Tuberculosis historical perspective: Difference between revisions
Joao Silva (talk | contribs) No edit summary |
Mohamed riad (talk | contribs) |
||
| (12 intermediate revisions by 5 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{Tuberculosis}} | {{Tuberculosis}} | ||
{{CMG}}; {{AE}} | {{CMG}}; {{AE}} {{Mashal Awais}}; {{JS}} | ||
==Overview== | ==Overview== | ||
[[Tuberculosis]] has been | [[Tuberculosis]] has been detected for a long time. The earliest unambiguous detection of ''[[Mycobacterium tuberculosis]]'' was in the remains of [[bison]], dated 18,000 BC.<ref name="Rothschild_2001">{{cite journal |author=Rothschild B, Martin L, Lev G, Bercovier H, Bar-Gal G, Greenblatt C, Donoghue H, Spigelman M, Brittain D |title=Mycobacterium tuberculosis complex DNA from an extinct bison dated 17,000 years before the present |journal=Clin Infect Dis |volume=33 |issue=3 |pages=305-11 |year=2001 | pmid = 11438894}}</ref> However, whether [[tuberculosis]] originated in [[cattle]] and then transferred to humans, or [[diverged]] from a [[common]] [[ancestor]], is unclear.<ref name="Pearce-Duvet_2006">{{cite journal |author=Pearce-Duvet J |title=The origin of human pathogens: evaluating the role of agriculture and domestic animals in the evolution of human disease |journal=Biol Rev Camb Philos Soc |volume=81 |issue=3 |pages=369-82 |year=2006 | pmid = 16672105}}</ref> Through history [[tuberculosis]] has had many names including ''[[Tuberculosis|phthisis]]'' and ''[[Wasting disease]]'', which were mostly derived from its [[symptoms]]. [[Robert Koch]] identified the ''[[Mycobacterium tuberculosis]]'' 1882. In the 19th and early 20th centuries, [[tuberculosis]] was considered an endemic disease of the urban poor and a public healthcare issue. In 1946, the development of the [[antibiotic]] [[streptomycin]] made the cure possible. In the 1980s, the [[Antibiotic resistant|drug-resistant]] strains appeared increasingly eliminating the hope of cure. | ||
==Historical Perspective== | ==Historical Perspective== | ||
[[Image:TB history 1.png|left|thumb| | [[Image:TB history 1.png|left|thumb|400px|Tubercular decay has been found in the spines of Egyptian mummies. Pictured: Egyptian mummy in the British Museum<SMALL><SMALL>''[http://commons.wikimedia.org/wiki/File:Mummy_at_British_Museum.jpg Adapted from Wikimedia Commons]''<ref name="Wikimedia Commons">{{Cite web | title = Wikimedia Commons | url = http://commons.wikimedia.org/wiki/File:Mummy_at_British_Museum.jpg}}</ref></SMALL></SMALL>]] | ||
TB was present in prehistoric humans and the evidence of infection was found in the skeletal remains 4000 BC, in addition to the spines of mummies showing tubercular decay from 3000-2400 BC.<ref name="Zink_2003">{{cite journal |author=Zink A, Sola C, Reischl U, Grabner W, Rastogi N, Wolf H, Nerlich A |title=Characterization of Mycobacterium tuberculosis complex DNAs from Egyptian mummies by spoligotyping |journal=J Clin Microbiol |volume=41 |issue=1 |pages=359-67 |year=2003 | pmid = 12517873}}</ref> Phthisis is a Greek term for [[tuberculosis]]; around 460 BC. In terms of Hippocrates point of view, phthisis was the most widespread disease of the time involving fever and coughing up blood, which was almost always fatal.<ref>Hippocrates. [http://web.archive.org/web/20050211173218/http://classics.mit.edu/Hippocrates/aphorisms.mb.txt Aphorisms.] Accessed 07 October 2006.</ref> TB was present in South America for about 2,000 years evidenced by some genetic studies.<ref name="Konomi_2002">{{cite journal |author=Konomi N, Lebwohl E, Mowbray K, Tattersall I, Zhang D |title=Detection of mycobacterial DNA in Andean mummies |journal=J Clin Microbiol |volume=40 |issue=12 |pages=4738–40 |year=2002 | pmid = 12454182}}</ref> In South America, the earliest evidence of [[tuberculosis]] was linked to the Paracas-Caverna culture (circa 750 BC to circa 100 AD).<ref>[http://memorias.ioc.fiocruz.br/98sup/6psa.html "South America: Prehistoric Findings"]. ''Memorias do Instituto Oswaldo Cruz'', Vol. 98 (Suppl.I) January 2003. Retrieved on [[2007-02-08]].</ref> | |||
