Ventricular tachycardia diagnosis
Template:Ventricular Tachycardia
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Please Take Over This Page and Apply to be Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [3] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
The diagnosis of ventricular tachycardia is made based on the rhythm seen on either a 12 lead EKG or a telemetry rhythm strip. It may be very difficult to differentiate between ventricular tachycardia and a wide-complex supraventricular tachycardia in some cases. In particular, supraventricular tachycardias with aberrant conduction from pre-existing bundle branch block are commonly misdiagnosed as ventricular tachycardia. Other rarer phenomena include ashman beats and antedromic atrioventricular re-entry tachcyardias.
Various diagnostic criteria have been developed to determine if a wide complex tachycardia is ventricular tachycardia or a more benign rhythm.[1][2] In addition to these diagnostic criteria, if the individual has a past history of a myocardial infarction, congestive heart failure, or recent angina, the wide complex tachycardia is much more likely to be ventricular tachycardia.[3]
The proper diagnosis is important, as the misdiagnosis of supraventricular tachycardia when ventricular tachycardia is present is associated with worse prognosis. This is particularly true if calcium channel blockers, such as verapamil are used to attempt to terminate a presumed supraventricular tachycardia.[4] It is therefore wisest to assume that all wide complex tachycardia is VT until proven otherwise.
EKG Findings
- Abnormal and wide QRS complexes with secondary ST segment and T wave changes.
- Usual QRS duration is > 0.12 seconds, may be shorter if the ectopic focus is located in the ventricular septum.
- The secondary ST segment and T wave changes are in a direction that is opposite the major deflection of the QRS.
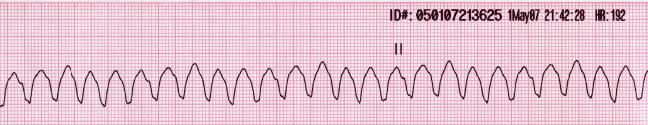
- A ventricular rate between 140 and 200 BPM.
- When the rate is >200 and has a sine wave appearance, it is called ventricular flutter.
- When the rate is <110 BPM it is called non-paroxysmal VT.
- A regular or slightly irregular (up to 0.03 seconds) rhythm.
- Abrupt onset and termination.
- AV dissociation.
- Atrial rate slower than ventricular rate.
- No relationship between atrial activity and ventricular activity.
- There can be VA conduction.
- The RP interval is >0.11 seconds.
- Occurs in about 50% of cases.
- Uncommon when the ventricular rate is rapid (only 1/7 when the rate was>200).
- Capture beats.
- Occurs when a supraventricular impulse is conducted and captures the ventricle.
- They are rare.
- Fusion beats.
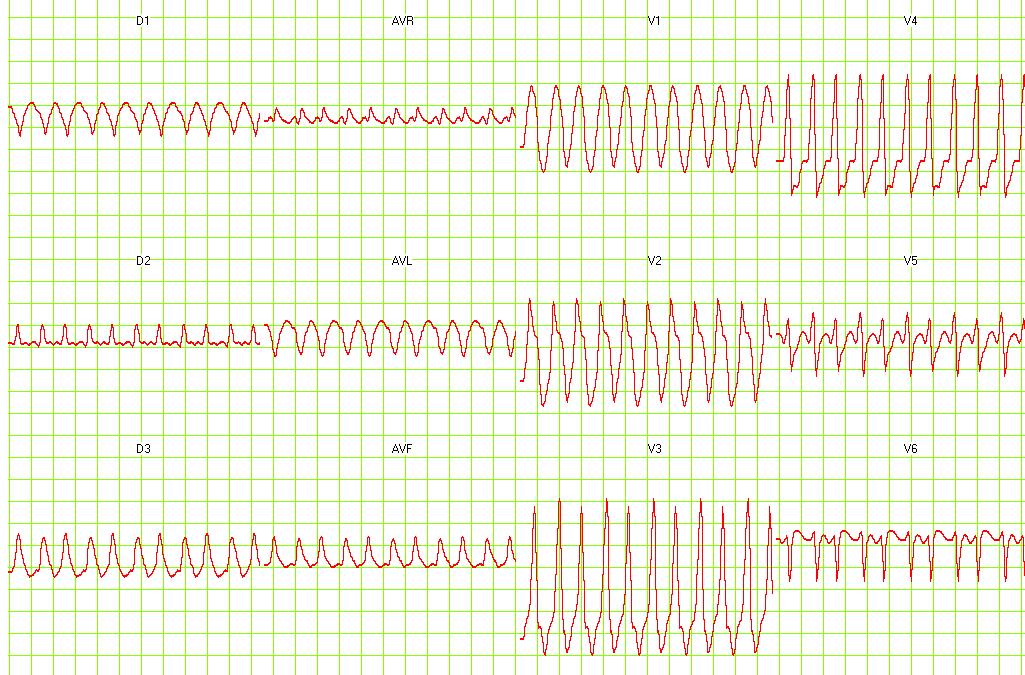
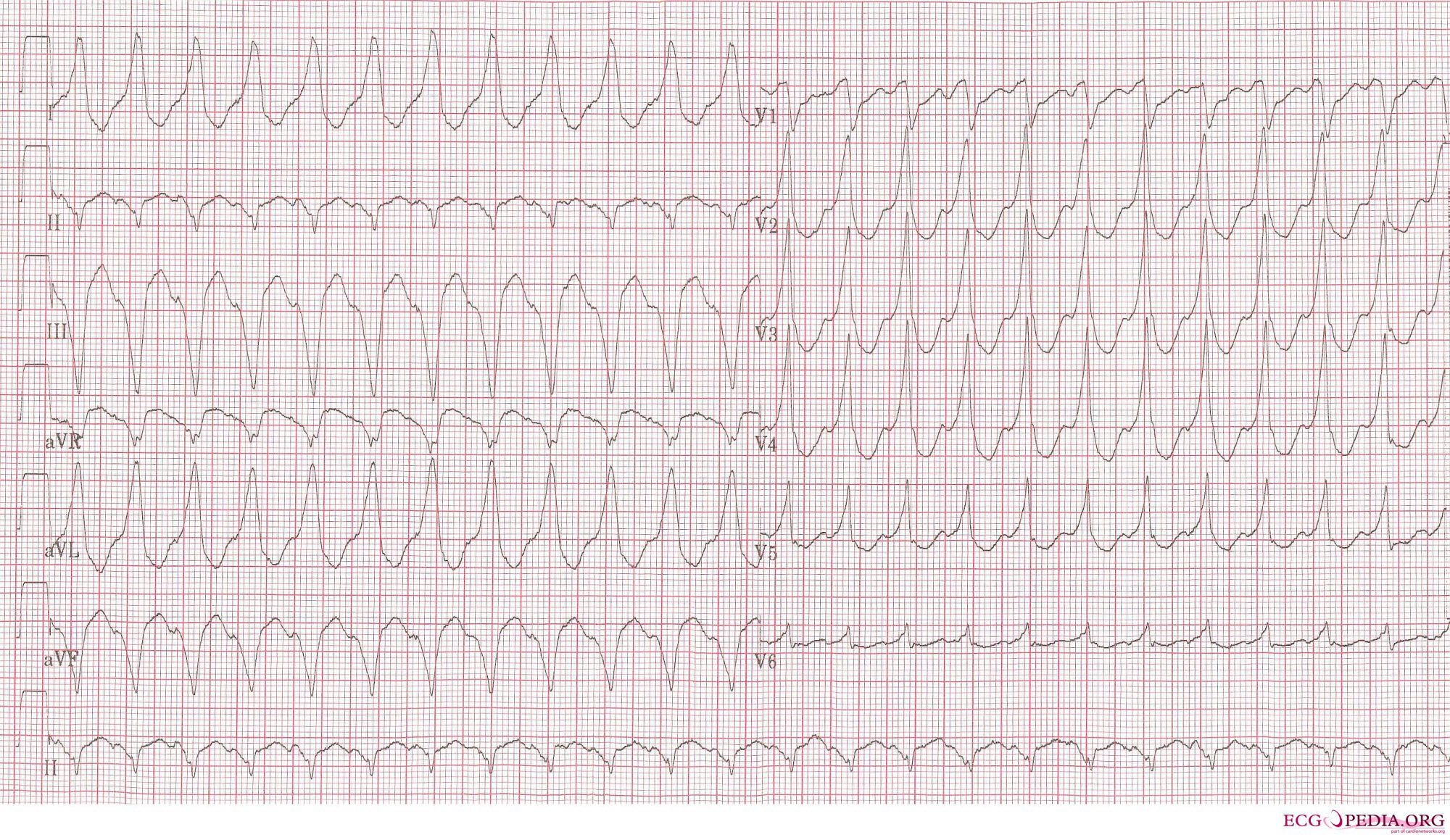
Examples of Ventricular Tachycardia:
-
12 lead EKG: Ventricular tachycardia.
