Wernicke's encephalopathy: Difference between revisions
mNo edit summary |
Ahmed Younes (talk | contribs) |
||
| Line 32: | Line 32: | ||
==Differentiating {{PAGENAME}} from Other Diseases== | ==Differentiating {{PAGENAME}} from Other Diseases== | ||
Wernicke's encephalopathy must be differentiated from other causes of headache, altered mental status and seizures such as brain tumors and delirium trmemns. | |||
{| | |||
|- style="background: #4479BA; color: #FFFFFF; text-align: center;" | |||
! rowspan="2" |<small>Diseases</small> | |||
! colspan="4" |<small>Diagnostic tests</small> | |||
! colspan="5" |<small>Physical Examination</small> | |||
! colspan="3" |<small>Symptoms | |||
! colspan="1" rowspan="2" |<small>Past medical history</small> | |||
! rowspan="2" |<small>Other Findings</small> | |||
|- style="background: #4479BA; color: #FFFFFF; text-align: center;" | |||
!<small>Na+, K+, Ca2+</small> | |||
!<small>CT /MRI</small> | |||
!<small>CSF Findings</small> | |||
!<small>Gold standard test</small> | |||
!<small>Neck stiffness</small> | |||
!<small>Motor or Sensory deficit</small> | |||
!<small>Papilledema</small> | |||
!<small>Bulging fontanelle</small> | |||
!<small>Cranial nerves</small> | |||
!<small>Headache</small> | |||
!<small>Fever</small> | |||
!<small>Altered mental status</small> | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" | [[Brain tumor|Brain tumour]]<ref name="pmid1278192">Soffer D (1976) [http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=1278192 Brain tumors simulating purulent meningitis.] ''Eur Neurol'' 14 (3):192-7. PMID: [http://pubmed.gov/1278192 1278192]</ref><ref name="pmid3883130" /> | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |? | |||
| style="background: #F5F5F5; padding: 5px text-align:center" |Cancer cells<ref name="pmid21371327">{{cite journal| author=Weston CL, Glantz MJ, Connor JR| title=Detection of cancer cells in the cerebrospinal fluid: current methods and future directions. | journal=Fluids Barriers CNS | year= 2011 | volume= 8 | issue= 1 | pages= 14 | pmid=21371327 | doi=10.1186/2045-8118-8-14 | pmc=3059292 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21371327 }}</ref> | |||
| style="background: #F5F5F5; padding: 5px;" |MRI | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" | | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |? | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |? | |||
| style="background: #F5F5F5; padding: 5px;text-align:center" |? | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" | ? | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |? | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" |? | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" |[[Cachexia]], gradual progression of symptoms | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Delirium tremens|Delerium Tremens]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |? | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" |Clinical diagnosis | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" | | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |? | |||
| style="background: #F5F5F5; padding: 5px;text-align:center" |? | |||
| style="background: #F5F5F5; padding: 5px;text-align:center" | | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" | ? | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" | ? | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |? | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |? | |||
| style="background: #F5F5F5; padding: 5px;" |Alcohal intake, sudden witdrawl or reduction in consumption | |||
| style="background: #F5F5F5; padding: 5px;" |Tachycardia, diaphoresis, hypertension, tremors, mydriasis, positional nystagmus, tachypnea | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" | [[Subarachnoid hemorrhage]]<ref name="pmid14585453">Yeh ST, Lee WJ, Lin HJ, Chen CY, Te AL, Lin HJ (2003) [http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=14585453 Nonaneurysmal subarachnoid hemorrhage secondary to tuberculous meningitis: report of two cases.] ''J Emerg Med'' 25 (3):265-70. PMID: [http://pubmed.gov/14585453 14585453]</ref> | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |? | |||
