WBR0097: Difference between revisions
No edit summary |
m (refreshing WBR questions) |
||
| (24 intermediate revisions by 4 users not shown) | |||
| Line 1: | Line 1: | ||
{{WBRQuestion | {{WBRQuestion | ||
|QuestionAuthor=William J Gibson | |QuestionAuthor=William J Gibson (Reviewed by {{YD}}, {{Rim}}) | ||
|ExamType=USMLE Step 1 | |ExamType=USMLE Step 1 | ||
|MainCategory=Genetics | |MainCategory=Genetics | ||
|SubCategory=Hematology | |SubCategory=Hematology | ||
|MainCategory=Genetics | |MainCategory=Genetics | ||
|SubCategory=Hematology | |SubCategory=Hematology | ||
|MainCategory=Genetics | |MainCategory=Genetics | ||
|SubCategory=Hematology | |SubCategory=Hematology | ||
|MainCategory=Genetics | |MainCategory=Genetics | ||
|MainCategory=Genetics | |MainCategory=Genetics | ||
|MainCategory=Genetics | |||
|SubCategory=Hematology | |SubCategory=Hematology | ||
|MainCategory=Genetics | |MainCategory=Genetics | ||
|SubCategory=Hematology | |SubCategory=Hematology | ||
|MainCategory=Genetics | |MainCategory=Genetics | ||
|SubCategory=Hematology | |SubCategory=Hematology | ||
|MainCategory=Genetics | |MainCategory=Genetics | ||
|SubCategory=Hematology | |SubCategory=Hematology | ||
|MainCategory=Genetics | |MainCategory=Genetics | ||
|MainCategory=Genetics | |MainCategory=Genetics | ||
|SubCategory=Hematology | |SubCategory=Hematology | ||
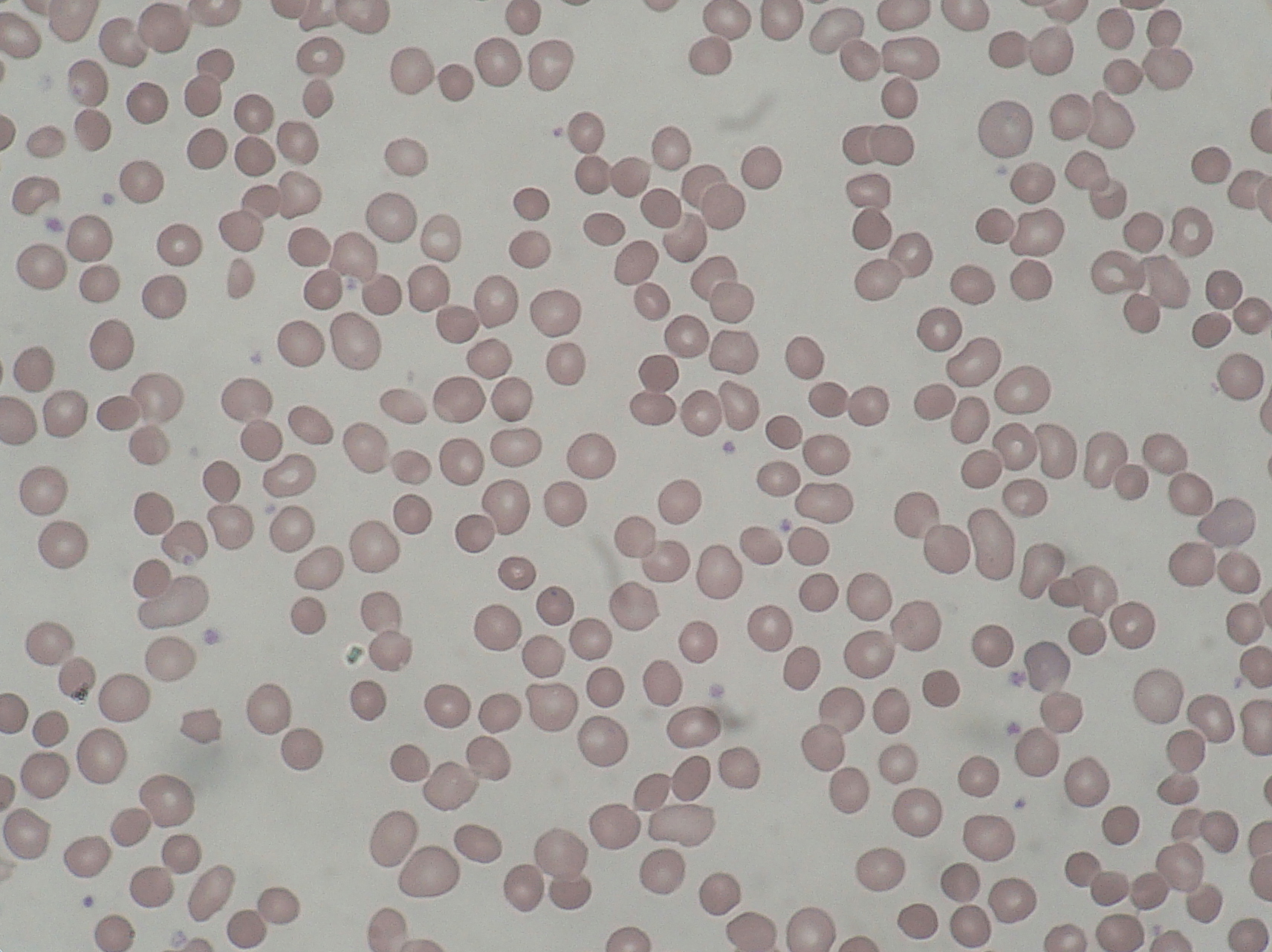
|Prompt=A 3 week old | |Prompt=A 3-week-old infant is brought to the pediatric emergency department (ED) by his mother for abdominal colics and yellowish skin that first appeared 2 days ago. The mother reports the patient is a product of an uncomplicated normal vaginal delivery and his neonatal course was uneventful. He is currently receiving formula milk. In the ED, physical examination is remarkable for jaundiced skin and icterus; his spleen is soft, non-tender, and easily palpable 4 cm below the left costal margin. Laboratory values reveal decreased RBC count and unconjugated hyperbilirubinemia. A peripheral blood smear from the patient is shown below. Which of the following is most likely responsible for this infant's condition? | ||
[[File:WBR0097.JPG|600px]] | |||
|Explanation=Hereditary sphereocytosis is an autosomal dominant genetic disease that is considered the most common red cell membrane disorder. Clinical presentation is typically during infancy; the hallmark is [[jaundice]], fatigue, and [[splenomegaly]]. Lab values reveal signs of hemolysis, such as elevated [[lactic dehydrogenase]] activity, low [[haptoglobin]], [[microcytic anemia]], especially with elevated [[mean corpuscular hemoglobin concentration]] (MCHC), [[reticulocytosis]], and [[unconjugated hyperbilirubinemia]]. Peripheral blood smear characteristically shows spherocytes, defined as small red blood cells that lack any central pallor. [[Howell-Jolly bodies]] may also be seen within red blood cells on peripheral smear. Acute cases can cause hypoxia due to anemia and acute [[kernicterus]] among newborns due to [[hyperbilirubinemia]]. Cholecystitis is very common among older patients with hereditary spherocytosis because patients eventually develop bilirubin stones due to the chronic hemolysis associated with the disease. In particular, these patients may develop aplastic anemia with [[Parvovirus B19]] infection. | |||
