Tibial plateau fracture pathophysiology
|
Tibial plateau fracture Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Tibial plateau fracture pathophysiology On the Web |
|
American Roentgen Ray Society Images of Tibial plateau fracture pathophysiology |
|
Risk calculators and risk factors for Tibial plateau fracture pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Rohan A. Bhimani, M.B.B.S., D.N.B., M.Ch.[2]
Overview
Pathophysiology
- The fracture pattern and severity of comminution depends on multiple factors including:[1]
- Decrease in bone mass density involves following process:[2]
- Autophagy is the mechanism through which osteocytes evade oxidative stress.
- The capability of autophagy in cells decreases as they age, a major factor of aging.
- As osteocytes grow, viability of cells decrease thereby decreasing the bone mass density.
Anatomy
 |
- Majority of the weight in the lower leg is transmitted through tibia.[3][4]
- The tibial plateau is the proximal portion of the tibia and forms the part of the knee joint.
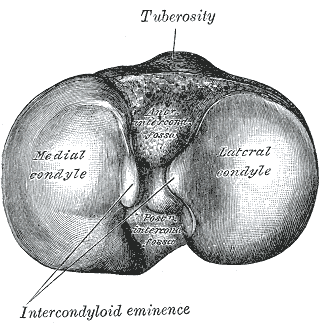
- The stronger of the two articular surfaces is the medial tibial condyle whereas the lateral tibial condyle is a weaker portion of the joint.
- The medial from the lateral tibial condyle are separated by the intercondylar eminence which serves as the attachment for the anterior cruciate ligament (ACL).
Medial Condyle
- The medial condyle is larger than the lateral condyle.
- The articular surface of medial condyle is oval and it is long axis is anteroposterior.
- The central part of the medial condylar surface is slightly concave.
- The peripheral part is falt and seperated from femoral condyle by the medial meniscus.
Lateral Condyle
- The lateral condyle overhangs the shaft of tibia.
- The articular surface is nearly circular.
- The central part is slightly concave and comes in direct contact with femoral condyle.
- The peripheral part is flat and seperated from femur by the lateral meniscus.
Mechanism of Fracture
- Proximal tibial injuries can occur due to direct trauma or indirect mechanisms such as axial compression.[5]
- The causes of most tibial plateau fractures are a valgus stress associated with an axial load.
- Most tibial plateau fractures result from motor vehicle-related injuries followed by sports-associated injuries.
- The bumper of a car striking the lateral plateau during this vehicle–pedestrian-related injury causes a valgus mechanism of injury.
- Motor vehicle injuries are high energy and often result in splitting types of fractures as well as direct injury to the surrounding soft tissues.
- Low-energy forces can cause a tibial plateau fracture usually in older patients with poor bone quality due to rotational forces.
- Such injuries are primarily seen in women >50 years with osteoporosis resulting in a depressed pattern plateau fracture.
References
- ↑ Azar, Frederick (2017). Campbell's operative orthopaedics. Philadelphia, PA: Elsevier. ISBN 9780323374620.
- ↑ Onal M, Piemontese M, Xiong J, Wang Y, Han L, Ye S; et al. (2013). "Suppression of autophagy in osteocytes mimics skeletal aging". J Biol Chem. 288 (24): 17432–40. doi:10.1074/jbc.M112.444190. PMC 3682543. PMID 23645674.
- ↑ Rockwood, Charles (2010). Rockwood and Green's fractures in adults. Philadelphia, PA: Wolters Kluwer Health/Lippincott Williams & Wilkins. ISBN 9781605476773.
- ↑ Azar, Frederick (2017). Campbell's operative orthopaedics. Philadelphia, PA: Elsevier. ISBN 9780323374620.
- ↑ Ramponi DR, McSwigan T (2018). "Tibial Plateau Fractures". Adv Emerg Nurs J. 40 (3): 155–161. doi:10.1097/TME.0000000000000194. PMID 30059369.