| style="background: #F5F5F5; padding: 5px;" |Xanthochromia<ref name="pmid1198628">{{cite journal| author=Lee MC, Heaney LM, Jacobson RL, Klassen AC| title=Cerebrospinal fluid in cerebral hemorrhage and infarction. | journal=Stroke | year= 1975 | volume= 6 | issue= 6 | pages= 638-41 | pmid=1198628 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=1198628 }}</ref> | |||
| style="background: #F5F5F5; padding: 5px;" |CT scan without contrast<ref name="pmid21694755">{{cite journal| author=Birenbaum D, Bancroft LW, Felsberg GJ| title=Imaging in acute stroke. | journal=West J Emerg Med | year= 2011 | volume= 12 | issue= 1 | pages= 67-76 | pmid=21694755 | doi= | pmc=3088377 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21694755 }}</ref><ref name="pmid21807345">{{cite journal| author=DeLaPaz RL, Wippold FJ, Cornelius RS, Amin-Hanjani S, Angtuaco EJ, Broderick DF et al.| title=ACR Appropriateness Criteria® on cerebrovascular disease. | journal=J Am Coll Radiol | year= 2011 | volume= 8 | issue= 8 | pages= 532-8 | pmid=21807345 | doi=10.1016/j.jacr.2011.05.010 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21807345 }}</ref> | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |? | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |? | |||
| style="background: #F5F5F5; padding: 5px;text-align:center" |? | |||
| style="background: #F5F5F5; padding: 5px;text-align:center" |? | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" | ? | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |? | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |? | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |? | |||
| style="background: #F5F5F5; padding: 5px;" |Trauma/fall | |||
| style="background: #F5F5F5; padding: 5px;" |Confusion, dizziness, nausea, vomiting | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" | [[Stroke]] | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" | | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |? | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" | Normal | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" | CT scan without contrast | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" | | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |? | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |? | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" | | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |? | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |? | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" | | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |? | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |TIAs, hypertension, diabetes mellitus | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |Speech difficulty, gait abnormality | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Neurosyphilis]]<ref name="pmid22482824">{{cite journal| author=Liu LL, Zheng WH, Tong ML, Liu GL, Zhang HL, Fu ZG et al.| title=Ischemic stroke as a primary symptom of neurosyphilis among HIV-negative emergency patients. | journal=J Neurol Sci | year= 2012 | volume= 317 | issue= 1-2 | pages= 35-9 | pmid=22482824 | doi=10.1016/j.jns.2012.03.003 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22482824 }} </ref><ref name="pmid24365430">{{cite journal |vauthors=Berger JR, Dean D |title=Neurosyphilis |journal=Handb Clin Neurol |volume=121 |issue= |pages=1461–72 |year=2014 |pmid=24365430 |doi=10.1016/B978-0-7020-4088-7.00098-5 |url=}}</ref> | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |? | |||
| style="background: #F5F5F5; padding: 5px;" |'''?''' [[Leukocytes]] and [[protein]] | |||
| style="background: #F5F5F5; padding: 5px;" |CSF [[VDRL]]-specifc | |||
CSF FTA-Ab -sensitive<ref name="pmid22421697">{{cite journal| author=Ho EL, Marra CM| title=Treponemal tests for neurosyphilis--less accurate than what we thought? | journal=Sex Transm Dis | year= 2012 | volume= 39 | issue= 4 | pages= 298-9 | pmid=22421697 | doi=10.1097/OLQ.0b013e31824ee574 | pmc=3746559 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22421697 }}</ref> | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |? | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |? | |||
| style="background: #F5F5F5; padding: 5px;text-align:center" |? | |||
| style="background: #F5F5F5; padding: 5px;text-align:center" |? | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |? | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |? | |||