In the | Egyptian mummies, that dates back to 2400 BC, showed skeletal deformities characteristic of tuberculosis of spine (Pott's lesions) and those findings were documented clearly in early Egyptian art.<ref name="pmid14221665">{{cite journal| author=MORSE D, BROTHWELL DR, UCKO PJ| title=TUBERCULOSIS IN ANCIENT EGYPT. | journal=Am Rev Respir Dis | year= 1964 | volume= 90 | issue= | pages= 524-41 | pmid=14221665 | doi=10.1164/arrd.1964.90.4.524 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=14221665 }}</ref> | ||
* ''Phthisis'' (Greek for consumption) | |||
* ''Phthisis pulmonalis'' | In the Ancient Greece TB was identified and named Phtisis. Hippocrates recognized it as a [[Mortality rate|fatal]] disease especially for young adults. Isocrates was the first to suggest that [[Tuberculosis|TB]] is considered an [[Infection|infectious]] disease, while Aristotle suggested its [[Infectious disease|contagious]] in oxes and pigs.<ref name="pmid285156262">{{cite journal| author=Barberis I, Bragazzi NL, Galluzzo L, Martini M| title=The history of tuberculosis: from the first historical records to the isolation of Koch's bacillus. | journal=J Prev Med Hyg | year= 2017 | volume= 58 | issue= 1 | pages= E9-E12 | pmid=28515626 | doi= | pmc=5432783 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28515626 }}</ref> | ||
* ''[[Scrofula]]'' (in adults) - | |||
* ''Tabes mesenterica'' - [[TB]] of the [[abdomen]] | Along time ago, Since tuberculosis was similar to the idea of consumption of the infected patients with [[fever]], [[hemoptysis]], [[pallor]], and severe [[wasting]], [[tuberculosis]] was called [[consumption]]. Other names are:<ref name="Britannica1911">[http://www.1911encyclopedia.org/Tuberculosis Tuberculosis] ''Encyclopedia Britannica,'' 11th ed.</ref><ref>[http://www.antiquusmorbus.com/English/English.htm Rudy's List of Archaic Medical Terms] English Glossary of Archaic Medical Terms, Diseases and Causes of Death. Accessed 09 Oct 06</ref><ref name="Britannica1911" /><ref>[http://www.nlm.nih.gov/medlineplus/ency/article/000624.htm Disseminated tuberculosis] NIH Medical Encyclopedia. Accessed 09 Oct 06</ref> | ||
* ''[[Lupus vulgaris]]'' - [[TB]] of the [[skin]] | |||
* ''Wasting disease'' | *''Phthisis'' (Greek for consumption) | ||
* ''White plague'' - | *''Phthisis pulmonalis'' | ||
* ''King's evil'' - | *''[[Scrofula]]'' (in adults) - TB of the lymphatic system, resulting in [[Swelling|swollen]] [[cervical]] [[Lymph node|lymph nodes]] | ||
* ''[[Pott's disease]]'' | *''Tabes [[mesenterica]]'' - [[TB]] of the [[abdomen]] | ||
* [[Miliary tuberculosis]] – | *''[[Lupus vulgaris]]'' - [[TB]] of the [[skin]] | ||
*''Wasting disease'' | |||
*''White [[plague]]'' - due to [[paleness]] of the sufferers | |||
*''King's evil'' - as people had a false belief that that scrofula would heal by the king’s touch | |||
*''[[Pott's disease]]'' - TB of the [[spine]] | |||
*[[Miliary tuberculosis]] – also called ''[[disseminated TB]]'', occurs when the [[infection]] spreads in the [[blood]] stream, resulting in lesions in multiple [[Organ (anatomy)|organs]] with the [[appearance]] of millet [[seeds]] on [[x-ray]]. | |||
===Folklore=== | ===Folklore=== | ||
[[tuberculosis]] was sometimes considered as as vampirism before the industrial revolution. When one family member died from it, the other members became infected and died slowly. People had a false belief that this occurs because the first victim drains the life from the other family members. Moreover, people who had [[TB]] had [[symptoms]] such as red, swollen [[red eye|eyes]] (which also causes [[photosensitivity]]), pale [[skin]] and [[coughing blood|hemoptysis]] that are similar to what people knew about vampires. This suggested the idea that the only way for the afflicted to replenish this loss of [[blood]] was by sucking [[blood]].<ref name="Sledzik_1994">{{cite journal |author=Sledzik P, Bellantoni N |title=Brief communication: bioarcheological and biocultural evidence for the New England vampire folk belief |journal=Am J Phys Anthropol |volume=94 |issue=2 |pages=269-74 |year=1994 |url=http://users.net1plus.com/vyrdolak/tableone.htm | pmid = 8085617}}</ref> people also attributed it to being forced, nightly, to attend fairy revels, so that the victim wasted away due to lack of rest.<ref name="Briggs">[[Katharine Mary Briggs|Katharine Briggs]], ''An Encyclopedia of Fairies'' "Consumption" ([[Pantheon Books]], 1976) p. 80. ISBN 0-394-73467-X</ref> Similarly, but rarely, it was attributed to the victims being 'hagridden' - being transformed into horses by witches (hags) to travel to their nightly meetings leading to [[Lack (manque)|lack]] of rest.<ref name="Briggs" /> | |||