|AnswerA=Mutation of glutamic acid to valine in the Beta globin gene | |||
| | Hereditary spherocytosis is caused by a variety of molecular defects, all of which eventually cause a deficiency of spectrin leading to unstable red cell membrane and change of its appearance from a biconcave shape to a sphere. Common mutations include those in the genes that code for [[spectrin]] (alpha and beta), [[ankyrin]], band 3 protein, protein 4.2, and other erythrocyte membrane proteins. Mutations in ankyrin are the most common and are thought to account for approximately 35 to 65 percent of cases. | ||
Common diagnostic tests for [[hereditary spherocytosis]] are the [[osmotic fragility test]], [[acidified glycerol lysis test]] (AGLT), and [[eosin-5-maleimide binding test]]. Management of patients with hereditary spherocytosis includes close follow-up, and iron and folic acid supplementation if anemia is not too severe. In cases of severe anemia, poor growth, chronic fatigue, and extramedullary hematopoiesis, [[splenectomy]] should be considered. Transfusions are generally not required except in cases of severe anemia and fatigue, hypersplenism, and hypoplastic crisis due to [[parvovirus B19]] virus infection. | |||
|AnswerA=Mutation of glutamic acid to valine in the beta globin gene | |||
|AnswerAExp=A missense mutation of the sixth amino acid of the beta-globin gene to [[valine]] causes [[sickle cell anemia]]. [[Beta globin]] mutations are not associated with [[hereditary spherocytosis]]. | |||
|AnswerB=Mutation of three copies of the alpha globin gene | |||
|AnswerBExp=Mutation of three copies of the alpha globin gene cause the hemoglobin [[H disease]], a subtype of [[alpha thalassemia]]. | |||
|AnswerC=Mutation of ankyrin | |AnswerC=Mutation of ankyrin | ||
|AnswerD=Mutation of | |AnswerCExp=[[Ankyrin]] mutations are the most common genetic disorder of [[hereditary spherocytosis]]. Ankyrin normally serves as the binding partner for [[spectrin]] and allows spectrin to be incorporated into cell membranes. [[Ankyrin]] deficiency therefore causes a decrease in [[spectrin]] localization to the [[RBC]] membrane. | ||
|AnswerE=Nonsense mutation in the beta | |AnswerD=Mutation of spectrin | ||
|AnswerDExp=[[Spectrin]] deficiency is common to all forms of hereditary spherocytosis. However, spectrin deficiency is more often secondary to [[ankyrin]] mutations than to [[spectrin]] mutations. | |||
|AnswerE=Nonsense mutation in the beta globin gene | |||
|AnswerEExp=Nonsense mutations of the beta globin gene cause [[beta thalassemia]]. A missense mutation of glutamic acid to valine at position 6 of the beta globin gene causes [[sickle cell anemia]]. Beta globin mutations are not associated with [[hereditary spherocytosis]]. | |||
|EducationalObjectives=[[Hereditary spherocytosis]] is a genetic disorder that causes RBC membrane instability. It is commonly due to mutations in the [[ankyrin]] gene that lead to spectrin deficiency. | |||