| style="background: #F5F5F5; padding: 5px;" |Unprotected sexual intercourse, STIs | |||
| style="background: #F5F5F5; padding: 5px;" |Blindness, confusion, [[depression]], | |||
Abnormal [[gait]] | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Viral encephalitis]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" |? | |||
| style="background: #F5F5F5; padding: 5px;" |Increased RBCS or xanthochromia, mononuclear lymphocytosis, high protein content, normal glucose | |||
| style="background: #F5F5F5; padding: 5px;" |Clinical assesment | |||
| style="background: #F5F5F5; padding: 5px;" |? | |||
| style="background: #F5F5F5; padding: 5px;" |? | |||
| style="background: #F5F5F5; padding: 5px;text-align:center" |? | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" | ? | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |? | |||
| style="background: #F5F5F5; padding: 5px;" |? | |||
| style="background: #F5F5F5; padding: 5px;" |? | |||
| style="background: #F5F5F5; padding: 5px;" |Tick bite/mosquito bite/ viral prodome for several days | |||
| style="background: #F5F5F5; padding: 5px;" |Extreme lethargy, rash hepatosplenomegaly, lymphadenopathy, behavioural changes | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Herpes simplex encephalitis]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" |? | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" |Clinical assesment | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" |? | |||
| style="background: #F5F5F5; padding: 5px;" |? | |||
| style="background: #F5F5F5; padding: 5px;" |? | |||
| style="background: #F5F5F5; padding: 5px;" |? | |||
| style="background: #F5F5F5; padding: 5px;" |? | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" |History of hypertension | |||
| style="background: #F5F5F5; padding: 5px;" |Delirium, cortical blindness, cerebral edema, seizure | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Wernicke's Encephalopathy|Wernicke’s encephalopathy]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" |Normal | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" |? | |||
| style="background: #F5F5F5; padding: 5px;" |? | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" |? | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" |History of alcohal abuse | |||
| style="background: #F5F5F5; padding: 5px;" |Ophthalmoplegia, confusion | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[CNS abscess]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" |? | |||
| style="background: #F5F5F5; padding: 5px;" |'''?''' leukocytes >100,000/ul, '''?''' glucose and '''?''' protien, '''?''' red blood cells, lactic acid >500mg | |||
| style="background: #F5F5F5; padding: 5px;" |Contrast enhanced MRI is more sensitive and specific, | |||
Histopathological examination of brain tissue | |||
| style="background: #F5F5F5; padding: 5px;" |? | |||
| style="background: #F5F5F5; padding: 5px;" |? | |||
| style="background: #F5F5F5; padding: 5px;" |? | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" |? | |||
| style="background: #F5F5F5; padding: 5px;" |? | |||
| style="background: #F5F5F5; padding: 5px;" |? | |||
| style="background: #F5F5F5; padding: 5px;" |? | |||
| style="background: #F5F5F5; padding: 5px;" |History of drug abuse, endocarditis, '''?''' immune status | |||
| style="background: #F5F5F5; padding: 5px;" |High grade fever, fatigue,nausea, vomiting | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Drug toxicity]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" |? | |||
| style="background: #F5F5F5; padding: 5px;" |? | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" |Lithium, Sedatives, phenytoin, carbamazepine | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Conversion disorder]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" |Diagnosis of exclusion | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" | | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |? | |||
| style="background: #F5F5F5; padding: 5px;text-align:center" | | |||