In the 19th century. Many people believed [[TB]] caused a [[sensation]] of [[euphoria]] called <nowiki>''Spes phthisica'' or ''hope of the consumptive''</nowiki>. It was believed that artists affected with [[Tuberculosis|TB]] had bursts of creativity with TB [[progression]]. It was also believed that [[TB]] sufferers were having a final burst of [[energy]] just before their [[death]] that made women more beautiful and men more creative.<ref name="StudiesLiteraryImagination-Clark">Lawlor, Clark. "Transatlantic Consumptions: Disease, Fame and Literary Nationalism in the Davidson Sisters, Southey, and Poe". ''Studies in the Literary Imagination'', Fall 2003. Available at [http://findarticles.com/p/articles/mi_qa3822/is_200310/ai_n9310101 findarticles.com.] Retrieved on [[2007-06-08]].</ref> | |||
===Study and Treatment=== | ===Study and Treatment=== | ||
[[Image:TB history 2.png|left|thumb|200px|Dr. Robert Koch discovered the tuberculosis bacilli.<SMALL><SMALL>''[http://commons.wikimedia.org/wiki/File:RobertKoch.jpg Adapted from Wikimedia Commons]''<ref name="Wikimedia Commons">{{Cite web | title = Wikimedia Commons | url = http://commons.wikimedia.org/wiki/File:RobertKoch.jpg}}</ref></SMALL></SMALL>]]In 1020s, [[Avicenna|Ibn Sina]] (Avicenna), with his book ''[[The Canon of Medicine]],'' was the first physician to identify [[pulmonary tuberculosis]] as a [[Infectious disease|contagious disease]] and suggest that it could spread through contact with soil and [[water]].<ref>Y. A. Al-Sharrah (2003), "The Arab Tradition of Medical Education and its Relationship with the European Tradition", ''Prospects'' '''33''' (4), [[Springer Science+Business Media|Springer]].</ref><ref>[[George Sarton]], ''Introduction to the History of Science''. <br> ([[cf.]] Dr. A. Zahoor and Dr. Z. Haq (1997). [http://www.cyberistan.org/islamic/Introl1.html Quotations From Famous Historians of Science], Cyberistan.)</ref> He developed the method of [[quarantine]] to reduce the spread of [[tuberculosis]].<ref>David W. Tschanz, MSPH, PhD (August 2003). "Arab Roots of European Medicine", ''Heart Views'' '''4''' (2).</ref> | |||
Although | Although [[Dr Richard Morton]] established that the [[pulmonary]] form was associated with 'tubercles' in 1689,<ref name="WhoNamedIt-Calmette">Who Named It? [http://www.whonamedit.com/doctor.cfm/2413.html Léon Charles Albert Calmette.] Retrieved on 6 October 2006.</ref><ref name="MedHist1970-Trail">{{cite journal |author=Trail R |title=Richard Morton (1637–1698) |journal=Med Hist |volume=14 |issue=2 |pages=166-74 |year=1970 | pmid = 4914685}}</ref> due to the variation of its [[symptoms]], [[TB]] was not identified as a single disease until the 1820s and was not named '[[tuberculosis]]' until 1839 by [[Johann Lukas Schönlein|J. L. Schönlein]].<ref>Zur Pathogenie der Impetigines. Auszug aus einer brieflichen Mitteilung an den Herausgeber. [Müller’s] ''Archiv für Anatomie, Physiologie und wissenschaftliche Medicin''. 1839, page 82.</ref> During the years 1838-1845, Dr. John Croghan, the owner of Mammoth Cave, brought some [[tuberculosis]] sufferers into the cave to treat them with the constant temperature and purity of the cave air; however, they died within a year.<ref>[http://edition.cnn.com/2004/TRAVEL/DESTINATIONS/02/26/mammoth.cave.ap/index.html Kentucky: Mammoth Cave long on history.] ''[[CNN]]''. 27 February 2004. Accessed 08 October 2006.</ref> The first [[TB]] [[sanatorium]] opened in 1859 in Görbersdorf, Germany (today Sokołowsko, Poland) by Hermann Brehmer.<ref name="sanatoria">{{cite journal |author=McCarthy OR |title=The key to the sanatoria |journal=J R Soc Med |volume=94 |issue=8 |pages=413-7 |year=2001 | pmid = 11461990}}</ref> | ||