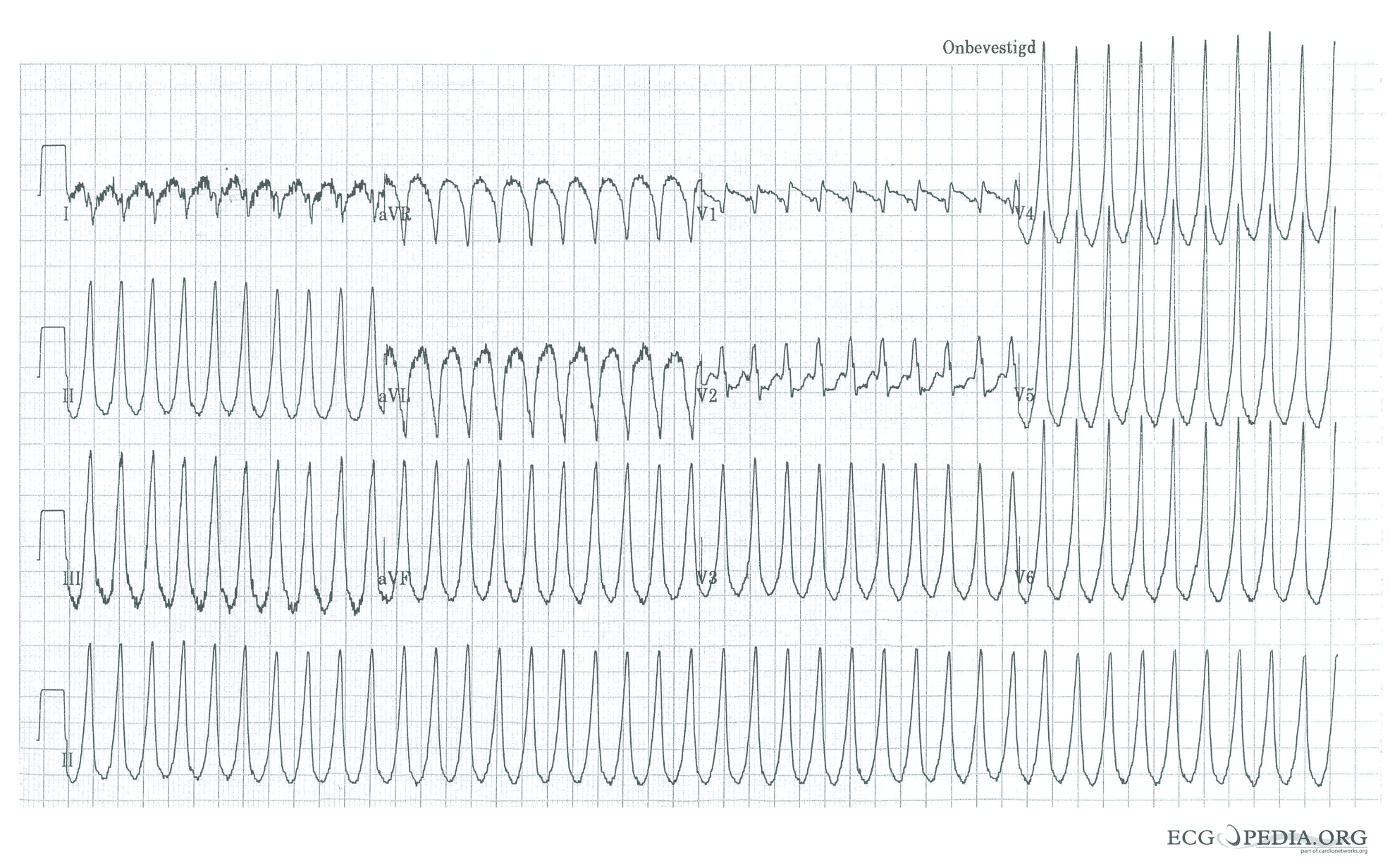
-
12 lead EKG: Ventricular tachycardia. Image courtesy of Dr Jose Ganseman
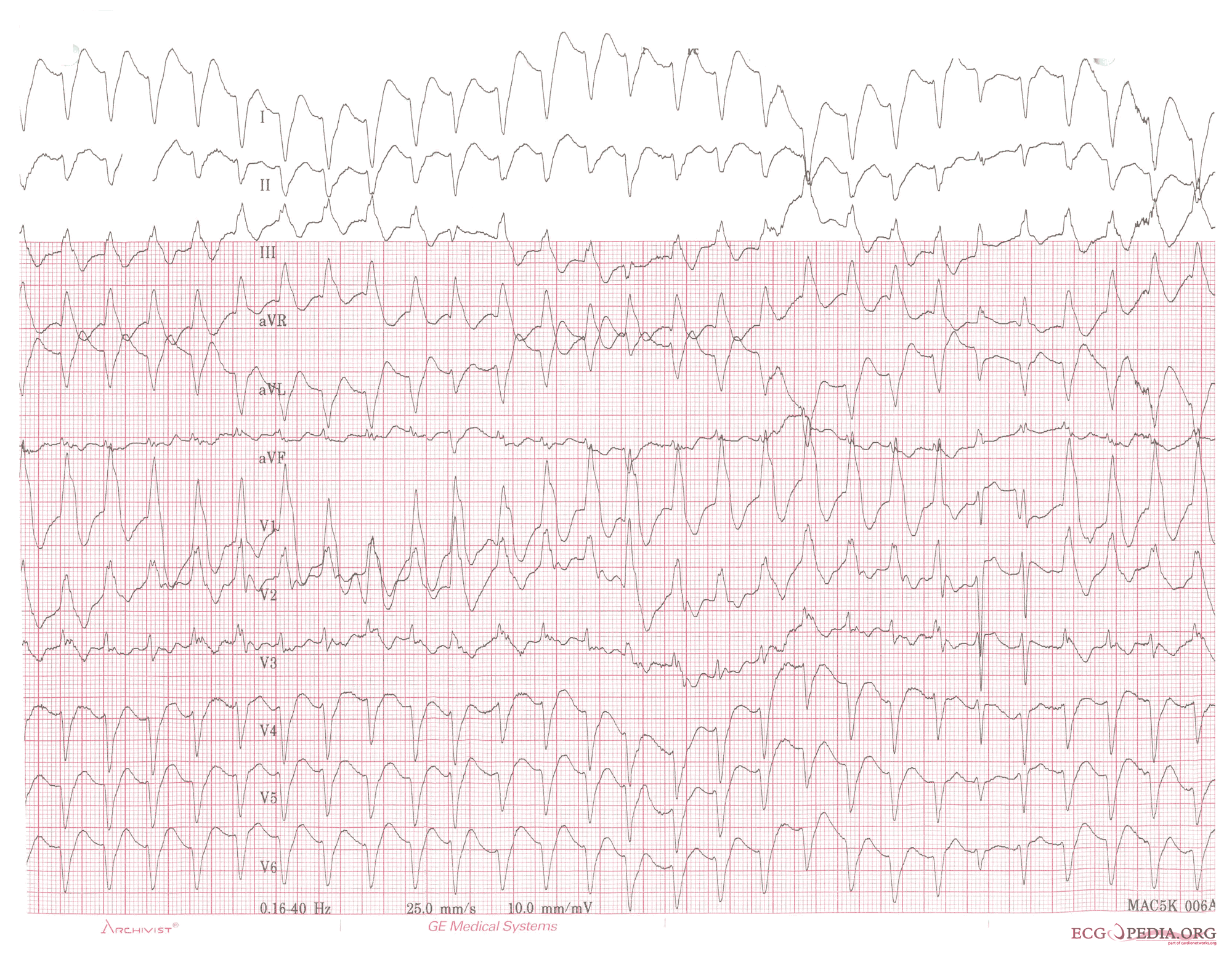
-
12 lead EKG: Ventricular tachycardia. Image