| style="background: #F5F5F5; padding: 5px;text-align:center" |? | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" | ? | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |? | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |? | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" |[[Tremor|Tremors]], [[blindness]], difficulty [[swallowing]] | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Electrolyte disturbance]] | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |'''?''' or '''?''' | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" |Depends on the cause | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" |? | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" |? | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" |Confusion, seizures | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Febrile seizure|Febrile seizures]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |Not performed in first simple febrile seizures | |||
| style="background: #F5F5F5; padding: 5px;" |Clinical diagnosis and EEG | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" | ? | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |? | |||
| style="background: #F5F5F5; padding: 5px;" |? | |||
| style="background: #F5F5F5; padding: 5px;" |? | |||
| style="background: #F5F5F5; padding: 5px;" |Family history of febrile seizures, viral illness or gastroenteritis | |||
| style="background: #F5F5F5; padding: 5px;" |Age > 1 month, | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Subdural empyema]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |? | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" | | |||
| style="background: #F5F5F5; padding: 5px;" |Clinical assesment and [[MRI]] | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |? | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |? | |||
| style="background: #F5F5F5; padding: 5px;" |? | |||
| style="background: #F5F5F5; padding: 5px;" |? | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |? | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |? | |||
| style="background: #F5F5F5; padding: 5px;" |History of relapses and remissions | |||
| style="background: #F5F5F5; padding: 5px;" |Blurry vision, [[urinary incontinence]], [[fatigue]] | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Hypoglycemia]] | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |? or '''?''' | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" |Serum blood [[Glucose-1-phosphate adenylyltransferase|glucose]] | |||
[[HbA1c]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" |? | |||
| style="background: #F5F5F5; padding: 5px;text-align:center" | | |||
| style="background: #F5F5F5; padding: 5px;text-align:center" | | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" | ? | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" | | |||
| style="background: #F5F5F5; padding: 5px;" |? | |||
| style="background: #F5F5F5; padding: 5px;" |History of [[Diabetes mellitus|diabetes]] | |||
| style="background: #F5F5F5; padding: 5px;" |[[Palpitation|Palpitations]], sweating, [[dizziness]], low serum, glucose | |||
|} | |||
==Epidemiology and Demographics== | ==Epidemiology and Demographics== | ||
Revision as of 21:41, 6 September 2017
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief:
| Wernicke encephalopathy | |
 | |
|---|---|
| Thiamine | |
| ICD-10 | E51.2 |
| ICD-9 | 265.1 |
| eMedicine | emerg/642 |
Overview
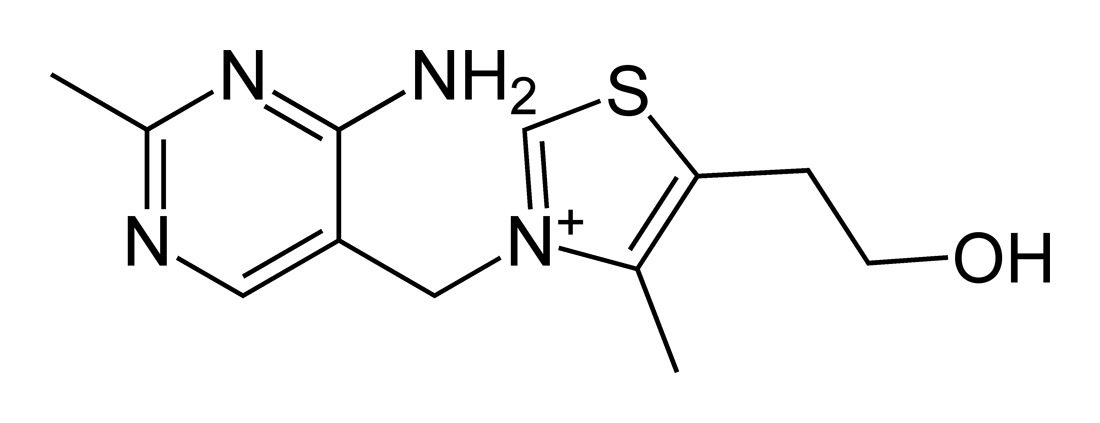
Wernicke encephalopathy is a severe syndrome characterised by ataxia, ophthalmoplegia, confusion and loss of short-term memory.[1][2] It is linked to damage to the medial thalamic nuclei, mammillary bodies, periaqueductal, and periventricular brainstem nuclei , and superior cerebellar vermis. In the brain, it is the result of inadequate intake or absorption of thiamine (Vitamin B)[1] coupled with continued carbohydrate ingestion.[1] The most common cause of an onset is prolonged alcohol consumption that is sufficient enough to cause a thiamine deficiency. Alcoholics are therefore particularly at risk, but it may also occur due to other causes of malnutrition. Other causes of thiamine deficiency may be found in patients with carcinoma, chronic gastritis, or continuous vomiting.[3][4]
Historical Perspective
Classification
Pathophysiology
Causes
Differentiating Wernicke's encephalopathy from Other Diseases
Wernicke's encephalopathy must be differentiated from other causes of headache, altered mental status and seizures such as brain tumors and delirium trmemns.