Hermann Lebert published his project ''Traite Pratique des Maladies Scrofuleuses et Tuberculeuses in 1849'', reporting that the [[Tuberculosis|TB]] or "King's evil" was a childhood disease that can affect multiple body's sites such as [[skin]], [[Eye|eyes]], [[Ear|ears]], [[Joint|joints]], and [[bones]], causing [[Ulcer|ulceration]] and [[Pus|suppuration]].<ref name="pmid28515626">{{cite journal| author=Barberis I, Bragazzi NL, Galluzzo L, Martini M| title=The history of tuberculosis: from the first historical records to the isolation of Koch's bacillus. | journal=J Prev Med Hyg | year= 2017 | volume= 58 | issue= 1 | pages= E9-E12 | pmid=28515626 | doi= | pmc=5432783 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28515626 }}</ref> | |||
[[Robert Koch]] identified and deascribed the [[bacillus]] causing [[tuberculosis]], ''[[Mycobacterium tuberculosis]]'', on March 24, 1882 for which He received the [[Nobel Prize in physiology or medicine]] in 1905.<ref>[[Nobel Foundation]]. [http://nobelprize.org/nobel_prizes/medicine/laureates/1905/ The Nobel Prize in Physiology or Medicine 1905.] Accessed 07 October 2006.</ref> Koch did not identify that bovine (cattle) and human [[tuberculosis]] were the same infection, which delayed considering [[infected]] milk as a source of [[infection]]. Later on, this source was eliminated by the process of milk [[pasteurization]]. Koch identified a [[glycerine]] extract of the tubercle [[bacilli]] as in 1890, calling it 'tuberculin'. It was not accurate, but was later adapted as a test for pre-symptomatic [[tuberculosis]].<ref name="Waddington_2004">{{cite journal |author=Waddington K |title=To stamp out "so terrible a malady": bovine tuberculosis and tuberculin testing in Britain, 1890–1939 |journal=Med Hist |volume=48 |issue=1 |pages=29–48 |year=2004 | pmid = 14968644}}</ref> | |||
[[Tuberculosis]], or 'consumption' | The first achievement in [[tuberculosis]] [[immunization]] was 'BCG' ([[Bacillus Calmette-Guérin|Bacillus of Calmette and Guerin]]) that was developed from attenuated bovine-strain [[tuberculosis]] by [[Albert Calmette]] and [[Camille Guerin]] in 1906. The [[BCG vaccine]] was first used on humans in 1921 in France, and after World War II, [[BCG]] received approval in the USA, Great Britain, and Germany. | ||
[[Image:TB history 3.png|left|thumb|200px|Public health campaigns tried to halt the spread of TB<SMALL><SMALL>''[http://commons.wikimedia.org/wiki/File:TB_poster.jpg | |||
[[Tuberculosis]], or 'consumption' was considered an [[Endemic (epidemiology)|endemic]] disease of the urban poor and a public [[Health care|healthcare]] issue. In 1815, one in four deaths in England was of consumption; by 1918 one in six [[deaths]] in France were still caused by [[TB]]. In the 20th century, the number of deaths due to TB was 100 million people.<ref>[http://birdflubook.com/a.php?id=40&t=p Torrey EF and Yolken RH. 2005. Their bugs are worse than their bite. Washington Post, April 3, p. B01.]</ref> After the establishment in the 1880s that the disease was [[contagious]], [[TB]] was reported as a [[List of notifiable diseases|notifiable disease]] in Britain.<ref name="sanatoria" /> | |||
[[Image:TB history 3.png|left|thumb|200px|Public health campaigns tried to halt the spread of TB<SMALL><SMALL>''[http://commons.wikimedia.org/wiki/File:TB_poster.jpg Adapted from Wikimedia Commons]''<ref name="Wikimedia Commons">{{Cite web | title = Wikimedia Commons | url = http://commons.wikimedia.org/wiki/File:TB_poster.jpg}}</ref></SMALL></SMALL>]] | |||
In the United States, concern about the spread of [[tuberculosis]] played a role in the movement to prohibit public spitting except into [[spittoon]]s. | In the United States, concern about the spread of [[tuberculosis]] played a role in the movement to prohibit public spitting except into [[spittoon]]s. | ||
In Europe, deaths from [[TB]] | In Europe, deaths from [[TB]] decreased from 500 out of 100,000 in 1850 to 50 out of 100,000 by 1950. [[public health]] [[improvements]] had an impact regarding decreasing [[tuberculosis]] cases even before the development of [[antibiotics]], but the disease was still representing a significant harm to [[public health]].<ref>[[Medical Research Council (UK)|]]. [http://www.mrc.ac.uk/YourHealth/StoriesDiscovery/Tuberculosis/index.htm MRC's contribution to Tuberculosis research.] Accessed 02 July 2007.</ref> | ||
