Wolff-Parkinson-White syndrome resident survival guide: Difference between revisions
Rim Halaby (talk | contribs) |
Rim Halaby (talk | contribs) |
||
| Line 30: | Line 30: | ||
==Overview== | ==Overview== | ||
[[Wolff-Parkinson-White]] (WPW) syndrome is a condition of pre-excitation of the [[Ventricle (heart)|ventricles]] of the [[heart]] due to the presence of an [[accessory pathway]] known as the [[Bundle of Kent]] | [[Wolff-Parkinson-White]] (WPW) syndrome is a condition of pre-excitation of the [[Ventricle (heart)|ventricles]] of the [[heart]] due to the presence of an [[accessory pathway]] known as the [[Bundle of Kent]]. The difference between [[WPW]] pattern and [[WPW]] syndrome is that [[WPW]] pattern is characterized by the presence of a [[delta wave]] on the [[EKG]], whereas [[WPW]] syndrome is the occurrence of [[tachycardia]] with or without associated symptoms in a subject with existing [[WPW]] pattern<ref>{{Cite web | last = | first = | title = Wolff-Parkinson-White Syndrome and Accessory Pathways | url = http://circ.ahajournals.org/content/122/15/e480.full | publisher = | date = | accessdate = 1 April 2014 }}</ref>. The treatment of WPW syndrome is targeted towards the restoration of the [[sinus rhythm]], usually by the administration of either [[ibutilide]] or [[procainamide]]. The most common type of arrhythmia in [[WPW syndrome]] is [[AV reentrant tachycardia]]. [[Atrial fibrillation]] in a patient with [[WPW]] is life threatening and should be managed urgently. [[Atrial fibrillation]] in a patient with [[WPW]] should be suspected when there is [[ECG]] findings suggestive of [[atrial fibrillation]] in the context of a [[heart rate]] higher than 220 beats per minute. | ||
==Causes== | ==Causes== | ||
Revision as of 21:08, 1 April 2014
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Hilda Mahmoudi M.D., M.P.H.[2]; Alonso Alvarado, M.D.; Alejandro Lemor, M.D. [3]
Synonyms and keywords: WPW syndrome, WPW pattern
| Wolff-Parkinson-White Syndrome Resident Survival Guide Microchapters |
|---|
| Overview |
| Causes |
| Diagnosis |
| Treatment |
| Do's |
| Don'ts |
Overview
Wolff-Parkinson-White (WPW) syndrome is a condition of pre-excitation of the ventricles of the heart due to the presence of an accessory pathway known as the Bundle of Kent. The difference between WPW pattern and WPW syndrome is that WPW pattern is characterized by the presence of a delta wave on the EKG, whereas WPW syndrome is the occurrence of tachycardia with or without associated symptoms in a subject with existing WPW pattern[1]. The treatment of WPW syndrome is targeted towards the restoration of the sinus rhythm, usually by the administration of either ibutilide or procainamide. The most common type of arrhythmia in WPW syndrome is AV reentrant tachycardia. Atrial fibrillation in a patient with WPW is life threatening and should be managed urgently. Atrial fibrillation in a patient with WPW should be suspected when there is ECG findings suggestive of atrial fibrillation in the context of a heart rate higher than 220 beats per minute.
Causes
Life Threatening Causes
Wolff-Parkinson-White syndrome can be a life-threatening condition and must be treated as such irrespective of the underlying cause.
Common Causes
Diagnosis
First Initial Rapid Evaluation of Suspected Wolff-Parkinson-White Syndrome
Shown below is an algorithm depicting the First Initial Rapid Evaluation (FIRE) of suspected Wolff-Parkinson-White syndrome.