| Diseases | Diagnostic tests | Physical Examination | Symptoms | Past medical history | Other Findings | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Na+, K+, Ca2+ | CT /MRI | CSF Findings | Gold standard test | Neck stiffness | Motor or Sensory deficit | Papilledema | Bulging fontanelle | Cranial nerves | Headache | Fever | Altered mental status | |||
| Brain tumour[5][6] | ? | Cancer cells[7] | MRI | ? | ? | ? | ? | ? | ? | Cachexia, gradual progression of symptoms | ||||
| Delerium Tremens | ? | Clinical diagnosis | ? | ? | ? | ? | ? | ? | Alcohal intake, sudden witdrawl or reduction in consumption | Tachycardia, diaphoresis, hypertension, tremors, mydriasis, positional nystagmus, tachypnea | ||||
| Subarachnoid hemorrhage[8] | ? | Xanthochromia[9] | CT scan without contrast[10][11] | ? | ? | ? | ? | ? | ? | ? | ? | Trauma/fall | Confusion, dizziness, nausea, vomiting | |
| Stroke | ? | Normal | CT scan without contrast | ? | ? | ? | ? | ? | TIAs, hypertension, diabetes mellitus | Speech difficulty, gait abnormality | ||||
| Neurosyphilis[12][13] | ? | ? Leukocytes and protein | CSF VDRL-specifc
CSF FTA-Ab -sensitive[14] |
? | ? | ? | ? | ? | ? | Unprotected sexual intercourse, STIs | Blindness, confusion, depression,
Abnormal gait | |||
| Viral encephalitis | ? | Increased RBCS or xanthochromia, mononuclear lymphocytosis, high protein content, normal glucose | Clinical assesment | ? | ? | ? | ? | ? | ? | ? | Tick bite/mosquito bite/ viral prodome for several days | Extreme lethargy, rash hepatosplenomegaly, lymphadenopathy, behavioural changes | ||
| Herpes simplex encephalitis | ? | Clinical assesment | ? | ? | ? | ? | ? | History of hypertension | Delirium, cortical blindness, cerebral edema, seizure | |||||
| Wernicke’s encephalopathy | Normal | ? | ? | ? | History of alcohal abuse | Ophthalmoplegia, confusion | ||||||||
| CNS abscess | ? | ? leukocytes >100,000/ul, ? glucose and ? protien, ? red blood cells, lactic acid >500mg | Contrast enhanced MRI is more sensitive and specific,
Histopathological examination of brain tissue |
? | ? | ? | ? | ? | ? | ? | History of drug abuse, endocarditis, ? immune status | High grade fever, fatigue,nausea, vomiting | ||
| Drug toxicity | ? | ? | Lithium, Sedatives, phenytoin, carbamazepine | |||||||||||
| Conversion disorder | Diagnosis of exclusion | ? | ? | ? | ? | ? | Tremors, blindness, difficulty swallowing | |||||||
| Electrolyte disturbance | ? or ? | Depends on the cause | ? | ? | Confusion, seizures | |||||||||
| Febrile seizures | Not performed in first simple febrile seizures | Clinical diagnosis and EEG | ? | ? | ? | ? | Family history of febrile seizures, viral illness or gastroenteritis | Age > 1 month, | ||||||
| Subdural empyema | ? | Clinical assesment and MRI | ? | ? | ? | ? | ? | ? | History of relapses and remissions | Blurry vision, urinary incontinence, fatigue | ||||
| Hypoglycemia | ? or ? | Serum blood glucose | ? | ? | ? | History of diabetes | Palpitations, sweating, dizziness, low serum, glucose | |||||||
Epidemiology and Demographics
Risk Factors
Screening
Natural History, Complications, and Prognosis
Natural History
Complications
Prognosis
Diagnosis
Diagnostic Criteria
History and Symptoms
Physical Examination
Wernicke encephalopathy onsets acutely, and usually presents with nystagmus, gaze palsies, ophthalmoplegia (especially of the abducens nerve, CN VI), gait ataxia, confusion, and short-term memory loss.
The classic triad for this disease is encephalopathy, ophthalmoplegia, and ataxia. Untreated, this condition may progress to Korsakoff's psychosis or coma.[1][2] Despite its name, Wernicke's encephalopathy is not related to damage of the speech and language interpretation area named Wernicke's area (see Wernicke's aphasia). Instead the pathological changes in Wernicke's encephalopathy are concentrated in the mammillary bodies, cranial nerve nuclei III, IV, VI and VIII, as well as the thalamus, hypothalamus, periaquiductal grey, cerebellar vermis and the dorsal nucleus of the vagus nerve. The ataxia and ophthalmoparesis relate to lesions in the oculomotor (ie IIIrd, IVth, and VIth nerves) and vestibular (ie VIIIth nerve) nuclei.
Laboratory Findings
Imaging Findings
Other Diagnostic Studies
Treatment
Medical Therapy
Treatment includes an intravenous (IV) or intramuscular (IM) injection of thiamine, prior to the assessment of other central nervous system (CNS) diseases or other metabolic disturbances. Patients are usually dehydrated, and so rehydration to restore blood volume should be started. If the condition is treated early, recovery may be rapid and complete.