In 1946, the development of the [[antibiotic]] [[streptomycin]] made the cure possible. Before the discovery of this drug, the only [[treatment]] besides [[sanatorium|sanatoria]] were [[surgical]] [[interventions]], such as the [[pneumothorax]] [[technique]] - in the form of collapsing an [[infected]] [[lung]] to rest it and allow lesions to heal - which was of little benefit and was largely stopped by the 1950s.<ref name="Wolfart_1990">{{cite journal |author=Wolfart W |title=[Surgical treatment of tuberculosis and its modifications—collapse therapy and resection treatment and their present-day sequelae] |journal=Offentl Gesundheitswes |volume=52 |issue=8–9 |pages=506-11 |year=1990 | pmid = 2146567}}</ref> The emergence of [[multidrug-resistant TB]] has again introduced surgery as part of the [[treatment]] for these [[infections]]. Here, [[surgical]] removal of [[lung]] [[Cavity|cavities]] will reduce the number of [[bacteria]] in the [[lungs]], as well as increase the exposure of the remaining [[bacteria]] to drugs in the [[bloodstream]], which is thought to increase the [[effectiveness]] of the [[chemotherapy]].<ref name="Lalloo_2006">{{cite journal |author=Lalloo U, Naidoo R, Ambaram A |title=Recent advances in the medical and surgical treatment of multi-drug resistant tuberculosis |journal=Curr Opin Pulm Med |volume=12 |issue=3 |pages=179-85 |year=2006 | pmid = 16582672}}</ref> | |||
In the 1980s, the [[Antibiotic resistant|drug-resistant]] strains appeared increasingly eliminating the hope of [[cure]]. For example, [[tuberculosis]] cases in Britain, numbering around 117,000 in 1913, had fallen to around 5,000 in 1987, but cases increased again, reaching 6,300 in 2000 and 7,600 cases in 2005.<ref>{{cite web | url =http://www.hpa.org.uk/infections/topics_AZ/tb/epidemiology/table1.htm | title = Tuberculosis – Respiratory and Non-respiratory Notifications, England and Wales, 1913-2005 | publisher = Health Protection Agency Centre for Infections | date = 21 March 2007 | accessdate = 2007-08-01}}</ref> As a result of the [[Elimination communication|elimination]] of [[public health]] facilities in New York and the [[emergence]] of [[HIV]], there was another [[TB]] resurgence in the late 1980s.<ref name="Paolo_2004">{{cite journal |author=Paolo W, Nosanchuk J |title=Tuberculosis in New York city: recent lessons and a look ahead |journal=Lancet Infect Dis |volume=4 |issue=5 |pages=287-93 |year=2004 | pmid = 15120345}}</ref> <br clear="left" /> | |||
<br clear="left"/> | |||
==References== | ==References== | ||
{{reflist|2}} | {{reflist|2}} | ||
{{WH}} | |||
{{WS}} | |||
[[Category:Disease]] | [[Category:Disease]] | ||
[[Category: Pulmonology]] | |||
[[Category:Pulmonology]] | |||
[[Category:Bacterial diseases]] | [[Category:Bacterial diseases]] | ||
Latest revision as of 03:33, 24 February 2021
|
Tuberculosis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Tuberculosis historical perspective On the Web |
|
American Roentgen Ray Society Images of Tuberculosis historical perspective |
|
Risk calculators and risk factors for Tuberculosis historical perspective |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Mashal Awais, M.D.[2]; João André Alves Silva, M.D. [3]
Overview
Tuberculosis has been detected for a long time. The earliest unambiguous detection of Mycobacterium tuberculosis was in the remains of bison, dated 18,000 BC.[1] However, whether tuberculosis originated in cattle and then transferred to humans, or diverged from a common ancestor, is unclear.[2] Through history tuberculosis has had many names including phthisis and Wasting disease, which were mostly derived from its symptoms. Robert Koch identified the Mycobacterium tuberculosis 1882. In the 19th and early 20th centuries, tuberculosis was considered an endemic disease of the urban poor and a public healthcare issue. In 1946, the development of the antibiotic streptomycin made the cure possible. In the 1980s, the drug-resistant strains appeared increasingly eliminating the hope of cure.
