Unstable angina / non ST elevation myocardial infarction diagnosis
| Unstable angina pectoris | |
 | |
|---|---|
| Plaque rupture in a coronary artery at arrows yielding obstructive thrombus in red. Image courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology | |
| ICD-10 | I20 |
| ICD-9 | 413 |
| DiseasesDB | 8695 |
| eMedicine | med/133 |
| MeSH | D000787 |
| Cardiology Network |
 Discuss Unstable angina / non ST elevation myocardial infarction diagnosis further in the WikiDoc Cardiology Network |
| Adult Congenital |
|---|
| Biomarkers |
| Cardiac Rehabilitation |
| Congestive Heart Failure |
| CT Angiography |
| Echocardiography |
| Electrophysiology |
| Cardiology General |
| Genetics |
| Health Economics |
| Hypertension |
| Interventional Cardiology |
| MRI |
| Nuclear Cardiology |
| Peripheral Arterial Disease |
| Prevention |
| Public Policy |
| Pulmonary Embolism |
| Stable Angina |
| Valvular Heart Disease |
| Vascular Medicine |
Template:WikiDoc Cardiology News Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Please Join in Editing This Page and Apply to be an Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [3] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Synonyms and related keywords: progressive angina, crescendo angina, accelerating angina, new-onset angina, pre-infarction angina, unstable angina pectoris, UAP, UA
Diagnosis of Unstable Angina Pectoris
Laboratory Findings
Cardiac biomarkers
If there is an elevation of a marker of myocardial necrosis (CK-MB or troponin), then the patient does not have unstable angina, but instead has a syndrome of either ST elevation MI or Non ST elevation MI depending upon the EKG changes.
The traditional definitions of MI were revisited in 2000 in a consensus document of a joint committee of the European Society of Cardiology(ESC) and American College of Cardiology(ACC). In this definition, myocardial necrosis is defined by an elevation of troponin above the 99th percentile of normal.
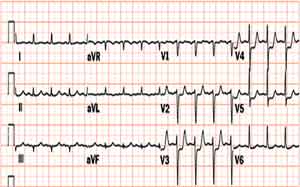
Electrocardiogram
The resting electrocardiogram may show either
- No changes
- Non specific ST T wave changes
- Flipped or inverted T waves
- ST Depression as shown below. ST depression carries the poorest prognosis. Greater magnitudes of downsloping ST depression are associated with a poorer prognosis.
Chest X Ray
A chest X-ray is critical to aid in the exclusion of aortic dissection. A mediastinal mass consistent with a cancer may be present, but it is unlikely to present with a syndrome of accelerating chest pain. The chest X ray is critical in assessing for the presence of pulmonary edema or congestive heart failure which requires urgent treatment and confers a poorer prognosis.
Echocardiography
Segmental wall motion abnormalities can occur within minutes of coronary artery occlusion and can be useful in establishing that the pain is of cardiac origin and in determining the myocardial territory that is at risk.
Coronary Angiography
An early invasive strategy including coronary angiography may be required if aggressive medical therapy fails to stabilize the patient, if prior revascularization procedures have been performed, in the presence of recurrent angina, and in the presence of abnormal non-invasive test results.