courtesy of Dr Jose Ganseman
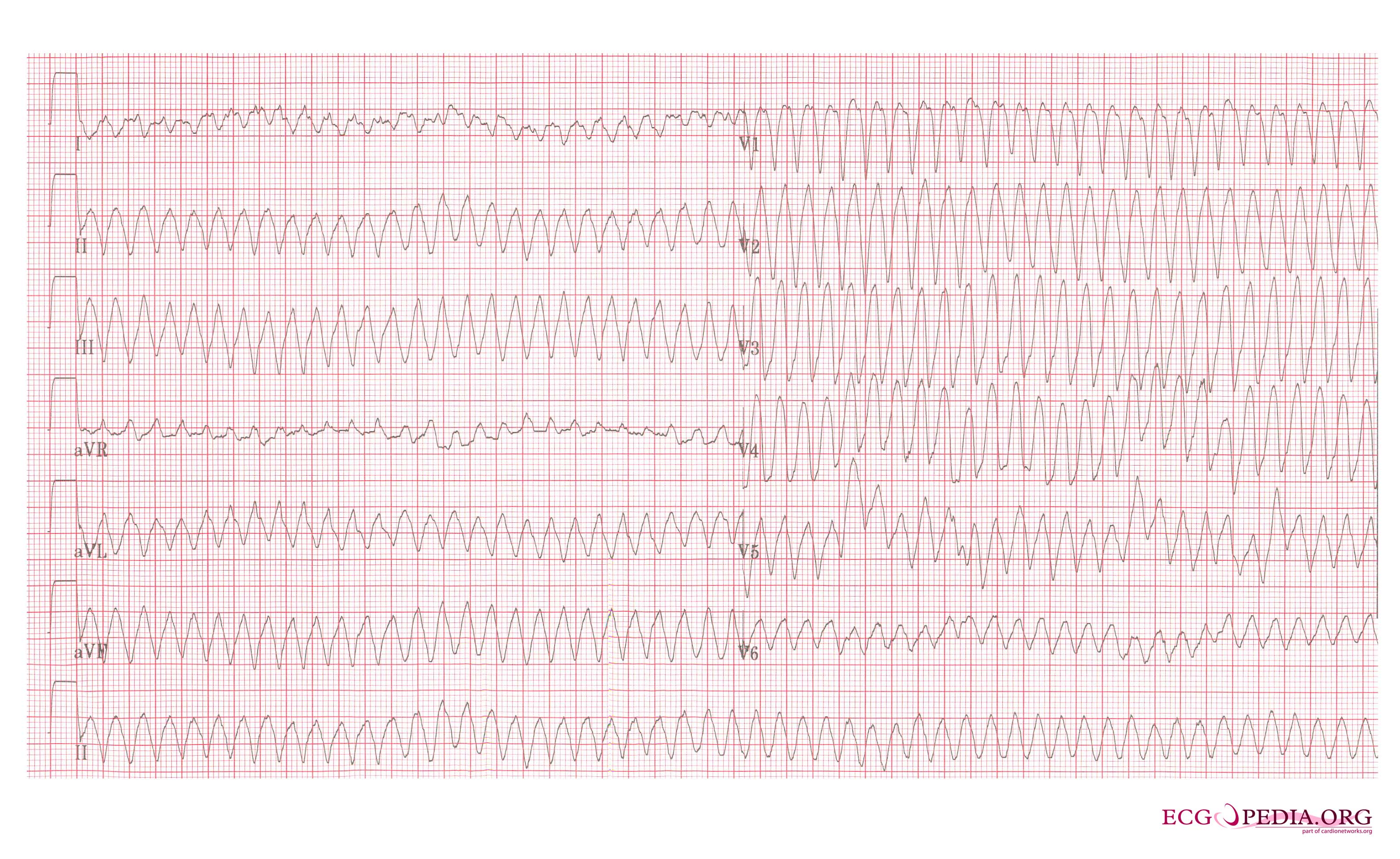
-
12 lead EKG: Ventricular tachycardia. Image courtesy of Dr Jose Ganseman
-
12 lead EKG: Ventricular tachycardia. Image