Historical Perspective

TB was present in prehistoric humans and the evidence of infection was found in the skeletal remains 4000 BC, in addition to the spines of mummies showing tubercular decay from 3000-2400 BC.[4] Phthisis is a Greek term for tuberculosis; around 460 BC. In terms of Hippocrates point of view, phthisis was the most widespread disease of the time involving fever and coughing up blood, which was almost always fatal.[5] TB was present in South America for about 2,000 years evidenced by some genetic studies.[6] In South America, the earliest evidence of tuberculosis was linked to the Paracas-Caverna culture (circa 750 BC to circa 100 AD).[7]
Egyptian mummies, that dates back to 2400 BC, showed skeletal deformities characteristic of tuberculosis of spine (Pott's lesions) and those findings were documented clearly in early Egyptian art.[8]
In the Ancient Greece TB was identified and named Phtisis. Hippocrates recognized it as a fatal disease especially for young adults. Isocrates was the first to suggest that TB is considered an infectious disease, while Aristotle suggested its contagious in oxes and pigs.[9]
Along time ago, Since tuberculosis was similar to the idea of consumption of the infected patients with fever, hemoptysis, pallor, and severe wasting, tuberculosis was called consumption. Other names are:[10][11][10][12]
- Phthisis (Greek for consumption)
- Phthisis pulmonalis
- Scrofula (in adults) - TB of the lymphatic system, resulting in swollen cervical lymph nodes
- Tabes mesenterica - TB of the abdomen
- Lupus vulgaris - TB of the skin
- Wasting disease
- White plague - due to paleness of the sufferers
- King's evil - as people had a false belief that that scrofula would heal by the king’s touch
- Pott's disease - TB of the spine
- Miliary tuberculosis – also called disseminated TB, occurs when the infection spreads in the blood stream, resulting in lesions in multiple organs with the appearance of millet seeds on x-ray.
Folklore
tuberculosis was sometimes considered as as vampirism before the industrial revolution. When one family member died from it, the other members became infected and died slowly. People had a false belief that this occurs because the first victim drains the life from the other family members. Moreover, people who had TB had symptoms such as red, swollen eyes (which also causes photosensitivity), pale skin and hemoptysis that are similar to what people knew about vampires. This suggested the idea that the only way for the afflicted to replenish this loss of blood was by sucking blood.[13] people also attributed it to being forced, nightly, to attend fairy revels, so that the victim wasted away due to lack of rest.[14] Similarly, but rarely, it was attributed to the victims being 'hagridden' - being transformed into horses by witches (hags) to travel to their nightly meetings leading to lack of rest.[14]
In the 19th century. Many people believed TB caused a sensation of euphoria called ''Spes phthisica'' or ''hope of the consumptive''. It was believed that artists affected with TB had bursts of creativity with TB progression. It was also believed that TB sufferers were having a final burst of energy just before their death that made women more beautiful and men more creative.[15]
Study and Treatment

In 1020s, Ibn Sina (Avicenna), with his book The Canon of Medicine, was the first physician to identify pulmonary tuberculosis as a contagious disease and suggest that it could spread through contact with soil and water.[16][17] He developed the method of quarantine to reduce the spread of tuberculosis.[18]
Although Dr Richard Morton established that the pulmonary form was associated with 'tubercles' in 1689,[19][20] due to the variation of its symptoms, TB was not identified as a single disease until the 1820s and was not named 'tuberculosis' until 1839 by J. L. Schönlein.[21] During the years 1838-1845, Dr. John Croghan, the owner of Mammoth Cave, brought some tuberculosis sufferers into the cave to treat them with the constant temperature and purity of the cave air; however, they died within a year.[22] The first TB sanatorium opened in 1859 in Görbersdorf, Germany (today Sokołowsko, Poland) by Hermann Brehmer.[23]
Hermann Lebert published his project Traite Pratique des Maladies Scrofuleuses et Tuberculeuses in 1849, reporting that the TB or "King's evil" was a childhood disease that can affect multiple body's sites such as skin, eyes, ears, joints, and bones, causing ulceration and suppuration.[24]
Robert Koch identified and deascribed the bacillus causing tuberculosis, Mycobacterium tuberculosis, on March 24, 1882 for which He received the Nobel Prize in physiology or medicine in 1905.[25] Koch did not identify that bovine (cattle) and human tuberculosis were the same infection, which delayed considering infected milk as a source of infection. Later on, this source was eliminated by the process of milk pasteurization. Koch identified a glycerine extract of the tubercle bacilli as in 1890, calling it 'tuberculin'. It was not accurate, but was later adapted as a test for pre-symptomatic tuberculosis.[26]
The first achievement in tuberculosis immunization was 'BCG' (Bacillus of Calmette and Guerin) that was developed from attenuated bovine-strain tuberculosis by Albert Calmette and Camille Guerin in 1906. The BCG vaccine was first used on humans in 1921 in France, and after World War II, BCG received approval in the USA, Great Britain, and Germany.