ACC / AHA Guidelines- Identification of Patients at Risk of UA/NSTEMI (DO NOT EDIT) [1]
| “ |
Class I1. Primary care providers should evaluate the presence and status of control of major risk factors for coronary heart disease (CHD) for all patients at regular intervals (approximately every 3 to 5 years). (Level of Evidence: C) 2. Ten-year risk (National Cholesterol Education Program global risk) of developing symptomatic CHD should be calculated for all patients who have 2 or more major risk factors to assess the need for primary prevention strategies (2,3). (Level of Evidence: B) 3. Patients with established CHD should be identified for secondary prevention efforts, and patients with a CHD risk equivalent (e.g., atherosclerosis in other vascular beds, diabetes mellitus, chronic kidney disease, or 10-year risk greater than 20% as calculated by Framingham equations) should receive equally intensive risk factor intervention as those with clinically apparent CHD. (Level of Evidence: A) |
” |
ACC / AHA Guidelines- Initial Evaluation and Management (Clinical Assessment) (DO NOT EDIT) [1]
| “ |
Class I1. Patients with symptoms that may represent ACS should not be evaluated solely over the telephone but should be referred to a facility that allows evaluation by a physician and the recording of a 12-lead ECG and biomarker determination (e.g., an ED or other acute care facility). (Level of Evidence: C) 2. Patients with symptoms of ACS (chest discomfort with or without radiation to the arm[s], back, neck, jaw, or epigastrium; shortness of breath; weakness; diaphoresis; nausea; lightheadedness) should be instructed to call 9-1-1 and should be transported to the hospital by ambulance rather than by friends or relatives. (Level of Evidence: B) 3. Health care providers should actively address the following issues regarding ACS with patients with or at risk for CHD and their families or other responsible caregivers:
4. Prehospital EMS providers should administer 162 to 325 mg of aspirin (ASA; chewed) to chest pain patients suspected of having ACS unless contraindicated or already taken by the patient. Although some trials have used enteric-coated ASA for initial dosing, more rapid buccal absorption occurs with non–enteric-coated formulations. (Level of Evidence: C) 5. Health care providers should instruct patients with suspected ACS for whom nitroglycerin (NTG) has been prescribed previously to take not more than 1 dose of NTG sublingually in response to chest discomfort/pain. If chest discomfort/pain is unimproved or is worsening 5 min after 1 NTG dose has been taken, it is recommended that the patient or family member/friend/caregiver call 9-1-1 immediately to access EMS before taking additional NTG. In patients with chronic stable angina, if symptoms are significantly improved by 1 dose of NTG, it is appropriate to instruct the patient or family member/friend/caregiver to repeat NTG every 5 min for a maximum of 3 doses and call 9-1-1 if symptoms have not resolved completely. (Level of Evidence: C) 6. Patients with a suspected ACS with chest discomfort or other ischemic symptoms at rest for greater than 20 min, hemodynamic instability, or recent syncope or presyncope should be referred immediately to an ED. Other patients with a suspected ACS who are experiencing less severe symptoms and who have none of the above high-risk features, including those who respond to an NTG dose, may be seen initially in an ED or an outpatient facility able to provide an acute evaluation. (Level of Evidence: C) Class IIa1. It is reasonable for health care providers and 9-1-1 dispatchers to advise patients without a history of ASA allergy who have symptoms of ACS to chew ASA (162 to 325 mg) while awaiting arrival of prehospital EMS providers. Although some trials have used enteric- coated ASA for initial dosing, more rapid buccal absorption occurs with non–enteric-coated formulations. (Level of Evidence: B) 2. It is reasonable for health care providers and 9-1-1 dispatchers to advise patients who tolerate NTG to repeat NTG every 5 min for a maximum of 3 doses while awaiting ambulance arrival. (Level of Evidence: C) 3. It is reasonable that all prehospital EMS providers perform and evaluate 12-lead electrocardiograms (ECGs) in the field (if available) on chest pain patients suspected of ACS to assist in triage decisions. Electrocardiographs with validated computer-generated interpretation algorithms are recommended for this purpose. (Level of Evidence: B) 4. If the 12-lead ECG shows evidence of acute injury or ischemia, it is reasonable that prehospital ACLS providers relay the ECG to a predetermined medical control facility and/or receiving hospital. (Level of Evidence: B) |
” |
See Also
- The UA / NSTEMI Living Guidelines: Vote on current recommendations and suggest revisions to the guidelines
- The Living Guidelines: UA/NSTEMI
- Chronic stable angina
- Non ST Elevation Myocardial Infarction
- ST Elevation Myocardial Infarction
Sources
- The ACC/AHA 2007 Guidelines for the Management of Patients With Unstable Angina/Non-ST-Elevation Myocardial Infarction [1]
References
- ↑ 1.0 1.1 1.2 Anderson JL, Adams CD, Antman EM; et al. (2007). "ACC/AHA 2007 guidelines for the management of patients with unstable angina/non-ST-Elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines for the Management of Patients With Unstable Angina/Non-ST-Elevation Myocardial Infarction) developed in collaboration with the American College of Emergency Physicians, the Society for Cardiovascular Angiography and Interventions, and the Society of Thoracic Surgeons endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation and the Society for Academic Emergency Medicine". JACC. 50 (7): e1–e157. PMID 17692738. Text "doi:10.1016/j.jacc.2007.02.013 " ignored (help); Unknown parameter
|month=ignored (help)