Identify cardinal signs and symptoms that increase the pretest probability of Wolff-Parkinson-White syndrome ❑ Regular rhythm ❑ Rate over 150 bpm ❑ Crackles in pulmonary auscultation ❑ Hypotension | |||||||||||||||||||||||||||||||||||||||||||||||
Identify alarming signs and symptoms ❑ Tachycardia | |||||||||||||||||||||||||||||||||||||||||||||||
Unstable patient | Stable patient | ||||||||||||||||||||||||||||||||||||||||||||||
❑ Perform DC electrical cardioversion | |||||||||||||||||||||||||||||||||||||||||||||||
Complete Diagnostic Approach of Wolff-Parkinson-White Syndrome
Shown below is an algorithm summarizing the diagnostic approach to Wolff-Parkinson-White syndrome according to the 2003 ACC/AHA/ESC guidelines for the management of patients with supraventricular arrhythmias.[2]
Abbreviations: AVRT: AV reentrant tachycardia; BP: blood pressure; AF: atrial fibrillation HF: heart failure LVH: left ventricular hypertrophy; ECG: electrocardiography
Characterize the symptoms: ❑ Asymptomatic
❑ Duration
| |||||||||||||||||||||||
Identify possible triggers: ❑ Infection | |||||||||||||||||||||||
Examine the patient: Appearance of the patient Vitals
