Wolff-Parkinson-White syndrome pathophysiology: Difference between revisions
Rim Halaby (talk | contribs) |
|||
| Line 7: | Line 7: | ||
==Pathophysiology== | ==Pathophysiology== | ||
* | |||
* | * Electrical activity in the normal human heart is initiated when a cardiac action potential arises in the sinoatrial (SA) node, which is located in the right atrium. From there, the electrical stimulus is transmitted via internodal pathways to the atrioventricular (AV) node. After a brief delay at the AV node, the stimulus is conducted through the bundle of His to the left and right bundle branches and then to the Purkinje fibers and the endocardium at the apex of the heart, then finally to the ventricular myocardium. | ||
* | * The AV node serves an important function as a "gatekeeper", limiting the electrical activity that reaches the ventricles. In situations where the atria generate excessively rapid electrical activity (such as atrial fibrillation or atrial flutter), the AV node limits the number of signals conducted to the ventricles. For example, if the atria are electrically activated at 300 beats per minute, half those electrical impulses may be blocked by the AV node, so that the ventricles are stimulated at only 150 beats per minute—resulting in a pulse of 150 beats per minute. Another important property of the AV node is that it slows down individual electrical impulses. This is manifested on the electrocardiogram as the PR interval (the time from electrical activation of the atria to electrical activation of the ventricles), which is usually shortened to less than 120 milliseconds in duration. | ||
* Individuals with WPW have an accessory pathway that communicates between the atria and the ventricles, in addition to the AV node. This accessory pathway is known as the bundle of Kent (see below). This accessory pathway does not share the rate-slowing properties of the AV node, and may conduct electrical activity at a significantly higher rate than the AV node. For instance, in the example above, if an individual had an atrial rate of 300 beats per minute, the accessory bundle may conduct all the electrical impulses from the atria to the ventricles, causing the ventricles to contract at 300 beats per minute. Extremely rapid heart rates such as this may result in hemodynamic instability or cardiogenic shock. In some cases, the combination of an accessory pathway and cardiac dysrhythmias can trigger ventricular fibrillation, a leading cause of sudden cardiac death. | |||
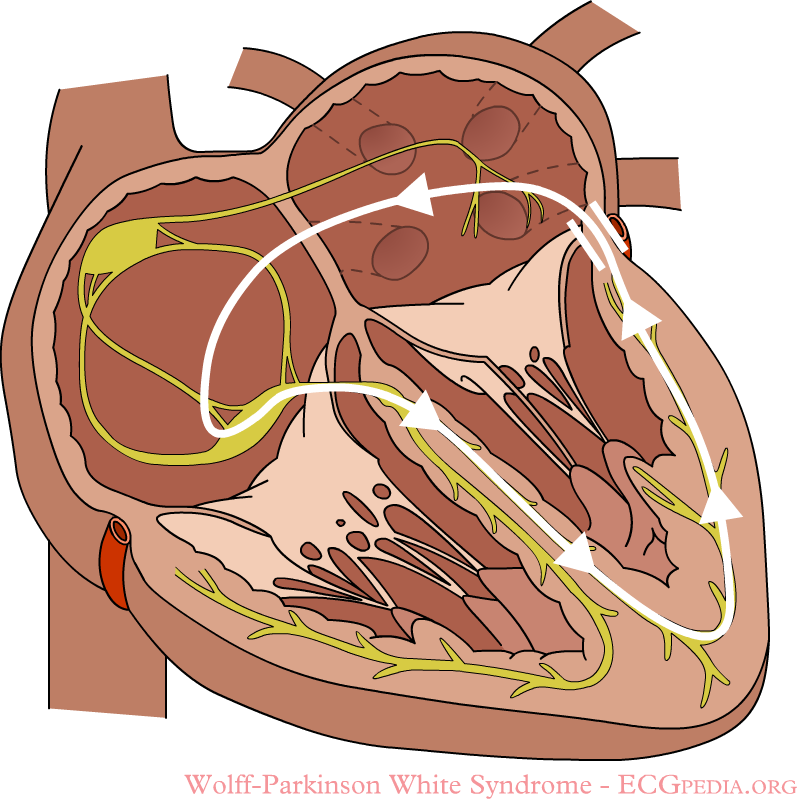
[[Image:WPW.png|thumb|center|300px|A atrioventricular tachycardia through the accessory bundle. The electrical signal travels from the ventricles via the accessory bundle to the atria and returns to the ventricles via the AV node]] | [[Image:WPW.png|thumb|center|300px|A atrioventricular tachycardia through the accessory bundle. The electrical signal travels from the ventricles via the accessory bundle to the atria and returns to the ventricles via the AV node]] | ||
Revision as of 23:43, 14 April 2014
|
Wolff-Parkinson-White syndrome Microchapters |
|
Differentiating Wolff-Parkinson-White syndrome from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Wolff-Parkinson-White syndrome pathophysiology On the Web |
|
Risk calculators and risk factors for Wolff-Parkinson-White syndrome pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Overview
In normal individuals, electrical activity in the heart is initiated in the sinoatrial (SA) node (located in the right atrium), propagates to the atrioventricular (AV) node, and then through the bundle of His to the ventricles of the heart. (See electrical conduction system of the heart).
