in about 23% of patients. However, in this small sample, patients with ACTs below 300 seconds did not have more coronary thrombotic events, and patients with ACTs over 450 seconds did not have higher bleeding rates.
Acute procedural success was defined as lack of death, emergent coronary artery bypass graft (CABG), or Q-wave myocardial infarction. Acute procedural success was reported in 98.2% of patients who underwent PCIs with argatroban anticoagulation compared with 94.3% of historical control patients anticoagulated with heparin (p = NS). Among the 112 interventions, 2 patients had emergency CABGs, 3 had repeat PTCAs, 4 had non-Q-wave myocardial infarctions, 3 had myocardial ischemia, 1 had an abrupt closure, and 1 had an impending closure (some patients may have experienced more than 1 event). No patients died.
How Supplied
Argatroban Injection is supplied as a single-use vial, containing 250 mg/2.5 mL (100 mg/mL). NDC 0143-9674-01 (Package of 1)
Storage
Store the vials in original carton at 20° - 25° C (68° - 77° F). Do not freeze. Retain in the original carton to protect from light. If the solution is cloudy, or if an insoluble precipitate is noted, the vial should be discarded.
Images
Drug Images
{{#ask: Page Name::Argatroban |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
{{#ask: Label Page::Argatroban |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
Inform patients of the risks associated with argatroban injection as well as the plan for regular monitoring during administration of the drug. Specifically, inform patients to report:
- The use of any other products known to affect bleeding.
- Any medical history that may increase the risk for bleeding, including a history of severe hypertension; recent lumbar puncture or spinal anesthesia; major surgery, especially involving the brain, spinal cord, or eye; hematologic conditions associated with increased bleeding tendencies such as congenital or acquired bleeding disorders and gastrointestinal lesions such as ulcerations.
- Any bleeding signs or symptoms.
- The occurrence of any signs or symptoms of allergic reactions (e.g., airway reactions, skin reactions and vasodilation reactions).
Precautions with Alcohol
Alcohol-Argatroban interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
Argatroban
Look-Alike Drug Names
- Argatroban - Aggrastat
- Argatroban - Orgaran
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
- ↑ K. Kumon, K. Tanaka, N. Nakajima, Y. Naito & T. Fujita (1984). "Anticoagulation with a synthetic thrombin inhibitor after cardiovascular surgery and for treatment of disseminated intravascular coagulation". Critical care medicine. 12 (12): 1039–1043. PMID 6439471. Unknown parameter
|month=ignored (help) - ↑ S. Kobayashi & Y. Tazaki (1997). "Effect of the thrombin inhibitor argatroban in acute cerebral thrombosis". Seminars in thrombosis and hemostasis. 23 (6): 531–534. doi:10.1055/s-2007-996131. PMID 9469625.
- ↑ K. Kumon, K. Tanaka, N. Nakajima, Y. Naito & T. Fujita (1984). "Anticoagulation with a synthetic thrombin inhibitor after cardiovascular surgery and for treatment of disseminated intravascular coagulation". Critical care medicine. 12 (12): 1039–1043. PMID 6439471. Unknown parameter
|month=ignored (help) - ↑ T. Kawada, H. Kitagawa, M. Hoson, Y. Okada & J. Shiomura (2000). "Clinical application of argatroban as an alternative anticoagulant for extracorporeal circulation". Hematology/oncology clinics of North America. 14 (2): 445–457. PMID 10806566. Unknown parameter
|month=ignored (help) - ↑ F. Vermeer, A. Vahanian, P. W. Fels, P. Besse, E. Muller, F. Van de Werf, D. Fitzgerald, H. Darius, J. Puel, D. Garrigou & M. L. Simoons (2000). "Argatroban and alteplase in patients with acute myocardial infarction: the ARGAMI Study". Journal of thrombosis and thrombolysis. 10 (3): 233–240. PMID 11122543. Unknown parameter
|month=ignored (help) - ↑ D. Fitzgerald & N. Murphy (1996). "Argatroban: a synthetic thrombin inhibitor of low relative molecular mass". Coronary artery disease. 7 (6): 455–458. PMID 8889361. Unknown parameter
|month=ignored (help)
{{#subobject:
|Label Page=Argatroban |Label Name=Argatroban label.jpg
}}
{{#subobject:
|Label Page=Argatroban |Label Name=Argatroban FDA panel.png
}}