Cardiovascular | |||||||||||||||||||||||
Order studies: ❑ ECG | |||||||||||||||||||||||
Orthodromic AVRT The impulse travels from the atrium to the ventricle through the AV node and returns to the atrium through the accessory pathway. 90-95% of WPW 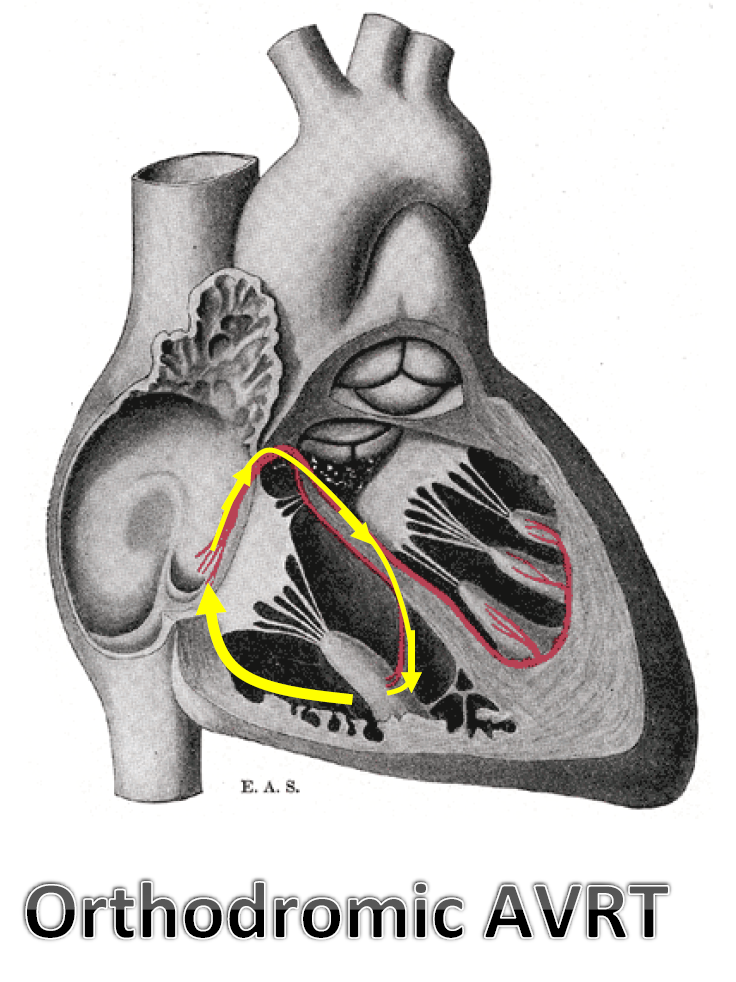 EKG findings: 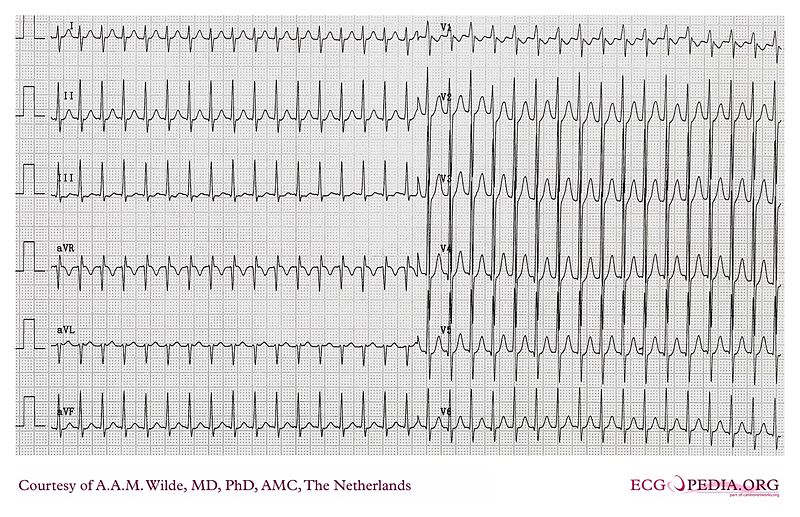 | Antidromic AVRT The impulse travels from the atrium to the ventricle through the accessory pathway and from the ventricle to the atrium through the AV node. Less than 10% of WPW 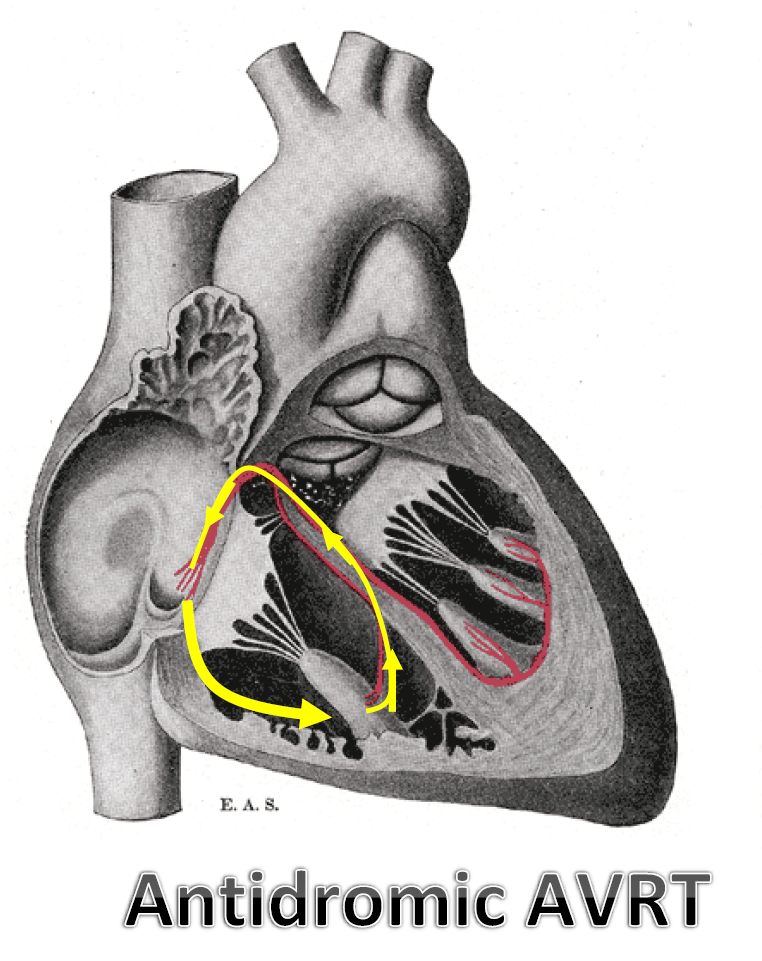 EKG findings: 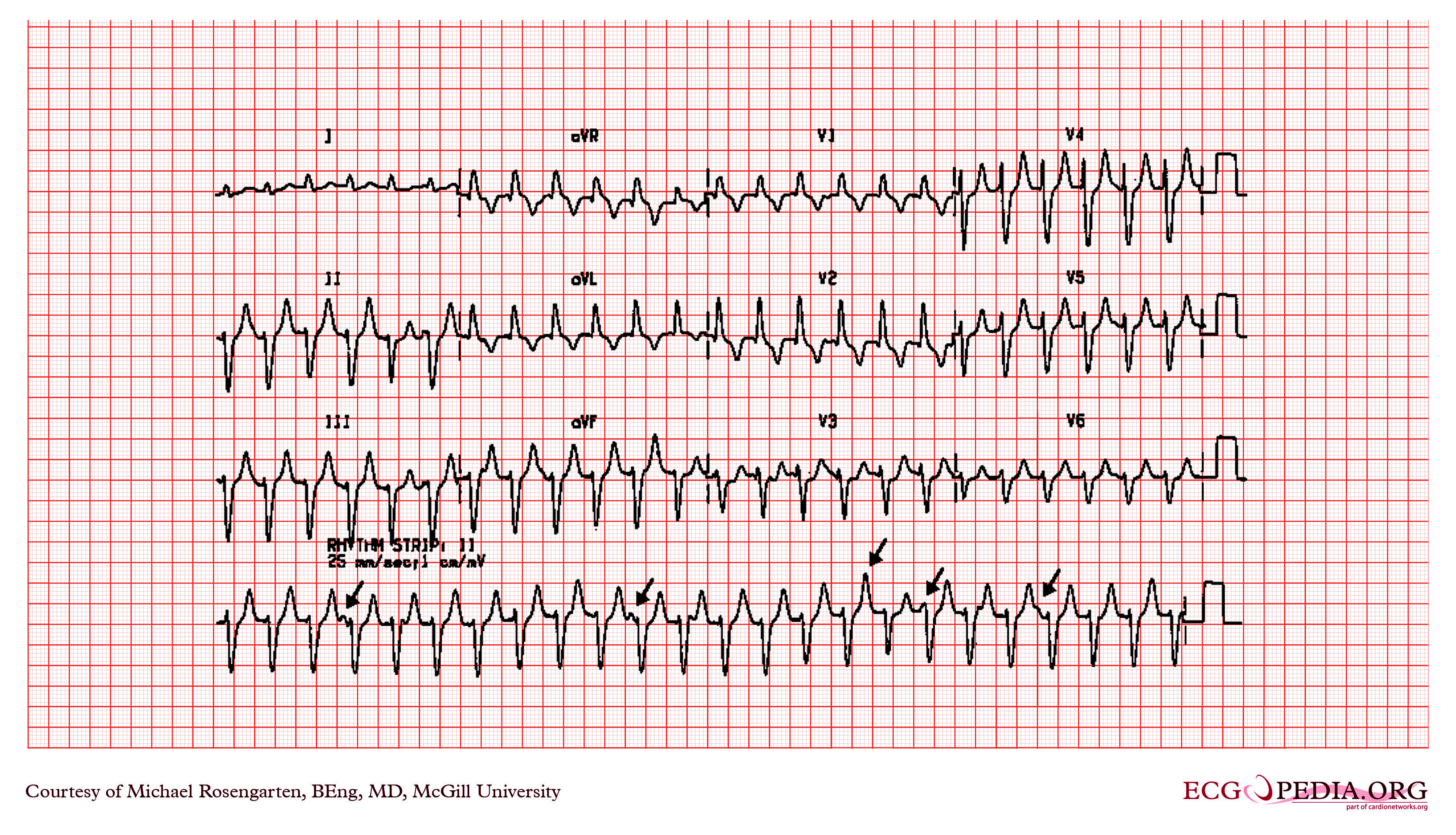 | ||||||||||||||||||||||
Treatment
Initial Treatment
Shown below is an algorithm summarizing the initial approach to Wolff-Parkinson-White syndrome according to the 2003 ACC/AHA/ESC guidelines for the management of patients with supraventricular arrhythmias.[2]
Determine if the patient has any unstable signs or symptoms ❑ Chest pain | |||||||||||||||||||||||||||||
| Stable patient | Unstable patient | ||||||||||||||||||||||||||||
❑ Assess the ECG | ❑ Urgent electrical cardioversion (Class I, Level of Evidence C) | ||||||||||||||||||||||||||||