Pathophysiology
- Electrical activity in the normal human heart is initiated when a cardiac action potential arises in the sinoatrial (SA) node, which is located in the right atrium. From there, the electrical stimulus is transmitted via internodal pathways to the atrioventricular (AV) node. After a brief delay at the AV node, the stimulus is conducted through the bundle of His to the left and right bundle branches and then to the Purkinje fibers and the endocardium at the apex of the heart, then finally to the ventricular myocardium.
- The AV node serves an important function as a "gatekeeper", limiting the electrical activity that reaches the ventricles. In situations where the atria generate excessively rapid electrical activity (such as atrial fibrillation or atrial flutter), the AV node limits the number of signals conducted to the ventricles. For example, if the atria are electrically activated at 300 beats per minute, half those electrical impulses may be blocked by the AV node, so that the ventricles are stimulated at only 150 beats per minute—resulting in a pulse of 150 beats per minute. Another important property of the AV node is that it slows down individual electrical impulses. This is manifested on the electrocardiogram as the PR interval (the time from electrical activation of the atria to electrical activation of the ventricles), which is usually shortened to less than 120 milliseconds in duration.
- Individuals with WPW have an accessory pathway that communicates between the atria and the ventricles, in addition to the AV node. This accessory pathway is known as the bundle of Kent (see below). This accessory pathway does not share the rate-slowing properties of the AV node, and may conduct electrical activity at a significantly higher rate than the AV node. For instance, in the example above, if an individual had an atrial rate of 300 beats per minute, the accessory bundle may conduct all the electrical impulses from the atria to the ventricles, causing the ventricles to contract at 300 beats per minute. Extremely rapid heart rates such as this may result in hemodynamic instability or cardiogenic shock. In some cases, the combination of an accessory pathway and cardiac dysrhythmias can trigger ventricular fibrillation, a leading cause of sudden cardiac death.
Genetics
WPW syndrome has been identified in to have a genetic backgournd as 0.55% of degree relatives of patients with WPW presents the disease. Missgene mutations (single nucelotide changes) in the gene PAKAG2 have been found in families with WPW. PAKAG2 encodes for the protein AMP-activated protein kinase (AMPK) gamma-2 subunit. AMPK, among other physiological functions, decreases glycogen synthesis, glycogen is abundant in the hearts conduction system, therefore an excesive acumulation of glycogen will prevent the accessory pathway to close. It has been reported that patients with familial WPW usualy have increased amounts of glycogen in the myocardial tissue. Patients with this disease, along with the preexcitations, they present myocardial hypertrophy and AV block. Nevertheless, WPW syndrome is usualy sporadic in origin and a small percentage from all csases have familial origin which presents as an autosomal dominant form.[1]
Associated Conditions
Associated disorders when present are most commonly associated with right-sided accessory pathway than left-sided pathways. WPW syndrome is associated with the following disorders:
- Ebstein's anomaly[2][3][4]
- Mitral valve prolapse: This cardiac disorder, if present, is associated with left-sided accessory pathways[5].
- Hypertrophic cardiomyopathy: This disorder is associated with familial/inherited form of WPW syndrome[6].
References
- ↑ Sidhu, J.; Roberts, R. (2003). "Genetic basis and pathogenesis of familial WPW syndrome". Indian Pacing Electrophysiol J. 3 (4): 197–201. PMID 16943919.
- ↑ Rao MP, Panduranga P, Al-Mukhaini M, Al-Jufaili M (2012). "Ebstein anomaly in an adult presenting with wide QRS tachycardia: diagnostic and therapeutic dilemmas". Am J Emerg Med. 30 (5): 834.e1–4. doi:10.1016/j.ajem.2011.03.001. PMID 21570234. Unknown parameter
|month=ignored (help) - ↑ Bayar N, Canbay A, Uçar O, Aydoğdu S, Diker E (2010). "[Association of Gerbode-type defect and Wolff-Parkinson-White syndrome with Ebstein's anomaly]". Anadolu Kardiyol Derg (in Turkish). 10 (1): 88–90. PMID 20150013. Unknown parameter
|month=ignored (help) - ↑ Legius B, Van De Bruaene A, Van Deyk K; et al. (2010). "Behavior of Ebstein's anomaly: single-center experience and midterm follow-up". Cardiology. 117 (2): 90–5. doi:10.1159/000318041. PMID 20924185.
- ↑ Savini E, Capone PL (1994). "[Wolff-Parkinson-White, a study on the prevalence of the site of accessory pathways: relations between stability of pre-excitation, symptoms, cardiac arrhythmias and association of mitral valve prolapse with localization of pre-excitation]". Minerva Cardioangiol (in Italian). 42 (7–8): 339–43. PMID 7970027.
- ↑ Kruchina TK, Vasichkina ES, Egorov DF, Tatarskiĭ BA (2012). "[Asymptomatic ventricular pre-excitation in children: a 17 year follow-up study]". Kardiologiia (in Russian). 52 (5): 30–6. PMID 22839583.