|References=Eber SW, Gonzalez JM, Lux ML, et al. Ankyrin-1 mutations are a major cause of dominant and recessive hereditary spherocytosis. Nat Genet. 1996;13(2):214-8. | |||
Shah H, Vega R. Hereditary spherocytosis. Pediatr Rev. 2004;25(5):168-72 | |||
First Aid 2014 page 386 | |||
|RightAnswer=C | |RightAnswer=C | ||
|WBRKeyword=Hematology, Hereditary spherocytosis, Spherocytosis, RBC, osmotic, fragility, test, splenectomy, jaundice, anemia, hemolytic, hemolysis, splenomegaly, infant, neonate, newborn, peripheral, smear, mutation, genetic, genetics, spectrin, ankyrin, red, cell, membrane | |||
|Approved=Yes | |Approved=Yes | ||
}} | }} | ||
Latest revision as of 23:20, 27 October 2020
| Author | [[PageAuthor::William J Gibson (Reviewed by Yazan Daaboul, M.D., Rim Halaby, M.D. [1])]] |
|---|---|
| Exam Type | ExamType::USMLE Step 1 |
| Main Category | MainCategory::Genetics |
| Sub Category | SubCategory::Hematology |
| Prompt | [[Prompt::A 3-week-old infant is brought to the pediatric emergency department (ED) by his mother for abdominal colics and yellowish skin that first appeared 2 days ago. The mother reports the patient is a product of an uncomplicated normal vaginal delivery and his neonatal course was uneventful. He is currently receiving formula milk. In the ED, physical examination is remarkable for jaundiced skin and icterus; his spleen is soft, non-tender, and easily palpable 4 cm below the left costal margin. Laboratory values reveal decreased RBC count and unconjugated hyperbilirubinemia. A peripheral blood smear from the patient is shown below. Which of the following is most likely responsible for this infant's condition? |
| Answer A | AnswerA::Mutation of glutamic acid to valine in the beta globin gene |
| Answer A Explanation | [[AnswerAExp::A missense mutation of the sixth amino acid of the beta-globin gene to valine causes sickle cell anemia. Beta globin mutations are not associated with hereditary spherocytosis.]] |
| Answer B | AnswerB::Mutation of three copies of the alpha globin gene |
| Answer B Explanation | [[AnswerBExp::Mutation of three copies of the alpha globin gene cause the hemoglobin H disease, a subtype of alpha thalassemia.]] |
| Answer C | AnswerC::Mutation of ankyrin |
| Answer C Explanation | [[AnswerCExp::Ankyrin mutations are the most common genetic disorder of hereditary spherocytosis. Ankyrin normally serves as the binding partner for spectrin and allows spectrin to be incorporated into cell membranes. Ankyrin deficiency therefore causes a decrease in spectrin localization to the RBC membrane.]] |
| Answer D | AnswerD::Mutation of spectrin |
| Answer D Explanation | [[AnswerDExp::Spectrin deficiency is common to all forms of hereditary spherocytosis. However, spectrin deficiency is more often secondary to ankyrin mutations than to spectrin mutations.]] |
| Answer E | AnswerE::Nonsense mutation in the beta globin gene |
| Answer E Explanation | [[AnswerEExp::Nonsense mutations of the beta globin gene cause beta thalassemia. A missense mutation of glutamic acid to valine at position 6 of the beta globin gene causes sickle cell anemia. Beta globin mutations are not associated with hereditary spherocytosis.]] |