| Orthodromic AVRT | Antidromic AVRT | ||||||||||||||||||||||||||||
❑ Use vagal maneuvers (Class I, Level of Evidence B)
| Avoid the use of av blocking agents such as digoxin, verapamil or diltiazem ❑ Administer ibutilide 1 mg IV infusion over 10 minutes (Class I, Level of Evidence B)
| ||||||||||||||||||||||||||||
Wolff-Parkinson-White Syndrome with Atrial Fibrillation
Atrial fibrillation in a patient with WPW should be suspected when the the heart rate of a patient with WPW is between 220 and 360 bpm. Shown below is an algorithm summarizing the managment of Wolff-Parkinson-White syndrome with atrial fibrillation according to the ACC/AHA/ESC 2006 Guidelines for the Management of Patients with Atrial Fibrillation.[3]
Determine if the patient has any unstable signs or symptoms ❑ Chest pain | |||||||||||||||||||||||||||
| Stable patient | Unstable patient | ||||||||||||||||||||||||||
Avoid the use of AV node blocking agents such as digoxin, verapamil or diltizem
| ❑ Urgent electric cardioversion (Class I, Level of Evidence B) | ||||||||||||||||||||||||||
Long-Term Treatment
Shown below is an algorithm summarizing the long-term treatment of Wolff-Parkinson-White syndrome.