courtesy of Dr Jose Ganseman
-
12 lead EKG: Ventricular tachycardia. Image courtesy of Dr Jose Ganseman
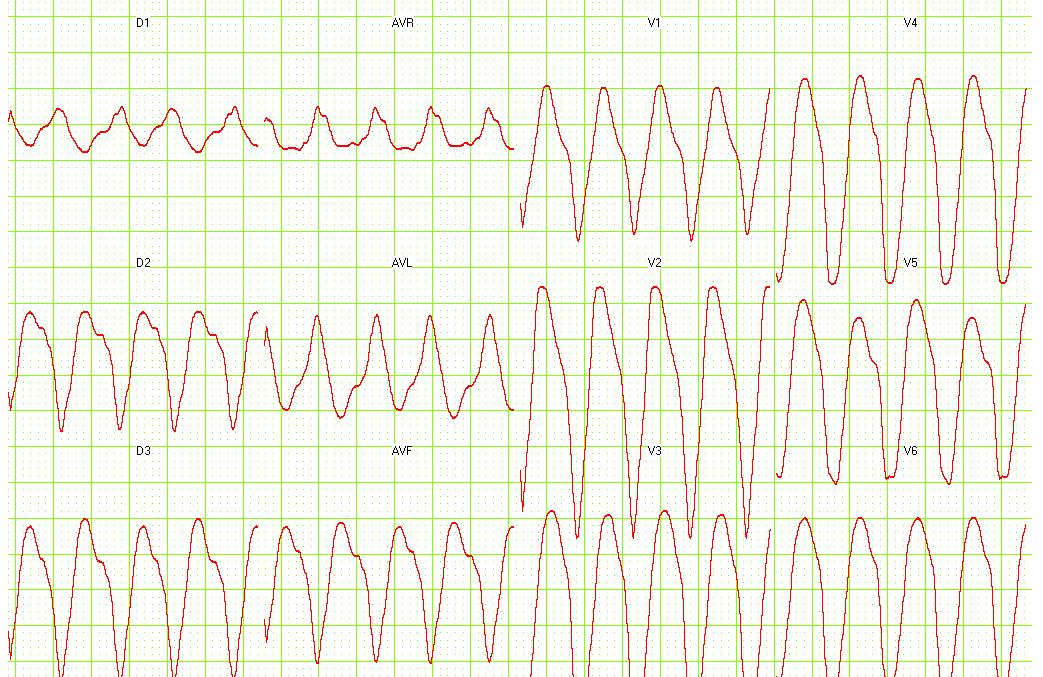
-
Ventricular tachycardia of 140 bpm with a