In individuals with sub-clinical thiamine deficiency, a large dose of glucose (either as sweet food etc or glucose infusion), can precipitate the onset of overt encephalopathy. Glucose loading results in metabolic disturbances in the brain that exacerbate the signs and symptoms of encephalopathy, and may trigger cellular processes leading to brain damage. [15]. If the patient is hypoglycemic (common in alcoholism), a thiamin injection should always precede the glucose infusion.
Surgery
Prevention
See also
External links
References
- ↑ 1.0 1.1 1.2 1.3 Aminoff, Michael J, Greenberg, David A., Simon, Roger P. (2005) Clinical Neurology (6th ed.). page 113 Lange Medical Books/McGraw-Hill. ISBN 0-07-142360-5
- ↑ 2.0 2.1 Beers, Mark H. et al (2006), The Merck Manual of Diagnosis and Therapy (18th ed.), pages 1688-1689, Merk Research Laboratories 2006, ISBN 0911910-18-2
- ↑ Kumar, Vinay, Abbas, Abul K., Fausto, Nelson (2005), Pathologic Basis of Disease (7th ed.), page 1399, Elsevier Saunders. ISBN 0-8089-2302-1
- ↑ Sullivan, Joseph; Hamilton, Roy; Hurford, Matthew; Galetta, Steven L; Liu Grant T (2006), "Neuro-Opthalmic Findings in Wernicke's Encephalopathy after Gastric Bypass Surgery", Neuro-Ophthalmology, Jul/Aug2006, Vol. 30 Issue 4, p85-89
- ↑ Soffer D (1976) Brain tumors simulating purulent meningitis. Eur Neurol 14 (3):192-7. PMID: 1278192
- ↑
- ↑ Weston CL, Glantz MJ, Connor JR (2011). "Detection of cancer cells in the cerebrospinal fluid: current methods and future directions". Fluids Barriers CNS. 8 (1): 14. doi:10.1186/2045-8118-8-14. PMC 3059292. PMID 21371327.
- ↑ Yeh ST, Lee WJ, Lin HJ, Chen CY, Te AL, Lin HJ (2003) Nonaneurysmal subarachnoid hemorrhage secondary to tuberculous meningitis: report of two cases. J Emerg Med 25 (3):265-70. PMID: 14585453
- ↑ Lee MC, Heaney LM, Jacobson RL, Klassen AC (1975). "Cerebrospinal fluid in cerebral hemorrhage and infarction". Stroke. 6 (6): 638–41. PMID 1198628.
- ↑ Birenbaum D, Bancroft LW, Felsberg GJ (2011). "Imaging in acute stroke". West J Emerg Med. 12 (1): 67–76. PMC 3088377. PMID 21694755.
- ↑ DeLaPaz RL, Wippold FJ, Cornelius RS, Amin-Hanjani S, Angtuaco EJ, Broderick DF; et al. (2011). "ACR Appropriateness Criteria® on cerebrovascular disease". J Am Coll Radiol. 8 (8): 532–8. doi:10.1016/j.jacr.2011.05.010. PMID 21807345.
- ↑ Liu LL, Zheng WH, Tong ML, Liu GL, Zhang HL, Fu ZG; et al. (2012). "Ischemic stroke as a primary symptom of neurosyphilis among HIV-negative emergency patients". J Neurol Sci. 317 (1–2): 35–9. doi:10.1016/j.jns.2012.03.003. PMID 22482824.
- ↑ Berger JR, Dean D (2014). "Neurosyphilis". Handb Clin Neurol. 121: 1461–72. doi:10.1016/B978-0-7020-4088-7.00098-5. PMID 24365430.
- ↑ Ho EL, Marra CM (2012). "Treponemal tests for neurosyphilis--less accurate than what we thought?". Sex Transm Dis. 39 (4): 298–9. doi:10.1097/OLQ.0b013e31824ee574. PMC 3746559. PMID 22421697.
- ↑ Zimitat C, Nixon P, (2000). "Glucose loading precipitates encephalopathy in thiamine-deficient rats". Metabolic Brain Disease. 14 (1): 1–10.
Template:Nutritional pathology