| Long Term management | |||||||||||||||||||||||||||||||||
Single or infrequent episodes ❑ No treatment (Class I, Level of Evidence C) | Recurrent episodes ❑ Catheter ablation (Class I, Level of Evidence B) | Asymptomatic ❑ No treatment (Class I, Level of Evidence C) | |||||||||||||||||||||||||||||||
Do's
- Perform catheter ablation of the accessory pathway if possible (class I, level of evidence B).
- Electrical cardioversion can be performed in cases of WPW with AF with rapid ventricular response (class II, level of evidence A).
- In asymptomatic patients, either no intervention (class I, level of evidence C) or catheter ablation (class IIb, level of evidence B) could be performed.
- Prescribe propafenone over flecainide for the prevention of recurrence orthodromic AVRT as it has also a mild beta blocking activity.
- Schedule exercise stress test and electrophysiology tests for the sudden cardiac death stratification (class IIa, level of evidence B).
- Consider catheter ablation in asymptomatic patients with structural heart disease (class IIb, level of evidence C).
Don'ts
- Don't use AV blocking agents in patients with WPW and antidromic AVRT as it will promote promote conduction down the accessory pathway (class III, level of evidence C).[4]
- Avoid the usage of AV blocking agents in patients with WPW and AF (class III, level of evidence B).
- Avoid AV blocking agents (such as digoxin, verapamil or diltiazem) as chronic treatment to prevent the recurrence of tachycardia (class III, level of evidence B).
References
- ↑ "Wolff-Parkinson-White Syndrome and Accessory Pathways". Retrieved 1 April 2014.
- ↑ 2.0 2.1 "ACC/AHA/ESC Guidelines for the Management of Patients With Supraventricular Arrhythmias—Executive Summary". Retrieved 15 August 2013.
- ↑ Fuster, V.; Rydén, LE.; Cannom, DS.; Crijns, HJ.; Curtis, AB.; Ellenbogen, KA.; Halperin, JL.; Le Heuzey, JY.; Kay, GN. (2006). "ACC/AHA/ESC 2006 Guidelines for the Management of Patients with Atrial Fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Revise the 2001 Guidelines for the Management of Patients With Atrial Fibrillation): developed in collaboration with the European Heart Rhythm Association and the Heart Rhythm Society". Circulation. 114 (7): e257–354. doi:10.1161/CIRCULATIONAHA.106.177292. PMID 16908781. Unknown parameter
|month=ignored (help) - ↑ Garratt, C.; Antoniou, A.; Ward, D.; Camm, AJ. (1989). "Misuse of verapamil in pre-excited atrial fibrillation". Lancet. 1 (8634): 367–9. PMID 2563516. Unknown parameter
|month=ignored (help) - ↑ Gulamhusein, S.; Ko, P.; Carruthers, SG.; Klein, GJ. (1982). "Acceleration of the ventricular response during atrial fibrillation in the Wolff-Parkinson-White syndrome after verapamil". Circulation. 65 (2): 348–54. PMID 7053894. Unknown parameter
|month=ignored (help) - ↑ McGovern, B.; Garan, H.; Ruskin, JN. (1986). "Precipitation of cardiac arrest by verapamil in patients with Wolff-Parkinson-White syndrome". Ann Intern Med. 104 (6): 791–4. PMID 3706931. Unknown parameter
|month=ignored (help)