left bundle branch block pattern and left heart axis.
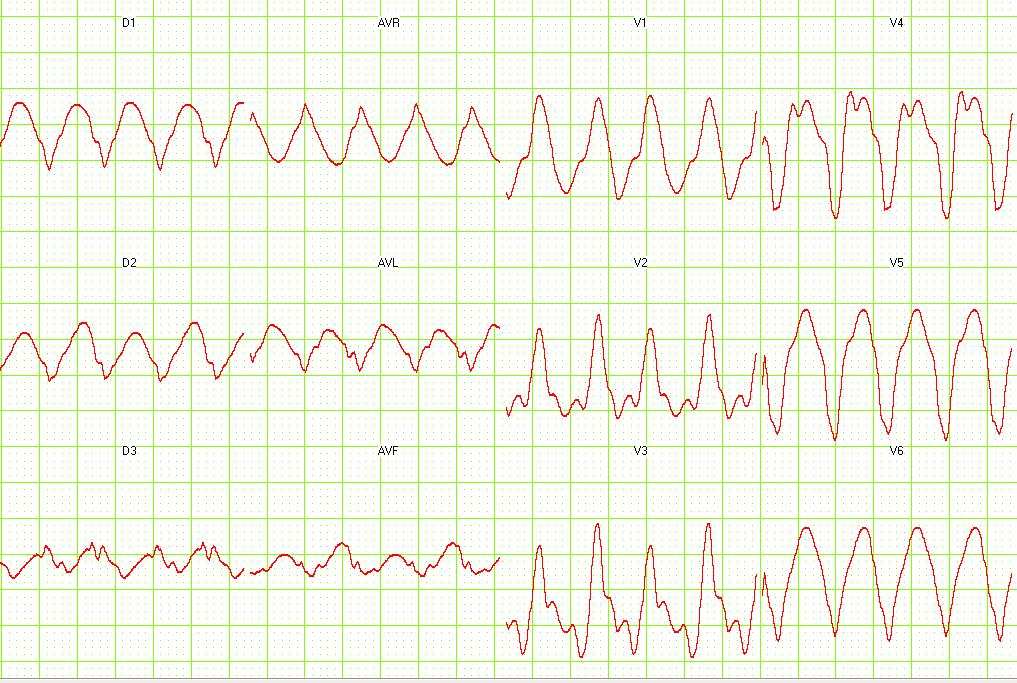
-
Ventricular tachycardia of 250 bpm with a right bundle branch block pattern and right heart axis.