Tuberculosis, or 'consumption' was considered an endemic disease of the urban poor and a public healthcare issue. In 1815, one in four deaths in England was of consumption; by 1918 one in six deaths in France were still caused by TB. In the 20th century, the number of deaths due to TB was 100 million people.[27] After the establishment in the 1880s that the disease was contagious, TB was reported as a notifiable disease in Britain.[23]
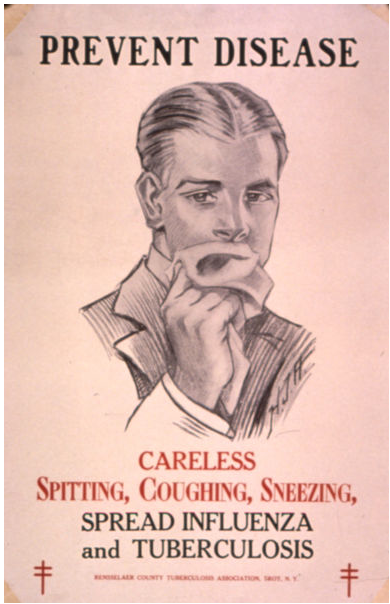
In the United States, concern about the spread of tuberculosis played a role in the movement to prohibit public spitting except into spittoons.
In Europe, deaths from TB decreased from 500 out of 100,000 in 1850 to 50 out of 100,000 by 1950. public health improvements had an impact regarding decreasing tuberculosis cases even before the development of antibiotics, but the disease was still representing a significant harm to public health.[28]
In 1946, the development of the antibiotic streptomycin made the cure possible. Before the discovery of this drug, the only treatment besides sanatoria were surgical interventions, such as the pneumothorax technique - in the form of collapsing an infected lung to rest it and allow lesions to heal - which was of little benefit and was largely stopped by the 1950s.[29] The emergence of multidrug-resistant TB has again introduced surgery as part of the treatment for these infections. Here, surgical removal of lung cavities will reduce the number of bacteria in the lungs, as well as increase the exposure of the remaining bacteria to drugs in the bloodstream, which is thought to increase the effectiveness of the chemotherapy.[30]
In the 1980s, the drug-resistant strains appeared increasingly eliminating the hope of cure. For example, tuberculosis cases in Britain, numbering around 117,000 in 1913, had fallen to around 5,000 in 1987, but cases increased again, reaching 6,300 in 2000 and 7,600 cases in 2005.[31] As a result of the elimination of public health facilities in New York and the emergence of HIV, there was another TB resurgence in the late 1980s.[32]
References
- ↑ Rothschild B, Martin L, Lev G, Bercovier H, Bar-Gal G, Greenblatt C, Donoghue H, Spigelman M, Brittain D (2001). "Mycobacterium tuberculosis complex DNA from an extinct bison dated 17,000 years before the present". Clin Infect Dis. 33 (3): 305–11. PMID 11438894.
- ↑ Pearce-Duvet J (2006). "The origin of human pathogens: evaluating the role of agriculture and domestic animals in the evolution of human disease". Biol Rev Camb Philos Soc. 81 (3): 369–82. PMID 16672105.
- ↑ 3.0 3.1 3.2 "Wikimedia Commons".
- ↑ Zink A, Sola C, Reischl U, Grabner W, Rastogi N, Wolf H, Nerlich A (2003). "Characterization of Mycobacterium tuberculosis complex DNAs from Egyptian mummies by spoligotyping". J Clin Microbiol. 41 (1): 359–67. PMID 12517873.
- ↑ Hippocrates. Aphorisms. Accessed 07 October 2006.
- ↑ Konomi N, Lebwohl E, Mowbray K, Tattersall I, Zhang D (2002). "Detection of mycobacterial DNA in Andean mummies". J Clin Microbiol. 40 (12): 4738–40. PMID 12454182.
- ↑ "South America: Prehistoric Findings". Memorias do Instituto Oswaldo Cruz, Vol. 98 (Suppl.I) January 2003. Retrieved on 2007-02-08.