| Right Answer | RightAnswer::C |
| Explanation | [[Explanation::Hereditary sphereocytosis is an autosomal dominant genetic disease that is considered the most common red cell membrane disorder. Clinical presentation is typically during infancy; the hallmark is jaundice, fatigue, and splenomegaly. Lab values reveal signs of hemolysis, such as elevated lactic dehydrogenase activity, low haptoglobin, microcytic anemia, especially with elevated mean corpuscular hemoglobin concentration (MCHC), reticulocytosis, and unconjugated hyperbilirubinemia. Peripheral blood smear characteristically shows spherocytes, defined as small red blood cells that lack any central pallor. Howell-Jolly bodies may also be seen within red blood cells on peripheral smear. Acute cases can cause hypoxia due to anemia and acute kernicterus among newborns due to hyperbilirubinemia. Cholecystitis is very common among older patients with hereditary spherocytosis because patients eventually develop bilirubin stones due to the chronic hemolysis associated with the disease. In particular, these patients may develop aplastic anemia with Parvovirus B19 infection.
Hereditary spherocytosis is caused by a variety of molecular defects, all of which eventually cause a deficiency of spectrin leading to unstable red cell membrane and change of its appearance from a biconcave shape to a sphere. Common mutations include those in the genes that code for spectrin (alpha and beta), ankyrin, band 3 protein, protein 4.2, and other erythrocyte membrane proteins. Mutations in ankyrin are the most common and are thought to account for approximately 35 to 65 percent of cases. Common diagnostic tests for hereditary spherocytosis are the osmotic fragility test, acidified glycerol lysis test (AGLT), and eosin-5-maleimide binding test. Management of patients with hereditary spherocytosis includes close follow-up, and iron and folic acid supplementation if anemia is not too severe. In cases of severe anemia, poor growth, chronic fatigue, and extramedullary hematopoiesis, splenectomy should be considered. Transfusions are generally not required except in cases of severe anemia and fatigue, hypersplenism, and hypoplastic crisis due to parvovirus B19 virus infection. Shah H, Vega R. Hereditary spherocytosis. Pediatr Rev. 2004;25(5):168-72 First Aid 2014 page 386]] |
| Approved | Approved::Yes |
| Keyword | WBRKeyword::Hematology, WBRKeyword::Hereditary spherocytosis, WBRKeyword::Spherocytosis, WBRKeyword::RBC, WBRKeyword::osmotic, WBRKeyword::fragility, WBRKeyword::test, WBRKeyword::splenectomy, WBRKeyword::jaundice, WBRKeyword::anemia, WBRKeyword::hemolytic, WBRKeyword::hemolysis, WBRKeyword::splenomegaly, WBRKeyword::infant, WBRKeyword::neonate, WBRKeyword::newborn, WBRKeyword::peripheral, WBRKeyword::smear, WBRKeyword::mutation, WBRKeyword::genetic, WBRKeyword::genetics, WBRKeyword::spectrin, WBRKeyword::ankyrin, WBRKeyword::red, WBRKeyword::cell, WBRKeyword::membrane |
| Linked Question | Linked:: |
| Order in Linked Questions | LinkedOrder:: |