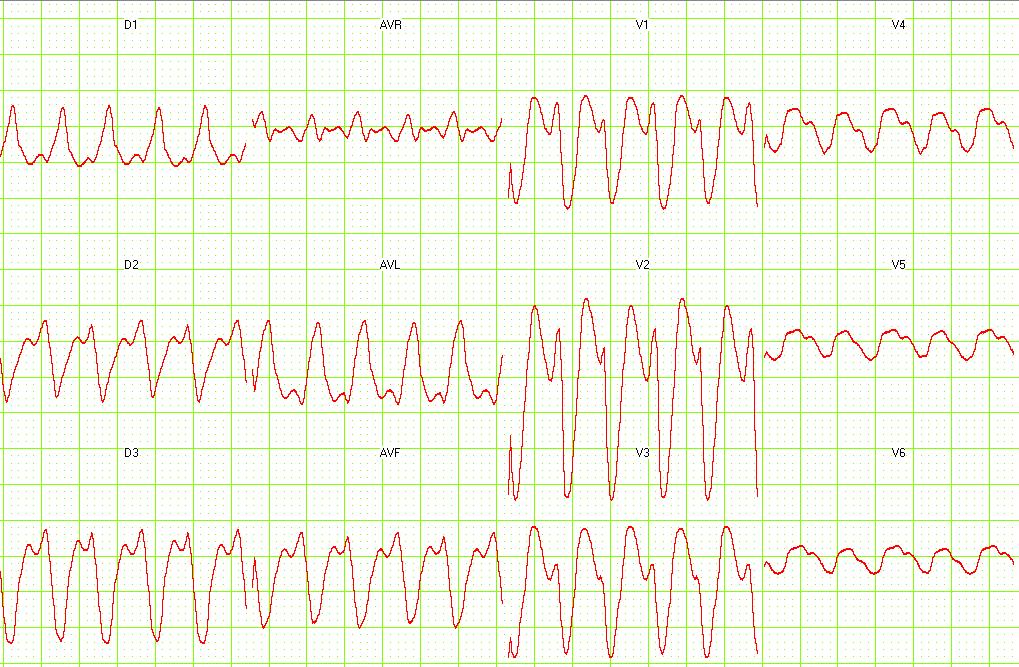
-
Ventricular tachycardia of 150 bpm with a right bundle branch block pattern and right heart axis. Note the 5th and 6th complex from the right side. These are fusion complexes.
-
Ventricular flutter on a 12 lead ECG
Differential Diagnosis of Underlying Causes of Ventricular Tachycardia
- Caffeine
- Cardiomyopathy
- Cocaine
- Congenital Heart Disease
- Congestive heart failure
- Electrolyte imbalance
- Hypertrophic cardiomyopathy
- Hypocalcemia
- Hypokalemia
- Hypomagnesia
- Iatrogenic due to pulmonary artery catheter, right heart catheterization, or electrophysiologic sutdy
- Methamphetamine
- STEMI
- Ventricular aneurysm
References
- ↑ Wellens HJ, Bar FW, Lie KI. (1978). "The value of the electrocardiogram in the differential diagnosis of a tachycardia with a widened QRS complex". Am J Med. 64 (1): 27–33. PMID 623134.
- ↑ Brugada P, Brugada J, Mont L, Smeets J, Andries EW. (1991). "A new approach to the differential diagnosis of a regular tachycardia with a wide QRS complex". Circulation. 83 (5): 1649–59. PMID 2022022.
- ↑ Baerman JM, Morady F, DiCarlo LA Jr, de Buitleir M. (1987). "Differentiation of ventricular tachycardia from supraventricular tachycardia with aberration: value of the clinical history". Ann Emerg Med. 16 (1): 40–3. PMID 3800075.
- ↑ Stewart RB, Bardy GH, Greene HL. (1986). "Wide complex tachycardia: misdiagnosis and outcome after emergent therapy". Ann Intern Med. 104 (6): 766–71. PMID 3706928.
- ↑ Chou's Electrocardiography in Clinical Practice Third Edition, pp. 398-409.
- ↑ Sailer, Christian, Wasner, Susanne. Differential Diagnosis Pocket. Hermosa Beach, CA: Borm Bruckmeir Publishing LLC, 2002:194 ISBN 1591032016
- ↑ Hammill S. C. Electrocardiographic diagnoses: Criteria and definitions of abnormalities, Chapter 18, MAYO Clinic, Concise Textbook of Cardiology, 3rd edition, 2007 ISBN 0-8493-9057-5