- ↑ MORSE D, BROTHWELL DR, UCKO PJ (1964). "TUBERCULOSIS IN ANCIENT EGYPT". Am Rev Respir Dis. 90: 524–41. doi:10.1164/arrd.1964.90.4.524. PMID 14221665.
- ↑ Barberis I, Bragazzi NL, Galluzzo L, Martini M (2017). "The history of tuberculosis: from the first historical records to the isolation of Koch's bacillus". J Prev Med Hyg. 58 (1): E9–E12. PMC 5432783. PMID 28515626.
- ↑ 10.0 10.1 Tuberculosis Encyclopedia Britannica, 11th ed.
- ↑ Rudy's List of Archaic Medical Terms English Glossary of Archaic Medical Terms, Diseases and Causes of Death. Accessed 09 Oct 06
- ↑ Disseminated tuberculosis NIH Medical Encyclopedia. Accessed 09 Oct 06
- ↑ Sledzik P, Bellantoni N (1994). "Brief communication: bioarcheological and biocultural evidence for the New England vampire folk belief". Am J Phys Anthropol. 94 (2): 269–74. PMID 8085617.
- ↑ 14.0 14.1 Katharine Briggs, An Encyclopedia of Fairies "Consumption" (Pantheon Books, 1976) p. 80. ISBN 0-394-73467-X
- ↑ Lawlor, Clark. "Transatlantic Consumptions: Disease, Fame and Literary Nationalism in the Davidson Sisters, Southey, and Poe". Studies in the Literary Imagination, Fall 2003. Available at findarticles.com. Retrieved on 2007-06-08.
- ↑ Y. A. Al-Sharrah (2003), "The Arab Tradition of Medical Education and its Relationship with the European Tradition", Prospects 33 (4), Springer.
- ↑ George Sarton, Introduction to the History of Science.
(cf. Dr. A. Zahoor and Dr. Z. Haq (1997). Quotations From Famous Historians of Science, Cyberistan.) - ↑ David W. Tschanz, MSPH, PhD (August 2003). "Arab Roots of European Medicine", Heart Views 4 (2).
- ↑ Who Named It? Léon Charles Albert Calmette. Retrieved on 6 October 2006.
- ↑ Trail R (1970). "Richard Morton (1637–1698)". Med Hist. 14 (2): 166–74. PMID 4914685.
- ↑ Zur Pathogenie der Impetigines. Auszug aus einer brieflichen Mitteilung an den Herausgeber. [Müller’s] Archiv für Anatomie, Physiologie und wissenschaftliche Medicin. 1839, page 82.
- ↑ Kentucky: Mammoth Cave long on history. CNN. 27 February 2004. Accessed 08 October 2006.
- ↑ 23.0 23.1 McCarthy OR (2001). "The key to the sanatoria". J R Soc Med. 94 (8): 413–7. PMID 11461990.
- ↑ Barberis I, Bragazzi NL, Galluzzo L, Martini M (2017). "The history of tuberculosis: from the first historical records to the isolation of Koch's bacillus". J Prev Med Hyg. 58 (1): E9–E12. PMC 5432783. PMID 28515626.
- ↑ Nobel Foundation. The Nobel Prize in Physiology or Medicine 1905. Accessed 07 October 2006.
- ↑ Waddington K (2004). "To stamp out "so terrible a malady": bovine tuberculosis and tuberculin testing in Britain, 1890–1939". Med Hist. 48 (1): 29–48. PMID 14968644.
- ↑ Torrey EF and Yolken RH. 2005. Their bugs are worse than their bite. Washington Post, April 3, p. B01.
- ↑ [[Medical Research Council (UK)|]]. MRC's contribution to Tuberculosis research. Accessed 02 July 2007.
- ↑ Wolfart W (1990). "[Surgical treatment of tuberculosis and its modifications—collapse therapy and resection treatment and their present-day sequelae]". Offentl Gesundheitswes. 52 (8–9): 506–11. PMID 2146567.
- ↑ Lalloo U, Naidoo R, Ambaram A (2006). "Recent advances in the medical and surgical treatment of multi-drug resistant tuberculosis". Curr Opin Pulm Med. 12 (3): 179–85. PMID 16582672.
- ↑ "Tuberculosis – Respiratory and Non-respiratory Notifications, England and Wales, 1913-2005". Health Protection Agency Centre for Infections. 21 March 2007. Retrieved 2007-08-01.
- ↑ Paolo W, Nosanchuk J (2004). "Tuberculosis in New York city: recent lessons and a look ahead". Lancet Infect Dis. 4 (5): 287–93. PMID 15120345.